1. Context
A urinary tract infection (UTI) is a type of infection that can occur in any part of the urinary system, including the kidneys, bladder, and urethra. Among children, it is a commonly seen infectious disease after viral influenza and affects boys and girls equally (1). The primary treatment for UTIs involves antibiotics, which are selected based on established guidelines (2). Various factors, such as the severity of the infection (whether it is complicated or uncomplicated) and the resistance patterns of the pathogens, play a role in determining treatment plans and choosing antibiotics for each patient. However, besides these approaches, certain complementary therapies have shown potential in boosting the system and aiding faster healing.
The effectiveness of the immune system primarily depends on the health status. Among the available supplements, vitamins hold significant importance as essential nutrients for maintaining human health. Unfortunately, their therapeutic potential often goes unnoticed. In reality, vitamins can be used to treat and prevent diseases in both adults and children (3). However, misinformation in this field can result in crediting the advantages of these supplements and missing the adverse effects (4).
Hence, it is vital to determine if these nutritional supplements can truly aid in the management of illnesses. As a result, our main goal was to investigate the scientific studies regarding vitamin supplements and UTIs.
2. Evidence Acquisition
A systematic literature search was carried out using both PubMed and Google Scholar from January 1950 to December 2022. The following MeSH terms were used for the search: 'Urinary Tract Infections', 'Children', 'Vitamin A', 'Vitamin B Complex', 'Vitamin B 6', 'Vitamin B 1', 'Thiamine', 'Vitamin B 2', 'Riboflavin', 'Vitamin B 3', 'Niacinamide', 'Vitamin B 6', 'Vitamin B 12' 'Ascorbic Acid', 'Vitamin E', 'Vitamin D', and 'Vitamin K'.
All original articles, clinical trials, review articles, and case reports between January 1950 and December 2022 were included. Conference abstracts and non-English literature were excluded.
3. Results
3.1. Vitamin A
3.1.1. Introduction
The significant role played by vitamin A has been acknowledged for a considerable time. In fact, since 1928, this vitamin has been recognized as an anti-infective vitamin (5, 6). Conversely, vitamin A also serves as a growth factor similar to a hormone and takes part in the re-epithelialization of mucosal tissue (7).
3.1.2. The Role of Vitamin A in Infections
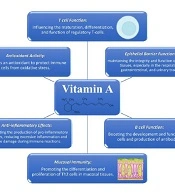
Vitamin A has been found to play crucial roles in the immune system, such as T cell function, antioxidant activity, and anti-inflammatory effects (8-13). The molecular mechanisms of the role of vitamin A in the immune system are summarized in Figure 1. Vitamin A deficiency presents symptoms similar to those found in immune system disorders, as it can result in pathological alterations in the mucosal tissue, reduced antibody responses, and impaired functioning of B- and T-cells (14). The recommendations for vitamin A supplementation mainly pertain to developing countries, where vitamin A deficiency is a prevalent public health concern (15). Moreover, the supplementation of vitamin A is linked to decreased mortality and morbidity rates caused by different infections, such as measles and respiratory infections (16).
3.1.3. Vitamin A and UTI
Research on the impact of vitamin A on UTIs has primarily focused on its ability to minimize renal scarring. Initial animal studies indicate that lower levels of vitamin A in the blood are associated with a greater incidence of renal scarring following UTI in rat models (17). This could be attributed to the therapeutic effect of vitamin A on the regeneration of mucosal tissue. On the other hand, certain animal studies not only failed to demonstrate the efficacy of vitamin A in reducing renal damage but also indicated that high doses of vitamin A were linked to more severe tissue damage (18). Nonetheless, human studies have shown promising results thus far. Some articles have reported that vitamin A supplements effectively reduce renal scarring in children with acute pyelonephritis (7, 19).
A meta-analysis conducted by Zhang et al. examined the effects of vitamin A supplements on renal damage using data from four randomized clinical trials (RCTs) involving 248 children. The findings confirmed that compared to the placebo group, vitamin A supplementation reduced renal damage (20). However, the authors emphasized the need for future RCTs of higher quality. Table 1 provides an overview of the RCTs investigating the association between vitamin A supplementation and renal scarring.
| Variables | ||||
|---|---|---|---|---|
| Author | Dalirani et al. (7) | Ayazi et al. (19) | Sobouti et al. (21) | Kahbazi et al. (22) |
| Method | Single-blinded randomized clinical trial | Single-blinded randomized clinical trial | Simple non-blind, open-label randomized clinical trial | Randomized, double-blind, placebo-controlled clinical trial |
| Year | 2011 | 2011 | 2013 | 2018 |
| Country | Tehran, Iran | Qazvin, Iran | Tehran, Iran | Arak, Iran |
| Number of participants (case/control) | 76 (37/39) | 50 (25/25) | 40 (20/20) | 74 (36/38) |
| Antibiotic treatment | Intravenous ceftriaxone 75 mg/kg for 10 days | Intravenous ceftriaxone 75 mg/kg twice a day for 10 days, followed by oral cephalexin (15 mg/kg) | According to the antibiogram profile, cephalothin or ampicillin (100 mg/kg/day 4 times daily) and amikacin (15 mg/kg/day 3times daily) for 10 days | Intravenous ceftriaxone 75 mg/kg/d followed by oral cephalexin (15 mg/kg) for 10 days. |
| Vitamin A treatment b | ||||
| Duration | First 3 days of admission | During admission | 10 days | 10 days |
| Route | Intramuscular | Intramuscular | Oral | Oral |
| Placebo | None | None | None | Once daily for 10 days |
| Follow-up time, mo | 6 | 3 | 6 | 6 |
Randomized Clinical Trials Evaluating the Association of Vitamin A Supplementation and Renal Scarring Following Acute Pyelonephritis in Pediatric Patients a
In 2019, Kahbazi et al. conducted an RCT which revealed that vitamin A supplementation in children was effective not only in reducing renal scarring after acute pyelonephritis but also in improving fever, frequency of urination, and poor nutrition in UTI patients (22). Another study by Yilmaz et al. also demonstrated that the administration of vitamin A in children with recurrent UTIs could potentially enhance treatment outcomes and decrease the frequency of recurrences (23). However, there is a paucity of articles exploring the role of this vitamin in the clinical manifestations and treatment of UTI.
3.2. Vitamin C
3.2.1. Introduction
Many years ago, scientific research unveiled the significance of vitamin C, also known as ascorbic acid, in mediating the immune system, particularly immune cell function (24). This essential nutrient cannot be produced by the human body (25). However, a daily intake of 100-200 mg of ascorbic acid is enough to fulfill our basic requirements and lower the likelihood of developing chronic illnesses (26). Inadequate vitamin C levels are linked to weakened immunity and a higher susceptibility to infections, and supplementing with this vitamin can aid in the prevention and treatment of infections (27).
3.2.2. The Role of Vitamin C in Infections
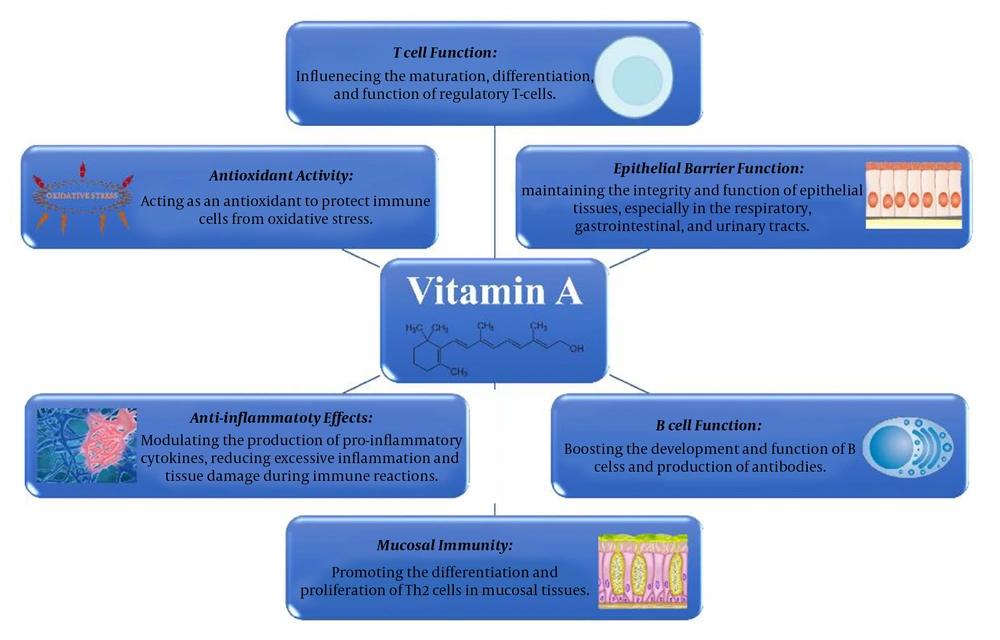
Ascorbic acid plays its role in the immune system in several ways, such as collagen synthesis, antioxidant activity, and production of pro-inflammatory cytokines (28-33). The roles of vitamin C in the immune system are summarized in Figure 2. Moreover, it possesses distinctive attributes specifically beneficial for UTIs. It has long been recognized that the abundant vitamin C excreted in urine can acidify it, thus diminishing bacterial proliferation (34).
3.2.3. Vitamin C and UTI
Previous research, including review articles and meta-analyses (35, 36), has confirmed the effectiveness of ascorbic acid supplementation in treating certain infections. Keya et al. specifically investigated its effects on respiratory tract infections and observed a decrease in illness duration (27).
For adults, vitamin C is often recommended as a preventive measure against recurring UTIs (37). In an RCT conducted in 2018, we examined the impact of vitamin C supplementation on children diagnosed with febrile upper UTI. Our findings revealed that it can help alleviate symptoms such as fever, dysuria, urinary urgency, and urinary dribbling. However, there was no observed effect on abdominal pain or recurrent UTIs (38). It is important to note that there is a lack of evidence in this area.
Some studies have explored the benefits of vitamin C-rich fruits such as cranberries in preventing UTIs. Meta-analyses have demonstrated their potential to reduce the risk and incidence of UTIs when consumed in the extract form (39-41).
3.3. Vitamin D
3.3.1. Introduction
Vitamin D is well-known for its role in regulating calcium and phosphorus levels. Interestingly, recent studies have brought attention to the immunomodulatory effects of vitamin D on both innate and adaptive immune systems. Although vitamin D is synthesized in the skin through exposure to ultraviolet (UV) light, vitamin D deficiency or insufficiency has become a global problem in recent years. In fact, in certain regions, the prevalence of vitamin D deficiency is reported to be as high as 68% (42).
Although there are currently no universally established guidelines for vitamin D supplementation, several recommendations suggest a daily intake of 400 IU for infants under the age of 1 year and 600 IU for older children (43). It is worth noting that low levels of vitamin D are associated with not only decreased bone density but also various comorbidities in pediatrics (44, 45).
3.3.2. The Role of Vitamin D in Infections
Numerous studies have indicated a correlation between low blood levels of vitamin D and different infections (46, 47). Consequently, several articles have identified vitamin D deficiency as an independent risk factor for UTIs (48, 49). In a systematic review and subgroup analysis conducted by Deng et al., significantly lower vitamin D levels were found in children with UTIs compared to the control group (50).
Various mechanisms have been proposed to explain the effects of vitamin D on UTIs. It is suggested that it improves the tight junctions of the urinary tract epithelium, thereby reducing the invasion of bacteria (51). Based on another mechanism, vitamin D enhances the local immune response, thereby protecting tissues from infection (52). While many studies have indicated that a type of immune peptide known as cathelicidin may be responsible for the role of vitamin D deficiency in infections, others argue that there is no association between cathelicidin levels and UTIs (49, 53).
3.3.3. Vitamin D and UTI
Despite several studies highlighting the link between vitamin D deficiency and UTIs, there is limited research examining whether vitamin D supplementation can lower UTI incidence or improve the treatment of the disease. In an RCT, Jorde et al. observed that supplementation with 20 000 IU per week led to a lower incidence of UTIs in adults (54). Therefore, there is still a lack of data on the impact of vitamin D in preventing or treating UTIs in pediatrics.
3.4. Vitamin E
3.4.1. Introduction
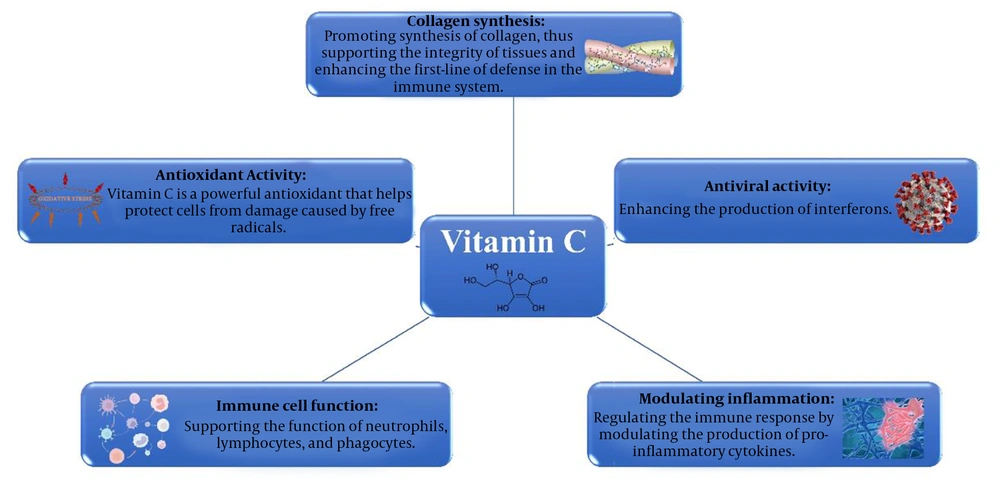
The use of vitamin E as an antioxidant to boost the immune system, particularly humoral immunity, has long been acknowledged (55). Furthermore, this vitamin has been recognized as a potent anti-inflammatory agent in both animal models and humans (56). Other molecular mechanisms of the role of vitamin E are supporting T- and B-cell function, as well as antioxidant activity (57-60). The molecular mechanisms of the role of vitamin E in the immune system are summarized in Figure 3. Lower levels of alpha-tocopherol – the most prevalent form of vitamin E – are linked to increased infections, poor growth, anemia, etc. (61).
Despite the various benefits of vitamin E supplementation, high doses of this vitamin have been shown to elevate overall mortality rates (62). Therefore, physicians should take this into consideration when recommending vitamin E supplements and advise against their consumption (63). However, the matter is subject to controversy.
3.4.2. Vitamin E and Kidney Disease
The impact of vitamin E on kidney disease dates back to early animal studies in the 1990s when vitamin E supplements were associated with reduced inflammation in pyelonephritis (56). Subsequent studies indicated that it could have a positive effect against nephropathy, renal scarring, and clinical symptoms and signs of UTIs (21, 64-66).
The initial studies conducted on rats by Bennett et al. suggested that vitamin A and E intake could be a potential treatment for reflux nephropathy (56). Later, Kongkham et al. examined the effects of alpha-tocopherol on contrast-induced nephropathy and demonstrated its protective influence on renal damage (64).
The relationship between vitamin E and renal scarring has been explored in several published articles. In 2008, Sadeghi et al. showed that an intraperitoneal injection of a vitamin E supplement prevented renal scarring after acute pyelonephritis in rats (67). Table 2 provides a summary of relevant human studies, wherein the three studies mentioned reported lower rates of renal scarring following vitamin E supplementation for acute pyelonephritis (21, 65, 66).
| Variables | |||
|---|---|---|---|
| Author | Sobouti et al. (21) | Yousefichaijan et al. (66) | Ghasemi et al. (65) |
| Method | A simple, non-blind, open-label, randomized clinical trial | A double-blinded randomized controlled trial | A single-blinded randomized controlled trial |
| Year | 2013 | 2015 | 2022 |
| Country | Tehran, Iran | Arak, Iran | Bandar Abbas, Iran |
| Number of participants (case/control) | 40 (20/20) | 152 (76/76) | 78 (37/41) |
| Age range, mo | 1 – 120 | 60 – 144 | 3 - 168 |
| Antibiotic treatment | According to the antibiogram profile, cephalothin or ampicillin (100 mg/kg/day 4 times daily) and amikacin (15 mg/kg/day 3times daily) for 10 days | Intravenous ceftriaxone 50 - 75 mg/kg/d, twice daily during hospitalization, and 8 mg/kg/d of oral cefixime twice daily after discharge | Intravenous ceftriaxone 50 - 75 mg/kg/d during the hospital stay |
| Vitamin E treatment duration b | 10 days | 14 days | 4 months |
| Placebo | None | Once daily | None |
| Follow-up time, mo | 6 | 4 – 6 | 4 |
Randomized Clinical Trials Evaluating the Association of Vitamin E Supplementation and Renal Scarring Following Acute Pyelonephritis in Pediatric Patients a
3.4.3. Vitamin E and UTI
Data about the impact of vitamin E on the clinical signs and symptoms of urinary tract infections are limited to our 2015 study. Our study revealed that a 14-day treatment with vitamin E supplements in addition to antibiotics in girls between the ages of 5 and 12 years with first-time acute pyelonephritis reduced the incidence of fever, urinary urgency, frequency, urinary dribbling, and urinary incontinence compared to antibiotic treatment alone (66). Further studies are necessary to confirm or challenge these findings.
3.4. Other Vitamins
The potential impacts of B-group vitamins and vitamin K supplements remain unexplored; thus, they were excluded from our current review.
4. Discussion
In this literature review, we delved into the role of vitamin supplementation in the treatment of UTI. Our aim was to investigate whether vitamin supplementation could be a viable option for UTI treatment. Our findings indicated that vitamins C, E, and A could be used in conjunction with antibiotic treatment.
The emergence of antibiotic resistance in UTI pathogens on a global scale is a growing concern (68-70). This increase in resistance, along with the appearance of multi-drug resistant (MDR) pathogens, is primarily the result of inadequate empirical therapy without proper testing to establish the susceptibility of the pathogens, leading to treatment failure for UTI (71). On the other hand, due to the severe course and potential complications of UTI, physicians often opt to initiate antibiotic therapy before conducting pathogen susceptibility testing. This circumstance has led us to consider the utilization of available adjunctive treatments to expedite the treatment process.
Previous articles have described alternative treatments. Chandra et al. have compiled a list of some alternative options, which include homeopathic medicine, Unani Medicine, and herbal-based medicine (72). One possible explanation for the mechanism of action of these alternatives is that herbal remedies can enhance the immune system. Additionally, Fazly Bazzaz et al. reviewed the effects of natural remedies in UTI treatment and reported positive outcomes when these remedies were incorporated alongside the main antibiotic treatment (73). However, it should be noted that some of these natural remedies are not universally accessible or have not obtained safety certifications. The advantage of vitamin supplementation over other alternatives lies in its safety and availability.
As mentioned earlier, there have been limited studies investigating the role of vitamin supplementation as an adjunctive treatment for UTI. Currently, we can hypothesize that vitamins A and E have the potential to decrease the incidence of renal scarring in UTIs. However, there is insufficient data to make a strong recommendation in this regard. As a result, we suggest that future articles design placebo-controlled studies with larger samples to further explore the role of vitamin A and E supplementation in preventing renal scarring.
With regard to vitamin C supplementation, we are convinced of its benefits in the treatment of various infections. However, we found that only one study has evaluated vitamin C supplementation specifically for UTI symptoms. Therefore, more research is needed to investigate the role of this vitamin in UTI recurrence and treatment. This is also the case for vitamin D supplementation. We did not come across any study investigating vitamin D supplements in pediatric patients with UTI, despite having nearly confirmed evidence that vitamin D deficiency and supplementation can decrease UTI incidence among adults. However, this could be due to the potential side effects of vitamin D supplementation. Nonetheless, further studies are required to establish the role of vitamin D deficiency and supplementation in pediatric patients.
4.1. Strengths and Limitations
This literature review provides a summary of the studies conducted thus far on the use of vitamin supplements as an alternative treatment for UTIs. The findings of our study highlight the potential benefits of utilizing vitamins in the treatment of UTIs, suggesting areas for further research. Still, it is important to consider the limitations of this review. We did not explore the role of other alternative treatments, such as mineral supplementation. Additionally, we were unable to conduct a comparative analysis or perform a meta-analysis due to the nature of a narrative review.
4.2. Conclusions
In general, vitamins play a crucial role in supporting the immune system. Specifically, vitamins C, E, and A have displayed encouraging outcomes as supplementary therapies for UTIs. Nevertheless, the available data on this subject are limited to a few RCTs, highlighting the need for additional research. Our intention with this review was to offer valuable insights into the involvement of vitamins in UTIs and to inspire further investigation in this field.
4.3. Expert Opinion
We can conclude from this review study that some vitamins are potential agents as a complementary treatment for UTI. According to previous studies, the suggested doses are 1,500 U/kg/d, with a maximum dose of 50 000 units, 20 U/kg/d, and 100 - 200 mg/day for vitamins A, E, and C, respectively.
According to our findings and the experience of the authors in the treatment of UTIs, the use of supplemental treatment with vitamins within the recommended dietary allowance can also help improve the symptoms and duration of UTIs in pediatrics, as the deficiency of most vitamins cannot be proven by testing and the clinical symptoms of deficiency appear only when a severe deficiency is present. According to the available studies, in addition to antibiotic treatment, treatment with vitamins A, E, and C should be more considered because they have been proven to reduce the symptoms and course of the disease.
Vitamin supplementation can decrease the economic burden of the disease as a low-risk and beneficial supplemental treatment as it reduces microbial resistance, doses and frequency of antibiotic treatments, and complications of the disease.
Further research is needed to expand our knowledge about the effects of vitamin supplementation on UTIs and to reveal the side effects.