1. Background
Kidney stones have been associated with an elevated susceptibility to chronic kidney disorders (1), end-stage renal failure (2), cardiovascular diseases, diabetes, and hypertension (3). The prevalence of kidney stone disease varies between 1% and 15% across individuals' lifetimes, depending on factors such as age, gender, ethnicity, and geographical location (4). Individuals requiring treatment for this condition are typically presented with five therapeutic options: Open surgery or retrograde intrarenal surgery (RIRS), percutaneous nephrolithotomy (PCNL), and extracorporeal shockwave lithotripsy (ESWL) (5). Initially introduced in the 1970s, PCNL was developed as a minimally invasive technique for eliminating kidney stones (6). Since 1980, PCNL has supplanted open surgery as the preferred approach for managing kidney stones larger than 2 cm due to its favorable outcomes in terms of reduced morbidity and shorter hospital stays (7).
Kidney stone disease, a condition characterized by recurrent occurrences, has detrimental effects on the quality of life of patients and imposes substantial financial burdens on healthcare systems (8). The demand for open surgery has considerably diminished as a result of advancements in ESWL and endourology techniques (9). Consequently, individuals who have previously undergone open stone surgery necessitate PCNL due to the recurrence of renal stones (10). Several studies indicated that prior open stone surgery could increase the failure rate of PCNL (11). At the same time, other research suggests that previous open stone surgery did not influence the outcomes of PCNL (12).
Notwithstanding its less intrusive nature compared to an open procedure, percutaneous renal surgery maintains a certain degree of risk regarding the occurrence of complications. Previous research has indicated that PCNL serves as an immensely proficient method of minimally invasive surgery, boasting success rates surpassing 90%. However, it is important to note that this approach has a higher prevalence of complications, exceeding 10%, as reported in relevant scholarly sources (13). Several meta-analytical studies have demonstrated reduced complication rates associated with PCNL, corroborating the notion of minimal adverse events (14).
2. Objectives
Despite using preoperative stone disease classification for over three decades, a standardized methodology to reliably forecast stone-free rates and complications remains elusive. While the ideal outcome is the complete eradication of stones, achieving this objective may prove challenging in some instances, mainly when dealing with stag-horn calculus or multiple calyces. Consequently, the present investigation retrospectively assessed the impact of previous therapeutic interventions for renal stones on the success rate and occurrence of complications during subsequent PCNL.
3. Methods
This retrospective descriptive-analytical study examined the data of 375 patients aged 18 years and above who had undergone PCNL at Imam Khomeini Hospital in Urmia, Iran. The reviewed data were during 2019 - 2021. The Ethics Committee of Urmia University of Medical Sciences approved the study (IR.UMSU.REC.1400.101).
3.1. Preoperative Evaluation
The patients were divided into four groups based on their prior therapeutic interventions. Group one comprised individuals (n = 196) without open renal stone surgery on the ipsilateral kidney. Group two consisted of patients (n = 64) with a history of PCNL. The third group included participants (n = 88) who had previously undergone ESWL. The fourth group encompassed individuals (n = 27) who had undergone open surgery procedures, such as open pyelolithotomy. The inclusion criteria were the absence of coagulopathy. Furthermore, individuals with a body mass index (BMI) equal to or exceeding 30 kg/m2 and those requiring a blood transfusion during the surgical procedure were deemed ineligible for participation.
The data for this study were extracted from patients' medical records, which included pre- and postoperative hemoglobin levels and duration of hospital stay stratified by age, gender, and BMI. In addition, we documented the success rate of the surgical procedure and the occurrence of complications, such as systemic inflammatory response syndrome (SIRS), the need for angioembolization, prolonged urinary leakage, infection, colon perforation, or mortality. Furthermore, the location and size of the stones were carefully examined and compared between different groups. Patients who tested positive for urine culture received appropriate antibiotic treatment for a minimum duration of two weeks prior to undergoing PCNL. Intravenous urography was the primary imaging modality, with computed tomography (CT) scans performed whenever necessary. The maximum stone length, as determined by CT measurements, was defined within the range of 2 - 4 cm.
3.2. Surgical Procedure
Following the induction of general anesthesia, a ureteral catheter with a diameter of 5 - 6 French (F) was inserted and secured alongside a Foley catheter. Subsequently, the patients were positioned in a prone posture, with particular attention paid to relieving pressure points. With the aid of fluoroscopy guidance, the targeted calyx was punctured, and a guide wire was introduced. Sequential metallic dilators were employed to expand the tract. Once an Amplatz sheath was successfully placed, nephroscopy was carried out, and stone fragmentation and removal were accomplished using a pneumatic lithotripter (Litho Crack, Sp. Swiss-Germany). Continuous irrigation with normal saline was maintained throughout the procedure. In cases where a residual stone exceeding 2 cm in diameter could not be accessed through the initial tract, secondary access was established. Residual stones measuring less than 2 cm were designated for treatment via ESWL; however, ESWL was not performed immediately postoperative. The Foley catheter and ureteral catheter were removed 24 h after the surgery, while the nephrostomy tube was clamped 48 h post-operation. Provided there was no evidence of urine leakage, pain, or fever, the tube was removed after an additional 24 h. It is essential to emphasize that meticulous attention was paid throughout the procedure to ensure optimal patient safety and comfort.
3.3. Postoperative Evaluation
A complete blood count and serum electrolytes were examined on the first day after the surgical procedure. Fever was considered in patients experiencing a body temperature exceeding 38°C during the postoperative period. Cold compression, antipyretics, and antibiotics were administered as necessary. Additionally, a comprehensive assessment involving plain radiography and abdominal ultrasonography or CT scan (for cases involving radiolucent stones) was performed within one day to identify residual stones. If no significant residual stones were detected, the nephrostomy tube was removed. The ureteral catheter was removed when urinary leakage from the site of nephrostomy removal was less than 100 mL/day. The objective of the study was to establish the stone-free rate (SFR), which was subsequently compared with diagnostic modalities employed before the surgery. Complications were assessed using the Clavien classification (15), and successful outcomes were defined as the complete removal of stones (Stone Free/SF) or clinically insignificant residual stones (CIRF) that were asymptomatic and smaller than 4 mm in size. Statistical analysis was conducted using SPSS software version 17 and the chi-Square test, with P-values below 0.05 considered statistically significant.
4. Results
The demographic variables and operation features of the study groups are shown in Table 1. There was a higher number of males than females in all groups. There was no statistically significant difference between the four groups concerning gender, age, and BMI. Patients’ mean age in group 4 was higher (48.18 ± 9.8) compared to the other three groups. The mean BMI was similar among all groups. BMI was 27.67 ± 5.83 kg/m2 in group 1, 28.93 ± 7.19 kg/m2 in group 2, 27.91 ± 4.83 kg/m2 in group 3, and 27.01 ± 3.38 kg/m2 in group 4 (P = 0.39).
| Variables | Group 1 | Group 2 | Group 3 | Group 4 | P-Value |
|---|---|---|---|---|---|
| Gender | 0.66 | ||||
| Male | 117 (59.7) | 44 (68.8) | 50 (56.8) | 18 (66.7) | |
| Female | 79 (43) | 20 (31.3) | 38 (43.2) | 9 (33.3) | |
| Age (y) | 45.34 ± 16.27 | 46.15 ± 12.95 | 44.81 ± 13.64 | 48.18 ± 9.87 | 0.74 |
| Body mass index (kg/m2) | 27.67 ± 5.83 | 28.93 ± 7.19 | 27.91 ± 4.83 | 27.01 ± 3.38 | 0.39 |
| Operation duration (min) | 57.32 ± 18.36 | 58.46 ± 15.75 | 57.64 ± 18.79 | 61.66 ± 19.85 | 0.88 |
| Hospital stay (day) | 3.93 ± 1.47 | 3.90 ± 1.47 | 3.92 ± 1.45 | 3.89 ± 1.42 | 0.96 |
| Preoperative hemoglobin changes | -1.25 ± 0.07 | -1.49 ± 0.46 | -1.54 ± 0.12 | -1.46 ± 0.22 | 0.14 |
| Preoperative hemoglobin changes 48 hours after operation surgery (g/L) | -1.56 ± 0.08 | -1.81 ± 0.5 | -1.66 ± 0.12 | -2.05 ± 0.28 | 0.19 |
| Site of stone | 0.41 | ||||
| Pelvis | 71 (34.5) | 19 (30.3) | 30 (37.5) | 8 (29.7) | |
| Upper calyx | 44 (30.6) | 17 (21.2) | 24 (22.3) | 7 (25.2) | |
| Middle calyx | 19 (10.5) | 8 (13.2) | 9 (11.5) | 3 (11.1) | |
| Lower calyx | 52 (25.2) | 18 (29.8) | 23 (26.4) | 9 (33.3) | |
| Ureter | 10 (5.1) | 2 (3.1) | 2 (2.3) | 0 (0) | |
| Stone size (cm) | 3.04 ± 0.21 | 3.34 ± 0.41 | 3.7 ± 0.57 | 3.56 ± 1.37 | 0.64 |
| Access time (min) | 70.58 ± 59.28 | 63.51 ± 38.98 | 57.8630 ± 0.23 | 81.53 ± 41.83 | 0.31 |
Values are expressed as Mean ± SD or No. (%).
Mean surgery duration was 57.32 ± 18.36, 58.46 ± 15.75, 57.64 ± 18.79, and 61.66 ± 19.85 minutes in groups 1, 2, 3, and 4, respectively (P = 0.88). The mean hospital stay between the four groups was not statistically different (P = 0.96). Compared to preoperative hemoglobin, there was a drop in the mean postoperative hemoglobin among four groups (-1.56 ± 0.08, -1.81 ± 0.5, -1.66 ± 0.12, and -2.050.28 ± g/L, respectively) which was not significantly different (P = 0.19).
All patients had a high number of pelvis stones in the four groups. Upper calyceal stones were detected in 30.6% of patients in group one, 21.2% of group two, 22.3% of group three, and 25.2% of group four. Middle calyceal and ureteral stones had a low rate among the four groups. All groups had nearly similar lower calyceal stone rates. No significant difference was observed between the groups concerning the stone site (P = 0.41). The mean stone size was similar in all groups (3.04 ± 0.21, 3.34 ± 0.41, 3.7 ± 0.57, 3.56 ± 1.37, respectively). There was no significant difference between the groups regarding the stone size (P = 0.64). Access time was longer in groups one and four (70.58 ± 59.28 and 81.53 ± 41.83, respectively) compared to other groups, but no statistically significant difference was observed (P = 0.31).
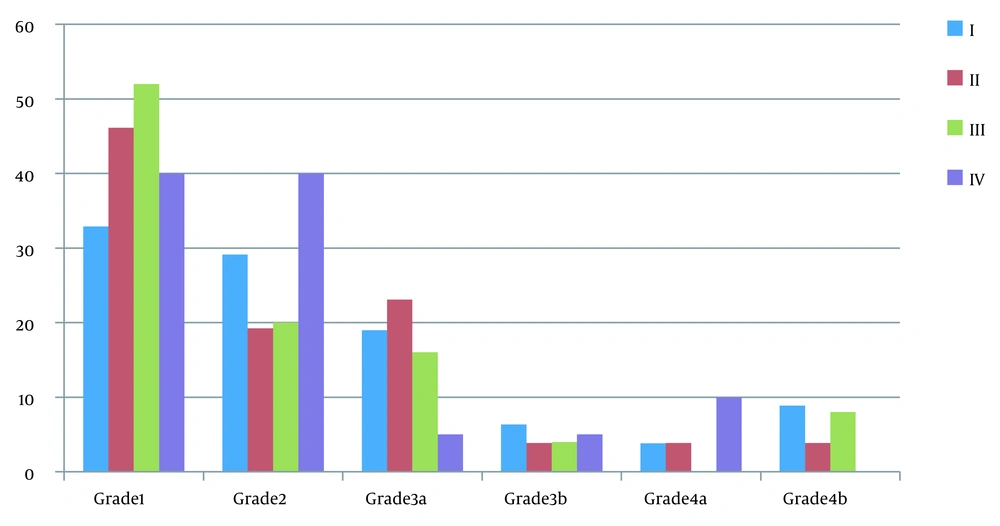
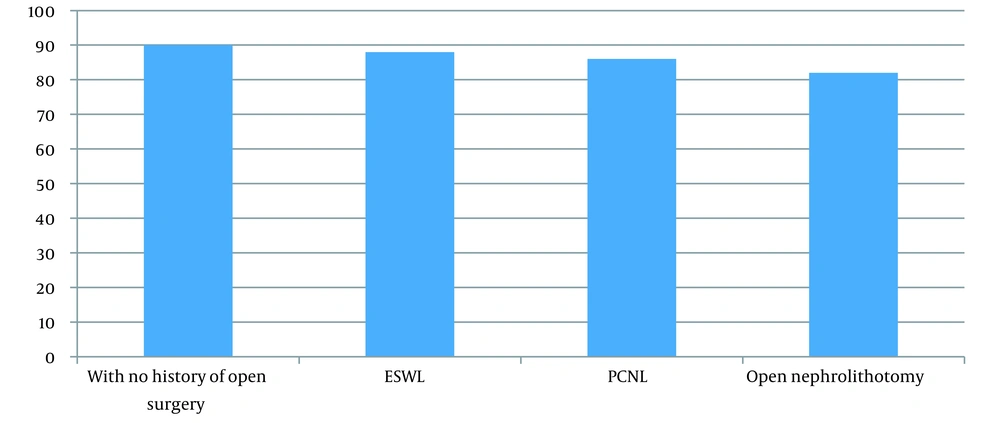
The complications were determined by the modified Clavien classification system, are presented in Figure 1, and are described in detail in Tables 2 and 3. In group 1, the most frequently observed complication was grade 1 (32.91%), while the least frequent complication was grade 4a (3.8%). Group 2 patients exhibited the highest frequency of grade 1 complications (46.15%) and the lowest frequencies for grades 4a, 3b, and 4b complications (3.85%). Within group 3, approximately half of the patients were classified as grade 1 (52%), and no instances of grade 4a complications were recorded. Among the patients in group 4, 40% were categorized as grade 1 and 40% as grade 2, with no occurrences of grade 4b complications. Notably, no cases of grade 5 complications were recorded in any of the treatment groups (not shown in Figure 1). As Table 3 displays, postoperative fever developed in 16 (8.1%) patients in group one, 8 (12.5%) in group two, 9 (10.22%) in group three, and 5 (18.5%) in group four. Due to decreased hemoglobin in all groups, blood transfusion was administered to 12 patients in all groups. Only a few patients required angioembolization (1 in the first and 2 in the second groups). As Table 3 shows, grade 1 and 2 complications had a high-frequency rate among the patients. None of the patients had grade 5 complications. The overall immediate success rate was 90% in group one, 86% in group two, 88% in group three, and 82% in group four (Figure 2).
| I | II | III | IV | |
|---|---|---|---|---|
| Grade 1 | 32.91 | 46.15 | 52 | 40 |
| Grade 2 | 29.11 | 19.23 | 20 | 40 |
| Grade 3a | 18.99 | 23.08 | 16 | 5 |
| Grade 3b | 6.33 | 3.85 | 4 | 5 |
| Grade 4a | 3.8 | 3.85 | 0 | 10 |
| Grade 4b | 8.86 | 3.85 | 8 | 0 |
| Grade | Group 1 | Group 2 | Group 3 | Group 4 |
|---|---|---|---|---|
| Grade 1, fever | 16 (8.1) | 8 (12.5) | 9 (10.22) | 5 (18.5) |
| Transient serum creatinine elevation | 10 (5.15) | 4 (6.25) | 4 (4.5) | 3 (11.11) |
| Grade 2, blood transfusion | 12 (6.1) | 3 (4.7) | 4 (4.5) | 3 (11.2) |
| Urine leakage for longer than 24 hours | 5 (2.55) | 1 (1.5) | 1 (1.1) | 1 (3.7) |
| Wound infection | 4 (2.04) | 1 (1.5) | 0 (0.0) | 2 (7.4) |
| Pneumonia | 2 (1.02) | 0 (0.0) | 0 (0.0) | 1 (3.7) |
| Grade 3a, renal hemorrhage requiring angioembolization | 1 (0.51) | 2 (3.12) | 0 (0.0) | 0 (0.0) |
| Hemo/pneumothorax requiring chest tube insertion | 2 (1.02) | 0 (0.0) | 1 (1/1) | 1 (3.7) |
| Retention due to blood clots | 12 (6.12) | 4 (4.5) | 3 (4.6) | 0 (0.0) |
| Grade 3b, ureteric calculus | 3 (1.56) | 1 (1.5) | 1 (1.1) | 0 (0.0) |
| Infundibular stricture | 2 (1.02) | 0 (0.0) | 0 (0.0) | 1 (3.7) |
| Grade 4a, neighboring organ injury | 1 (0.51) | 0 (0.0) | 0 (0.0) | 1 (3.7) |
| Myocardial infarction | 1 (0.51) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Acute renal failure | 1 (0.51) | 1 (1.51) | 0 (0.0) | 1 (3.7) |
| Grade 4b, sepsis | 7 (3.5) | 1 (1.5) | 2 (2.2) | 0 (0.0) |
| Grade 5, death | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
Values are expressed as No. (%).
5. Discussion
In the last two decades, there have been significant advancements in surgical interventions for renal tract stone disease, particularly with the introduction of minimally invasive techniques like ESWL and PCNL (10). PCNL has become a widely utilized procedure among patients with renal calculi (16). Due to the high recurrence rates of renal stones, these patients often require additional intervention. Previous studies suggested that individuals who have undergone open interventions in the past may experience higher failure rates with subsequent PCNL procedures (17). However, this study compared four groups with different histories of renal surgery. It determined that the type of previous stone surgery did not impact the outcomes or complications of subsequent PCNL procedures. These findings align with other studies that have demonstrated the successful execution of PCNL with minimal risk of complications in patients who have previously undergone open surgery or PCNL (10, 18).
In the present study, no statistically significant difference was observed between the four groups concerning gender, age, and BMI. However, the patient's mean age in the group with a history of open surgery was higher than the other three groups. No significant difference was found between the groups concerning demographic characteristics, which is in line with the literature (19).
Based on the findings of the present investigation, the patients with a history of previous open surgery exhibited a higher mean duration of operative time. This result is in accordance with earlier studies which have also documented prolonged operative times for individuals who had previously undergone open nephrolithotomy (18, 20). Several factors may potentially contribute to the extended duration of PCNL procedures in patients with prior open surgery or PCNL. These factors include the inherent challenges associated with dilating the tract within a scarred collecting system and perinephric spaces, difficulties encountered during the extraction of stone fragments using grasping forceps and rigid nephroscopy within a scarred kidney, as well as the meticulous fixation of the kidney within the retroperitoneum.
The present investigation demonstrated comparable durations of hospitalization among the four examined groups, with no patients necessitating extended stays in the hospital. Inconsistencies regarding hospitalization outcomes subsequent to PCNL have been noted in prior research (10, 18, 19). Certain studies have indicated prolonged hospital stays for individuals who had undergone previous open surgery, contrasting with the findings of our study (21, 22).
Both study groups, with and without prior open surgery, exhibited long access times. Similar findings were reported by Margel et al. and Khorrami et al., who observed greater access attempts in patients with previous open surgery (22, 23). Importantly, our study revealed that a history of renal stone surgery did not adversely affect the success rate of PCNL. The success rates were 90% in group one, 86% in group two, 88% in group three, and 82% in group four. These results align with the outcomes reported by Kurtulus et al. (24), who compared the success rates of patients undergoing initial PCNL surgery for kidney stones with those previously undergoing open kidney stone surgeries. They found no significant difference in cumulative stone-free rates between the two groups. However, other studies have suggested that open stone surgery may increase the failure rate of PCNL (25, 26). Furthermore, it was observed that success rates declined as the number of accesses increased (19).
An important finding of this study was that patients who had no prior experience with open surgery but underwent cold compression and received antipyretics showed a significant incidence of postoperative fever. This observation contradicts the findings of Khorrami et al. (23), which did not identify any differences in fever-related complications.
Hemorrhage, attributed to the kidney's high vascularity, represents a notable complication of PCNL. Hemorrhage of varying degrees is observed in every PCNL procedure (27), predominantly stemming from venous sources and often manageable through conservative measures (28). Reddy and Shaik reported instances of acute bleeding requiring transfusion among patients without a history of open surgery (10). In situations where conservative approaches prove ineffective, angioembolization emerges as a successful and efficacious intervention for terminating bleeding, with a reported success rate of 95% (29). Our study witnessed a limited number of cases necessitating angioembolization, akin to the hemorrhage rate of 0.8% requiring embolization reported by Zhang et al. (30). Grade 1 and 2 complications were frequently observed in our study cohort. In contrast, no grade 5 complications were encountered, consistent with earlier literature (5, 31-33).
The current study was subject to certain limitations, including a limited sample size and a retrospective design, which could potentially impact the strength of the findings. Furthermore, the surgeries were performed by a team comprising consultants and resident doctors, as per the teaching hospital setting, rather than a single surgeon. Notwithstanding these limitations, the study's favorable outcomes regarding the effectiveness of PCNL in this specific patient population may be significant and merit further exploration through a prospective study involving a larger sample size.
5.1. Conclusions
PCNL has emerged as an effective and safe treatment option for kidney stone management, irrespective of prior interventions. This minimally invasive approach offers a viable choice for all patients. Our study revealed that individuals with a history of open surgery exhibited higher levels of hemoglobin loss and longer surgical durations, potentially attributable to underlying histological and anatomical alterations in the kidney. Nevertheless, conducting larger-scale prospective multicenter studies to validate these findings is crucial.