1. Background
Chronic kidney disease (CKD) is a progressive condition characterized by a gradual decline in renal function over time (1), affecting nearly all physiological systems and organs. Common manifestations include electrolyte and acid-base imbalances (2). Globally, the prevalence of CKD is estimated at 13.4% (11/15 - 7/15), with the number of individuals requiring renal replacement therapy for end-stage renal disease (ESRD) ranging from 4.902 to 7.083 million. The significant number of deaths due to limited access to renal replacement therapy in developing countries, along with the projected increase in ESRD cases, is likely to place substantial economic burdens on even affluent nations (3). The management of CKD costs approximately 4.8 billion dollars annually, while ESRD incurs costs of up to 32.9 billion dollars (4).
End-stage renal disease necessitates renal replacement therapy, typically achieved through dialysis or transplantation. Although transplantation significantly enhances survival rates and quality of life, the majority of patients initially receive hemodialysis (5). This process removes waste products and excess fluids accumulated in the body due to kidney failure by circulating the patient's blood through a dialyzer (6). Hemodialysis is the predominant form of renal replacement therapy worldwide, constituting approximately 69% of all renal replacement therapies and 89% of all dialysis treatments (7). In Iran, the number of people undergoing hemodialysis is estimated to be between 40,000 and 50,000 (8).
Despite considerable technological and technical advancements in hemodialysis, challenges persist both during and after the procedure (9). While hemodialysis prolongs patients' lifespans, it also imposes various limitations that may result in physical, psychological, social, and economic complications (10, 11). One of the most common side effects during hemodialysis is fluctuating blood pressure, typically characterized by hypotension and, in 10 to 15% of cases, hypertension (12, 13). This complication is more prevalent among elderly patients, those on antihypertensive medications, and individuals with lower serum creatinine levels, and is independently associated with increased hospitalization rates and reduced survival rates (14, 15). Volume overload is a primary contributor to blood pressure alterations in hemodialysis patients. While antihypertensive medications may effectively address hypertension in a minority of patients for whom factors other than extracellular fluid volume contribute to blood pressure elevation, precise volume management provides optimal blood pressure control for the majority of these patients (16).
One nursing intervention available to dialysis nurses to reduce the likelihood of blood pressure-related complications during dialysis is the regulation of the ultrafiltration profile (17). Adjustments to the ultrafiltration profile can be made by configuring the dialysis machine to remove fluids from the patient's blood at a rate consistent with the predetermined profile. Decreasing the rate of ultrafiltration during the latter stages of dialysis may prove effective in preventing such complications (18, 19).
In certain studies, adjusting the ultrafiltration profile in conjunction with the sodium profile has shown favorable outcomes in balancing the blood pressure of patients experiencing hypotension during hemodialysis (17, 20). However, findings from a crossover clinical trial indicated that employing a linear ultrafiltration profile method with a negative slope yielded no significant difference compared to the conventional method in managing blood pressure elevation during hemodialysis (21). To date, most research in the domain of blood pressure regulation among dialysis patients has focused on preventing severe blood pressure drops. However, elevated blood pressure also causes serious complications in hemodialysis patients.
2. Objectives
Given the limitations of previous studies and the lack of examination into the efficacy of the negative slope ultrafiltration profile in addressing high blood pressure in these patients—an intervention that is relatively straightforward and lacks the cost and side effects associated with antihypertensive medications—the present study was undertaken to investigate the impact of ultrafiltration profiling compared to the conventional method on blood pressure regulation among hemodialysis patients.
3. Methods
3.1. Study Design
The present study employed a pre-test and post-test design involving a group of 30 hemodialysis patients at Shahid Beheshti Hospital in Hamadan, Iran. Conducted in 2022, the study comprised the implementation of both routine and ultrafiltration profiling methods.
3.2. Sample and Sampling Method
Initially, a sampling frame was created using a list of hemodialysis patients obtained from the hospital's information technology unit. Out of 250 patients, 158 met the eligibility criteria for participation. Using a random number table, 30 patients were then selected and enrolled in the study.
The inclusion criteria included individuals aged between 18 and 75 years, who had been undergoing hemodialysis for more than three months, experienced a weight gain of 1 to 3 kg between dialysis sessions, were diagnosed with end-stage kidney disease, and exhibited an upward trend in blood pressure during hemodialysis over the previous three months. Additionally, participants must not have had a history of specific cardiovascular ailments such as myocardial infarction or the need for a pacemaker, and must not have suffered from severe anemia (Hb < 8). Informed consent to participate in the study was also required.
Conversely, exclusion criteria included severe cardiac and pulmonary disorders such as unstable angina or myocardial infarction occurring during dialysis, death during the course of the study, and non-cooperation from the patient.
3.3. Data Collection Tool
The data collection instrument used in this study was a comprehensive checklist that included patient demographic information and details about the dialysis machine. The checklist covered variables such as age, gender, duration of hemodialysis treatment, medical history, as well as pre-and post-dialysis blood pressure and weight. These data were collected through a combination of file review, patient interviews, and instrumental measurements. For blood pressure measurement, an Ecomode KG-106 hand sphygmomanometer, manufactured in Iran and used with a stethoscope, was employed.
The content validity of the checklist was established through face validity. After a thorough review of authoritative literature and consultation with respected professors and experts, the checklist was formulated. Feedback was then sought from ten faculty members of the Nursing and Midwifery College at Hamadan, whose consensus confirmed the relevance and comprehensiveness of the questionnaire content.
To ascertain the reliability or instrumental precision of the sphygmomanometer, a test-retest method was employed. Systolic and diastolic blood pressure readings were taken three times from five individuals at five-minute intervals, maintaining consistency in their condition. Cronbach's alpha coefficients for both systolic and diastolic readings exceeded 75%, validating the instrument's reliability.
The accuracy of the hemodialysis machines was validated by the medical equipment unit of the hospital, ensuring uniformity as the same machines were used for all patients throughout the study period.
3.4. Methodology and Intervention
Each participant underwent a total of six sessions within a maximum timeframe of two months. During the initial three sessions, participants received standard hemodialysis, followed by three subsequent sessions where they underwent hemodialysis with ultrafiltration profiling. The average systolic and diastolic blood pressure readings were obtained by a single observer both pre- and post-hemodialysis in each session. Subsequently, the average blood pressure values from the three routine sessions were compared to those from the three sessions using the ultrafiltration profiling method. Notably, blood pressure was monitored and recorded five times during each session: Immediately pre-dialysis, at the first, second, and third hour of dialysis, and fifteen minutes after the completion of dialysis.
For this study, the protocol outlined by Flythe et al. was adopted for study design and implementation (21).
3.5. Hemodialysis Machine Settings
The dialysis machine settings were standardized for all participants, with the sodium concentration set constantly at 138 milliequivalents and linearly, the solution temperature maintained at 36.5 degrees Celsius, and the pump speed calibrated to 250. The ultrafiltration profile was configured to operate over three sessions with an interval design featuring a negative slope. Only B-Braun devices, calibrated within the preceding three months, were used for all participants, incorporating the Luflux strainer in all sessions.
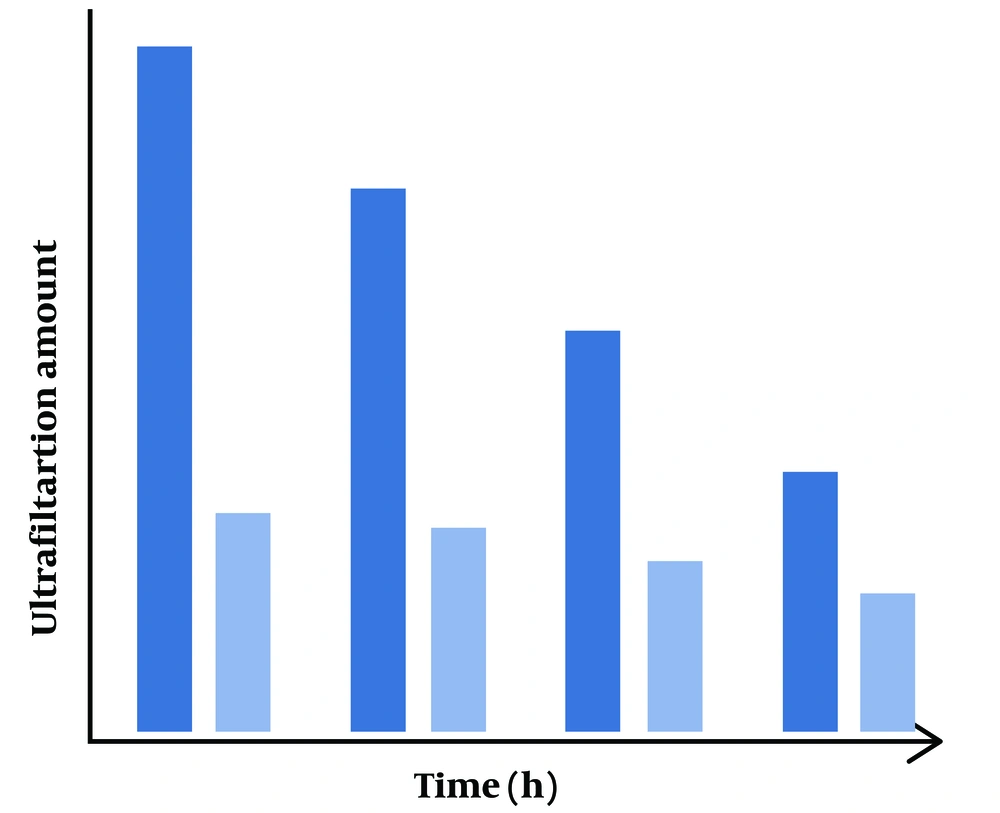
Participants were blinded as to whether each session incorporated the ultrafiltration profile. Additionally, safety precautions were implemented to ensure safety, with a contingency plan in place to revert to standard dialysis settings in case of abnormal blood pressure increases. The ultrafiltration profile during the hemodialysis intervention followed the selective profile depicted in Figure 1, wherein water intake was gradually reduced from the commencement to the conclusion of hemodialysis.
3.6. Ethical Considerations
This study was approved by the Ethics Committee of Hamadan University of Medical Sciences (ethics code: IR.UMSHA.REC.1400.844). Before enrollment, the study protocol was thoroughly explained to prospective participants by the researcher. Subsequently, written informed consent was obtained from all participants. Assurance was given regarding the confidentiality of their personal information, ensuring that data would be used solely for research purposes and shared only in aggregate form. Additionally, participants were informed of their right to withdraw from the study at any stage.
3.7. Statistical Analysis
Data analysis was conducted using SPSS-19 software. Descriptive statistics, including mean, standard deviation, frequency, and percentage, were employed to summarize the data. To compare the average blood pressure at each stage of the study between the routine method and the ultrafiltration profile method, the paired t-test was utilized. Furthermore, to explore the trend of blood pressure changes during different stages of dialysis for each method, repeated measures analysis of variance (ANOVA) was employed. Tukey's post-hoc test was applied to pairwise comparisons of blood pressure assessment times. All statistical tests were conducted at a 95% confidence level.
4. Results
The study revealed that the mean age of the dialysis patients under investigation was 55.23 ± 9.23 years, with an average duration of dialysis treatment of 4.61 ± 2.41 years. The majority of the patients were male (60%), married (96.7%), and underwent dialysis three times a week (50%). Additionally, most patients had a fistula (56.7%), while a significant proportion had a history of kidney transplant and rejection (86.7%) (Table 1).
| Features | Values |
|---|---|
| Sex | |
| Female | 12 (40) |
| Male | 18 (60) |
| Marital status | |
| Single | 1 (3.3) |
| Married | 29 (96.7) |
| Dialysis session (per week) | |
| Three | 15 (50) |
| Four | 11 (36.7) |
| Five | 4 (13.3) |
| Vascular access | |
| Fistula | 17 (56.7) |
| Catheter | 13 (43.3) |
| History of kidney transplantation | |
| Once | 26 (86.7) |
| Twice | 4 (13.3) |
| Age (y) | 55.23 ± 9.23 (18 - 66) |
| Dialysis treatment period (y) | 4.61 ± 2.41 (0.8 - 10.01) |
a Values are expressed as No. (%) or mean ± SD.
The paired t-test results showed a significant difference in the average systolic blood pressure among patients during three sessions, particularly between the pre-dialysis stage and 1 hour post-dialysis commencement, when comparing the routine method with the ultrafiltration profile method (P < 0.05). Notably, systolic blood pressure was higher in patients using the ultrafiltration profile method. Conversely, during the 2 hours following dialysis, no significant difference was observed between the routine method and the ultrafiltration profile method (P = 0.106). However, in subsequent stages, specifically 3 hours post-dialysis commencement and 15 minutes post-dialysis completion, the mean systolic blood pressure of patients using the ultrafiltration profile method was significantly lower than those using the routine method (P < 0.05 (Table 2).
| Stages | Routine | Ultrafiltration Profile | Paired t-Test |
|---|---|---|---|
| Just before start | 131.55 (12.50) | 134.05 (12.33) | t = - 4.37, df = 29, P < 0.001 |
| 1-hour after | 141.04 (11.60) | 142.58 (11.61) | t = - 2.27, df = 29, P = 0.030 |
| 2-hour after | 150.22 (10.43) | 148.93 (12.40) | t = 1.66, df = 29, P = 0.106 |
| 3-hour after | 159.01 (10.10) | 155.65 (14.97) | t = 2.85, df = 29, P = 0.008 |
| 15-mins after the end | 168.23 (9.86) | 164.57 (15.82) | t = 2.57, df = 29, P = 0.015 |
| Repeated measures analysis of variance | F = 23.85, df = 1, P < 0.001 | ||
a Values are expressed as No. (%) or mean ± SD.
To assess the changes in mean systolic blood pressure across different stages of the study, a repeated-measures analysis of variance revealed a consistent increase in blood pressure for both methods (routine and ultrafiltration profile). Nonetheless, a significant difference was observed between the methods overall (P < 0.001), with patients using the ultrafiltration profile method experiencing smaller increases in blood pressure compared to those using the routine method throughout the study stages (Table 2).
To conduct pairwise comparisons of the average systolic blood pressure across different phases within each method, Tukey's post hoc test results demonstrated a significant elevation in systolic blood pressure among patients at each stage of dialysis compared to the preceding stage for both the routine and ultrafiltration profile methods (P < 0.001). However, an important observation pertains to the differences between the average blood pressure at each stage and the preceding stage between the methods, as detailed in each row of the table. Across all stages of the study, the increase in average blood pressure from the preceding stage was more pronounced in patients undergoing the routine method compared to those undergoing the ultrafiltration method. These findings suggest that during dialysis, the ultrafiltration method was more effective in mitigating further increases in blood pressure (Table 3).
| Stages | Methods | |
|---|---|---|
| Routine | Ultrafiltration Profile | |
| Mean Difference (P-Value) | Mean Difference (P-Value) | |
| Just before start | ||
| 1 hour after start | 9.48, (< 0.001) | 8.43, (< 0.001) |
| 2 hours after start | 18.66, (< 0.001) | 14.77, (< 0.001) |
| 3 hours after start | 27.45, (< 0.001) | 21.50, (< 0.001) |
| A quarter after the end | 36.67, (< 0.001) | 30.42, (< 0.001) |
| 1 hour after start | ||
| 2 hours after start | 9.17, (< 0.001) | 6.34, (< 0.001) |
| 3 hours after start | 17.96, (< 0.001) | 13.06, (< 0.001) |
| A quarter after the end | 27.18, (< 0.001) | 21.98, (< 0.001) |
| 2 hours after start | ||
| 3 hours after start | 8.78, (< 0.001) | 6.72, (< 0.001) |
| A quarter after the end | 18.01, (< 0.001) | 15.64, (< 0.001) |
| 3 hours after start | ||
| A quarter after the end | 9.22, (< 0.001) | 892, (< 0.001) |
The average total diastolic blood pressure among the examined patients varied across different dialysis stages during three sessions. According to the paired t-test, patients receiving the ultrafiltration profile method exhibited higher diastolic blood pressure levels than those using the routine method before dialysis initiation (P < 0.05). However, one hour after the commencement of dialysis, there was no significant difference between the methods (P = 0.179). Conversely, at 2- and 3-hours post-dialysis initiation, and fifteen minutes after its completion, the average diastolic blood pressure of patients using the ultrafiltration profile method was significantly lower than those undergoing the routine method (P < 0.05) (Table 4).
| Stages | Routine | Ultrafiltration Profile | Paired t-Test |
|---|---|---|---|
| Before start | 81.01 (8.91) | 82.66 (9.15) | t = 3.31, df = 29 , P = 0.002 |
| 1 hour after | 87.85(8) | 88.51 (8.54) | t = -1.37, df = 29 , P = 0.179 |
| 2 hours after | 93.92 (7.13) | 92.77 (8.73) | t = 2.10 , df = 29 , p = 0.044 |
| 3 hours after | 100.30 (7.60) | 97.83 (11.03) | t=2.71, df = 29, P = 0.011 |
| A quarter after the end | 107.98 (8.40) | 104.91 (12.35) | t = 2.87, df = 29, P = 0.008 |
| Repeated measures analysis of variance | F = 9.30, df = 1, P = 0.002 | ||
a Values are expressed as No. (%) or mean ± SD.
To assess changes in average diastolic blood pressure across study stages, repeated measures analysis of variance revealed significant differences between the routine and ultrafiltration profile methods (P < 0.001). Although there was an incremental trend in diastolic blood pressure across dialysis stages for both methods, patients using the ultrafiltration profile method exhibited a smaller increase in mean diastolic blood pressure compared to those using the routine method (Table 4).
According to Tukey's post-hoc test results, the average diastolic blood pressure of patients at different stages within each method increased significantly over time compared to the preceding stage (P < 0.001). However, the average difference in diastolic blood pressure between consecutive stages was more pronounced among patients undergoing the routine method. These findings suggest that the ultrafiltration method was more effective in preventing substantial increases in diastolic blood pressure during dialysis (Table 5).
| Stages | Routine | Ultrafiltration Profile |
|---|---|---|
| Mean Difference (P-Value) | Mean Difference (P-Value) | |
| Just before start | ||
| 1 hour after start | 6.84, (< 0.001) | 5.84, (< 0.001) |
| 2 hours after start | 12.91, (< 0.001) | 10.11, (< 0.001) |
| 3 hours after start | 19.28, (< 0.001) | 15.16, (< 0.001) |
| A quarter after the end | 26.97, (< 0.001) | 22.24, (< 0.001) |
| 1 hour after start | ||
| 2 hours after start | 6.06, (< 0.001) | 4.26, (< 0.001) |
| 3 hours after start | 12.44, (< 0.001) | 9.32, (< 0.001) |
| A quarter after the end | 20.13, (< 0.001) | 16.40, (< 0.001) |
| 2 hours after start | ||
| 3 hours after start | 6.37, (< 0.001) | 5.05, (< 0.001) |
| A quarter after the end | 14.06, (< 0.001) | 12.13, (< 0.001) |
| 3 hours after start | ||
| A quarter after the end | 7.68, (< 0.001) | 7.07, (< 0.001) |
5. Discussion
The present study investigates and evaluates the effects of ultrafiltration profiling compared to conventional methods on blood pressure regulation among hemodialysis patients, an area with limited comparative research. Drawing inspiration from previous studies that utilized ultrafiltration with sodium to mitigate blood pressure drops—such as Borzou et al.'s investigation, which demonstrated significantly reduced hypotension incidence and enhanced patient comfort (22)—our study explores the efficacy of ultrafiltration without sodium and employs an interval profile with a negative slope.
Our findings indicate that the ultrafiltration approach effectively mitigates further elevation in blood pressure throughout the dialysis process, though blood pressure was elevated by both routine and ultrafiltration methods. Aligned with the findings of Hamidi et al., who observed reduced complications and treatment measures with the use of linear and stepped sodium-ultrafiltration profiles compared to the routine method, particularly noting lower hypotension occurrences (8), our results reinforce the potential benefits of innovative ultrafiltration techniques. Additionally, many studies have shown that ultrafiltration rates and profiles affect intradialytic blood pressure and cardiovascular outcomes. Flythe et al. conducted a randomized crossover trial and determined that ultrafiltration profiling, which involves a constantly evolving ultrafiltration rate, did not reduce the risk of cardiac stress caused by treatment but did reduce the risk of lightheadedness and hypervolemia after dialysis (21). Mahony and Ward also examined the use of blood volume monitoring to guide ultrafiltration and optimize intradialytic blood pressure, concluding that it may assist in preventing intradialytic hypotension and achieving dry weight (23). According to Yu et al., high ultrafiltration rates (> 10 mL/h/kg) are associated with intradialytic hypotension in humans (24). Additionally, studies suggest that blood volume monitoring-guided ultrafiltration biofeedback reduced intradialytic hypotension and improved cardiac function (25, 26). It is therefore suggested that ultrafiltration methods may have an indirect effect on blood pressure during dialysis, and that individualized and tailored ultrafiltration strategies may help improve hemodynamic stability and cardiovascular outcomes during dialysis.
It appears that the etiology of elevated blood pressure during dialysis among hemodialysis patients involves multifactorial contributors, notably extracellular volume overload, hyperactivity of the renin-angiotensin-aldosterone system, sympathetic nervous system activation, and endothelial dysfunction. Management challenges include fluctuations in interdialytic and intradialytic blood pressure, alongside the absence of consensus on optimal target blood pressure levels and first-line pharmacotherapy. Although renin-angiotensin-aldosterone system antagonists, adrenergic receptor blockers, and calcium channel blockers are commonly prescribed, individualized treatment approaches are imperative, considering patient-specific factors (27).
The study's strengths lie in its novel investigation and comparison of systolic and diastolic blood pressure dynamics using routine and profiled ultrafiltration methods, addressing a significant research gap in the field. However, due to the condition's low prevalence and limited access to a suitable statistical population, further replication of this intervention in diverse medical settings is warranted. This would enable a deeper exploration of disease dynamics, the efficacy of the ultrafiltration profile, and the underlying determinants of this complication, cautioning against broad generalizations of the study's outcomes.
5.1. Conclusions
The study's findings reveal that while both conventional methods and ultrafiltration profiling during hemodialysis sessions led to an increase in blood pressure, the utilization of the ultrafiltration profile method demonstrated superior control over the rise in average systolic and diastolic blood pressure compared to the routine approach. Consequently, healthcare practitioners, particularly physicians and nurses specializing in hemodialysis care, are encouraged to consider employing the ultrafiltration profile method with a linear configuration featuring a negative slope and interval profile, and minimal sodium, for patients with a history of high blood pressure during hemodialysis sessions.