1. Background
Voiding dysfunction in pediatric patients involves urinary symptoms, including incontinence, frequency, urgency, or hesitancy. It is an abnormal urination pattern for a child's age, such as nocturnal urination in a 10-year-old or daytime urinary control transition in infants of 18 - 36 months. This condition can be distressing for parents and children and may cause significant morbidity if not treated (1, 2).
During the initial years of life, the bladder transitions from involuntary voiding to voluntary control. Voiding dysfunction primarily arises from functional disturbances, which can be due to either a malfunction of the lower urinary tract or delayed maturation of the central nervous system. This dysfunction can be categorized into neurogenic bladder dysfunction and non-neurogenic bladder dysfunction. Intriguingly, urinary disorders, frequently of undetermined origin, are prevalent in children who do not exhibit anatomical or neurological abnormalities, ranging from 20% to 50% (1, 3, 4).
The alleviation of symptoms and the prevention of kidney damage are of priority in managing bladder dysfunction in children. Treatment should take into account multiple factors, including the underlying cause (behavioral included), the patient's age, the duration and severity of symptoms, the motivation and attention span of the patient and their family, as well as potential risk factors (e.g., recurrent urinary tract infections or vesicoureteral reflux) (5-7).
The age of 0-6 years represents a critical period for child development, during which children learn to express their emotions, particularly in response to unfulfilled desires. Tantrums, marked by emotional outbursts, such as stubbornness and crying, are most common between the age of 2 - 3 years. Environmental factors, psychological influences, and parenting styles shape these reactions. While some level of restrictive parenting might be required, teaching self-control can empower children to respond to stress more positively (8).
Effective child-rearing techniques encompass diverse methods, such as time-outs, depriving privileges, modeling proper behavior, and instructing about the relationship between actions and consequences. As children mature and enhance their ability to communicate emotions, the instances of feeling anger tend to diminish. This decline mirrors the growth of emotional intelligence and the child's capacity for emotional regulation (8, 9).
This research explores the potential relationship between tantrums and urinary disorders in children. The findings could be of value because the timely treatment of urinary disorders can reduce complications, and tantrums are common in children. If a relationship between tantrums and urinary disorders is found, the study will recommend that doctors consider not only urinary issues but also children's behavior and tantrums. This approach may lead to a more comprehensive understanding and management of urinary and behavioral problems in pediatric patients.
There is currently limited evidence linking tantrums and voiding dysfunction in children, although both may relate to underlying behavioral, emotional, and medical issues, family dynamics, and parenting styles. Therefore, this research evaluates the potential relationship between these two conditions. Given the importance of timely urinary disorder treatment and the commonality of tantrums in children, these findings could be significant. If a substantial link between tantrums and urinary disorders is observed, the study will suggest doctors address both urinary issues and children's behavior and tantrums.
2. Objectives
This approach leads to more holistic pediatric patient care, potentially resulting in more effective interventions and improved well-being.
3. Methods
3.1. Participants and Procedures
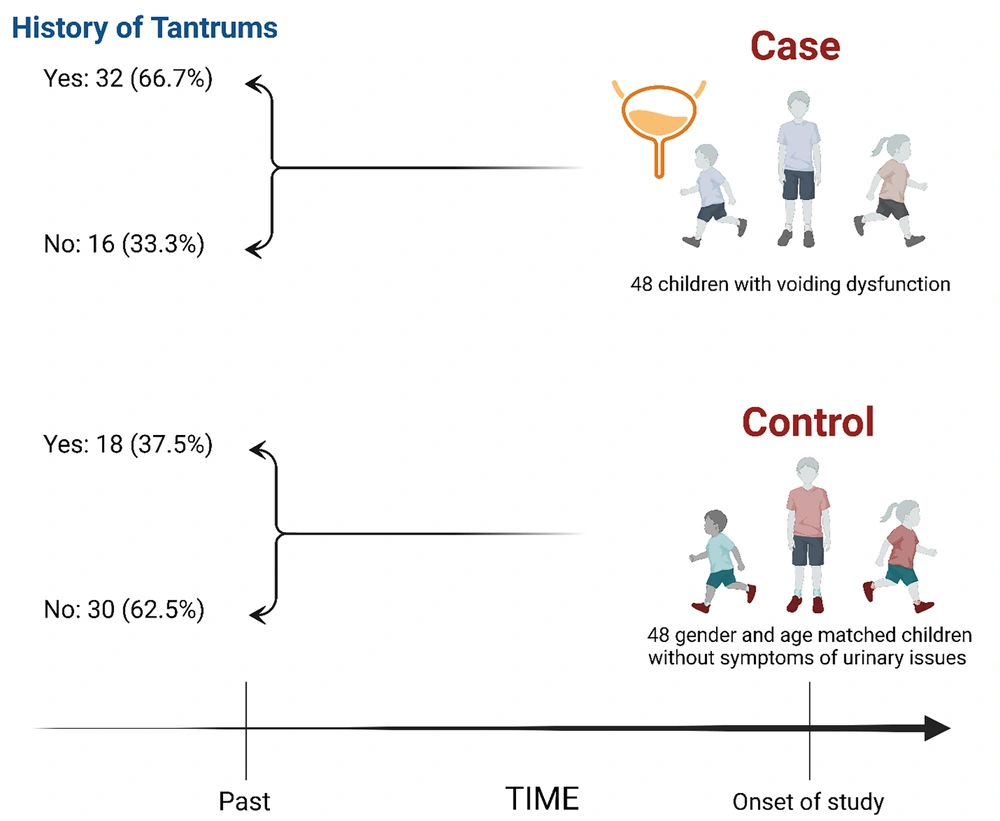
This case-control investigation was conducted at the Children's Clinic of Amir Kabir Hospital on patients who visited the clinic to be screened for thyroid function disorders. Children aged four and older exhibiting daytime urinary incontinence symptoms were evaluated. Parents received information about tantrums, and upon obtaining informed consent, their children were enrolled as cases in the study. For each case, a gender- and age-matched child without the symptoms of urinary issues was chosen as a control. Parents of 96 children—48 with urinary disorders and 48 healthy—completed a questionnaire on tantrum behavior. The exclusion criteria for both groups were the lack of consent to continue participating in the study. See Figure 1.
3.2. Measures
Voiding dysfunction was ascertained based on the patient's medical history. The clinical criteria for evaluating daytime voiding dysfunction encompassed incontinence, frequency, decreased urination, urgency, and a burning sensation. Tantrums were identified using a questionnaire derived from the Parents' Experience of Temper Tantrums in Children (PETTC). This questionnaire contained ten symptomatic inquiries: Screaming, stomping, kicking, head banging, and biting. A symptom lasting over one minute or deemed as "always" or "often" by the mother was classified as a tantrum. Conversely, the absence of these symptoms or their rare or occasional occurrence was not classified as a tantrum (10).
3.3. Statistical Analysis
Quantitative data were analyzed as mean and standard deviation, while qualitative data were presented as numbers and percentages. The Kolmogorov-Smirnov test was used to assess the normality of the quantitative variables. Moreover, the independent t-test or Mann-Whitney U test was applied for mean comparisons, and the chi-square test was utilized for the qualitative correlations. All analyses were conducted at a 95% confidence level and 5% alpha error using SPSS version 23 to ensure an accurate evaluation of the potential link between tantrums and urinary disorders in the studied pediatric population.
4. Results
We randomly selected 96 children over four years of age, with 48 participants having urinary disorders (case group) and 48 being healthy (control group). None of the included participants met the exclusion criteria. The average age of the children was 6.54 ± 1.71 years, with a range of 4 - 11 years. We found no statistically significant difference between the average age of the case and control groups (P = 1). Both groups included an equal number of boys and girls (24 of each, accounting for 50% of each group), indicating no significant gender difference between the two groups (P = 1). In the case group, 32 children (66.7%) experienced tantrums, while in the control group, 18 children (37.5%) had tantrums. Comparing the prevalence of tantrums in the two groups using the chi-square test revealed that tantrums were significantly more common in children with voiding dysfunction than in the control group (P = 0.004).
The relationship between voiding dysfunction and each of the ten questions in the PETTC questionnaire was assessed using the chi-square test. The analysis revealed that screaming (P = 0.016) and throwing things (P = 0.022) significantly affected the presence of voiding dysfunction. Other behaviors, including crying, hitting parents or siblings, throwing self on the floor, stomping feet, breaking things, biting, and kicking, demonstrated no significant association with the presence of voiding dysfunction (Table 1).
| Variables | Case | Control | P-Value |
|---|---|---|---|
| Screaming | 21 (43.8) | 10 (20.8) | 0.016 |
| Crying | 11 (22.9) | 11 (22.9) | 1.0 |
| Hitting | 9 (18.8) | 8 (16.7) | 0.789 |
| Throwing themselves on the floor | 2 (4.2) | 1 (2.1) | 0.500 |
| Stomping feet | 10 (20.8) | 6 (12.5) | 0.273 |
| Breaking things | 0 (0.0) | 1 (2.1) | 0.315 |
| Banging head against something | 0 (0.0) | 0 (0.0) | null |
| Throwing things | 5 (10.4) | 0 (0.0) | 0.022 |
| Biting | 1 (2.1) | 1 (2.1) | 1.0 |
| Kicking | 10 (20.8) | 6 (12.5) | 0.273 |
a Values are presented as No. (%).
5. Discussion
Our research delineates a compelling connection between pediatric voiding dysfunction and tantrums, suggesting a potential interplay between physiological and behavioral challenges in children. Understanding the multifaceted nature of these linked phenomena is essential for ensuring a holistic approach to pediatric care. Our analysis revealed a significant difference in tantrum frequency between the study groups, establishing a direct correlation between voiding dysfunction and tantrums in children. This relationship underscores the importance of integrating urinary and behavioral considerations when treating children with voiding dysfunction, advocating for a more comprehensive and practical approach.
The established correlation between voiding dysfunction and tantrums hints at an intertwined relationship between a child's physiological well-being and emotional and behavioral responses. The distress and discomfort from urinary issues might exacerbate or induce emotional outbursts in children. Conversely, behavioral challenges might aggravate urinary dysfunction due to the stress they cause (11). In examining the link between ten individual tantrum symptoms and daytime voiding dysfunction, only two specific behaviors, screaming and throwing things, demonstrated a significant difference between children with urinary incontinence compared to the control group. However, other behaviors, such as crying, hitting, kicking, and breaking things, were observed in healthy children and those with urinary disorders, with no significant difference between the groups.
The conspicuous association of some behaviors, such as screaming and throwing things, with voiding dysfunction is notable. One theory might be that these specific manifestations of tantrums represent higher intensity or acute distress. Such behaviors might serve as clear indicators for clinicians to investigate underlying physiological issues, namely urinary disorders. Salehi et al. studied 180 children with primary enuresis and an equal number of healthy children aged 7 - 17 with similar demographics. The diagnosis was based on DSM IV-TR, and the results showed a significant difference in general anxiety disorder frequency between the groups (P = 0.005), highlighting a link between primary enuresis and anxiety. Similarly, in our investigation on daytime urinary incontinence and tantrums, a significant relationship was found between these factors in children, underscoring the complex interplay between emotional and physiological aspects of children's health (12). Mahjani et al. found a relationship between hyperactivity and urinary symptoms, aligning with our conclusion linking tantrums and similar symptoms (13). Dourado et al. also reported relationships between behavioral problems and urinary disorders, consistent with our findings but focusing specifically on tantrums (14).
5.1. Limitations
This study highlights the need for broader, more diverse studies for enhanced generalizability. Data was gathered using a parental questionnaire, potentially introducing bias due to parents' perceptions. While the case-control study design shows associations, it does not confirm causation, warranting further prospective or interventional research. The current research might overlook confounding factors, such as psychological conditions or family dynamics. The findings of the present study may only be generalized to some cultures as it is conducted in a specific locale. Furthermore, focusing on children aged four and up, the exclusion of younger kids, known to throw tantrums frequently, might omit valuable insights. The PETTC questionnaire may not reveal all the nuances or types of tantrums children might display. Despite these constraints, the study provides essential initial insights into the potential relationship between these two conditions and their implications for pediatric care.
5.2. Conclusions
Considering tantrums in children up to age 4 years as normal, our findings recommend interventions for children aged four and older showing continued tantrums to prevent or improve daytime urinary incontinence, possibly through behavioral therapy. Based on the observed link, pediatricians treating children over four with daytime urinary incontinence should also assess and possibly treat tantrums concurrently. This integrated approach emphasizes the interplay between behavioral disorders and urinary symptoms in the clinical care of affected children.