1. Background
Coronavirus disease 2019 (COVID-19), first detected in China, has spread globally, resulting in the ongoing coronavirus pandemic and causing millions of human deaths (1, 2). Coronavirus disease 2019 manifestations are highly diverse. Common symptoms include fever, dry cough, tiredness, musculoskeletal pains, and breathing problems (2), while symptoms such as skin involvement, eyelid swelling, ocular discharge enhancement, and gastrointestinal problems are less frequently reported (3).
Noticeably, nearly all organ systems can be affected during or following a COVID-19 infection; in this regard, experiencing new symptoms or flare-ups of underlying diseases may be the only presentation of COVID-19. Lower urinary tract involvement, often characterized by increased urinary frequency and nocturia, has been reported in both mild and severe COVID-19-infected patients (4). Lower urinary tract symptoms (LUTS) comprise two main groups: Storage symptoms [e.g., overactive bladder (OAB), and stress urinary incontinence (SUI)] and voiding symptoms (e.g., hesitancy and other voiding difficulties) (5).
Hypotheses for COVID-19-related urinary symptoms include the increase of inflammatory cytokines released into the urine or their expression in the bladder, high distribution of the urothelial cell-surface protein angiotensin-converting enzyme 2 (ACE2) facilitating adhesion of the COVID-19 spike protein, and direct involvement of endothelial cells with the virus leading to diffuse endothelial inflammation (6, 7).
Assessing less-studied presentations of COVID-19 can deepen physicians' understanding of unusual infection symptoms and aid in better patient care (4, 8).
2. Objectives
Considering the importance of a thorough assessment of COVID-19, this study aims to investigate any new onset or worsening LUTS in patients with COVID-19.
3. Methods
This cross-sectional study was conducted on 88 laboratory-confirmed COVID-19 patients admitted to the Infectious Diseases Department of Yas Hospital, affiliated with Tehran University of Medical Sciences, from July to August 2020. Patients aged ≥ 18 years who were in the acute phase of COVID-19 (diagnosed with positive RT-PCR or antigen tests followed by seroconversion within two weeks from the onset of initial symptoms) (9) were included in the study. They were admitted to the department according to the centers for disease control and prevention indications (10).
Participants were excluded if they had neurological diseases, uncontrolled diabetes, urinary tract infections, high post-void residual volume, or any issues with their kidneys, bladder, or prostate. They were also excluded if they had an indwelling urinary catheter or were unwilling to participate in the study.
Overactive bladder was diagnosed based on the presence of urinary urgency without an infectious agent or other obvious pathologies (11). The presence of the COVID-19 virus was considered a likely cause of urgency and frequency in these patients. To investigate OAB symptoms, patients filled out the International Consultation on Incontinence-Overactive Bladder Questionnaire (ICIQ-OAB) (12) and the Overactive Bladder Symptom Score Questionnaire (OABSS) (13), both of which had been translated and validated into Persian. These were completed on the first day of admission. If a patient was unable to fill out the questionnaire, one of the authors assisted them.
The ICIQ-OAB questionnaire assesses OAB syndrome and its impact on quality of life, as well as evaluating treatment outcomes for both sexes. This questionnaire measures urgency, urge incontinence, urinary frequency, and nocturia, with scores ranging from 0 to 16; higher scores indicate more severe symptoms (14).
The OABSS questionnaire evaluates OAB symptoms through four questions on a single ordinal scale. The question scores range from 2 to 5, addressing daytime frequency (2 points), nighttime frequency (3 points), urgency (5 points), and urge urinary incontinence (5 points). The total score ranges from 0 to 15, with higher values indicating more severe symptoms.
Individuals were also assessed for SUI and any difficulties in voiding. Stress urinary incontinence is defined as the involuntary loss of urine during physical activity, sneezing, or coughing. Voiding dysfunction is characterized by symptoms such as hesitancy, slow stream, intermittent flow, a feeling of incomplete emptying, and post-micturition leakage (15).
Fluid management involved a prescribed daily maintenance dose, with additional replacement fluid administered upon physician request, based on the patient’s needs, such as being febrile. A frequency volume chart (FVC) was used to record urine leakage due to urgency or increased intra-abdominal pressure, as well as the frequency of urination for all patients over two consecutive days, aligning with the questionnaire scores. The study outcomes included the frequency of LUTS, quality of life score, the relationship between LUTS and quality of life in COVID-19 patients, and the relationship between LUTS and COVID-19 severity according to the percentage of lung involvement in CT scans.
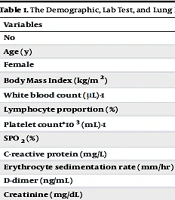
Additional data collected included age, sex, Body Mass Index (BMI), underlying diseases, and O2 saturation upon entering the emergency department. Laboratory tests conducted included complete blood count, C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), D-dimer, lactate dehydrogenase (LDH), creatine phosphokinase (CPK), ferritin, troponin (I and T), creatine kinase myocardial band (CKMB), and liver and kidney function tests. Lung involvement in CT scans was categorized as mild for less than 40% involvement, moderate for 40 - 60% involvement, and severe for more than 60% involvement.
3.1. Ethical Considerations
This study was approved by the Research Ethics Committees of the School of Medicine- Tehran University of Medical Sciences (Number: IR.TUMS.MEDICINE.REC.1400.856, Date: 2021-10-31).
3.2. Statistical Analysis
Qualitative variables were presented as numbers (percent), and quantitative variables as mean ± SD or median (interquartile range). The chi-square and Fisher's exact tests were employed to identify variations in proportions. After assessing normality with the Kolmogorov-Smirnov test, the independent t-test was used for parametric data and the Mann-Whitney U-test for non-parametric data. A P-value of less than 0.05 was considered statistically significant. Data were analyzed using IBM SPSS Statistics for Windows, version 19.0, Armonk, NY: IBM Corp.
4. Results
The mean age of the participants was 52.43 ± 13.98, ranging from 24 to 80 years. Of the patients, 36 (40.9%) were male, and 52 (59.1%) were female. Diabetes mellitus was reported in 15 (17%) patients, hypertension (HTN) in 17 (19.3%), hypothyroidism in 13 (14.8%), ischemic heart disease in 9 (10.2%), and cancer in 5 (5.7%). The mean peripheral capillary oxygen saturation percentage upon admission was 90.15 ± 5.18%. CT scans conducted on 72 patients demonstrated mild lung involvement in 31 (43.1%), moderate involvement in 30 (41.7%), and severe involvement in 11 (15.3%).
New onset of OAB symptoms was detected in 35 (39.8%) patients; the median ICIQ-OAB and OABSS scores were both 4 (range 3 - 8), for these patients. Worsening of pre-diagnosed OAB symptoms was detected in 4 (4.5%) patients; the median ICIQ-OAB and OABSS scores were 4.5 (range 2.5 - 5) and 3.5 (range 2.25 - 5.5), respectively. New onset SUI was reported in 17 (32.7%) women (no cases were detected in men), and voiding dysfunction was reported in one woman and two men.
According to the results presented in Table 1, there was no significant difference (P > 0.05) between patients with and without LUTS regarding demographic characteristics, laboratory tests, and lung involvement. However, new onset or worsening LUTS significantly affected the quality of life of the patients (P < 0.001) (Table 2).
| Variables | Lower Urinary Tract Symptoms | P-Value | |
|---|---|---|---|
| No | Yes | ||
| Age (y) | 52.50 ± 15.39 | 52.34 ± 12.17 | 0.958 |
| Female | 25 (51) | 27 (69.2) | 0.126 |
| Body Mass Index (kg/m2) | 29.41 ± 4.89 | 28.53 ± 4.88 | 0.421 |
| White blood count (μL)-1 | 9729.17 ± 2005.84 | 7421.05 ± 548.34 | 0.320 |
| Lymphocyte proportion (%) | 15.59 ± 7.55 | 16.39 ± 10.00 | 0.682 |
| Platelet count*103 (mL)-1 | 200.74 ± 81.91 | 207.23 ± 73.36 | 0.750 |
| SPO2 (%) | 89.46 ± 5.28 | 91.03 ± 4.98 | 0.165 |
| C-reactive protein (mg/L) | 80.18 ± 52.16 | 78.95 ± 52.81 | 0.915 |
| Erythrocyte sedimentation rate (mm/hr) | 32.97 ± 26.68 | 40.68 ± 25.01 | 0.221 |
| D-dimer (ng/mL) | 884.92 ± 137.91 | 750.87 ± 169.10 | 0.538 |
| Creatinine (mg/dL) | 1.17 ± 0.50 | 1.10 ± 0.22 | 0.450 |
| Aspartate transaminase (U/L) | 49.45 ± 4.57 | 60.91 ± 13.91 | 0.438 |
| Alanine transaminase (U/L) | 47.83 ± 5.12 | 54.44 ± 9.80 | 0.522 |
| Alkaline phosphatase (U/L) | 265.80 ± 118.60 | 265.50 ± 150.20 | 0.992 |
| Lactate dehydrogenase (U/L) | 708.68 ± 259.91 | 633.54 ± 258.57 | 0.212 |
| Lung involvement | 0.473 | ||
| < 40% | 16 (38.1) | 15 (50.0) | |
| 40 - 69% | 20(47.6) | 10 (33.3) | |
| > 70% | 6 (14.3) | 5 (16.7) | |
| Variables | Lower Urinary Tract Symptoms | P-Value | |
|---|---|---|---|
| No | Yes | ||
| ICIQ-OAB total score | 1.51 ± 0.35 | 5.07 ± 0.50 | < 0.001 |
| Bother of LUTS | 1.30 ± 0.63 | 10.25 ± 1.36 | < 0.001 |
| OABSS total score | 1.38 ± 0.34 | 5.20 ± 0.56 | < 0.001 |
z Abbreviations: ICIQ-OAB, International Consultation on Incontinence- Overactive Bladder Questionnaire; LUTS, lower urinary tract symptoms; and OABSS, Overactive Bladder Symptom Score.
5. Discussion
The diagnosis of COVID-19 can be challenging since patients often present with vague and non-respiratory complaints, along with symptoms involving multiple organ systems. For example, a wide variety of neurological complications have been observed in COVID-19-infected patients, including headaches, loss of the sense of smell, loss of consciousness, central nervous system infections, and neuropathy (16, 17).
Our study revealed that urinary symptoms were the only initial symptom in 31.8% of cases or part of the initial symptoms. This finding aligns with research by Mumm et al., which suggests increased urinary frequency secondary to viral cystitis as a potential symptom of COVID-19 (8). A previous study also reported that patients may present several weeks after discharge (10 - 14 weeks post-discharge) with new or worsening urinary symptoms, with a prevalence of up to 71%. These researchers similarly noted that these symptoms adversely impacted the patients' quality of life, with worsened scores compared to pre-COVID conditions (4). Despite results consistent with ours, one major issue in their study is the potential for recall bias, as they did not assess patients during hospitalization but rather 10 - 14 weeks post-discharge, asking about pre-COVID symptoms at that time. In addition to COVID-19 infection, new onset or recent worsening of urinary frequency, nocturia, urgency, and urgency incontinence have also been reported in other infectious diseases, such as human immunodeficiency virus (HIV) (18) and human T cell lymphotropic virus-1 (HTLV-1) infection (19).
Similar to Daryanto et al. (20), our research found that the most common LUTS in COVID-19-infected patients are those associated with OAB. While our study found no significant association between demographic factors, laboratory tests, disease severity, and LUTS, Daryanto et al. (20) identified significant correlations between LUTS and factors such as male sex, age over 50, comorbidities, and higher degrees of COVID-19 infection. The differences between these findings might be attributed to the use of different study questionnaires (international prostate score was used in the Daryanto et al. study) and the inclusion of COVID-19-infected patients ranging from asymptomatic to severely symptomatic.
Previous research (4, 21) has shown that an OAB is associated with increased patient fatigue and sleep disorders, which further contribute to COVID-19 morbidity. Therefore, symptomatic management of urinary complications could reduce the disease burden by alleviating the fatigue caused by frequent voiding throughout the day, aligning with our findings.
Reporting the presence of RNA virus, hematuria, and pyuria in urine analysis is a poor prognostic factor associated with a higher mortality rate in COVID-19-infected patients. Additionally, RNA virus shedding in urine can be detected after the acute phase of the disease, when the patient is recovering from COVID-19 (22, 23).
Considering our significant insights into this novel virus, this study had several limitations. These include a limited sample size, the single-center nature of the study, not assessing outpatients, and not following participants after discharge. Moreover, we did not measure other pro-inflammatory markers such as Interleukin-6 or 8 in the patients' urine samples. Therefore, further studies are needed to compare LUTS in general populations without COVID-19 in the same admitted ward as COVID-19 cases.
5.1. Conclusions
According to the results, this study demonstrated that LUTS could be the only initial symptom of COVID-19 or part of the complex initial symptoms of the disease. Additionally, given the unclear impact of LUTS on COVID-19 prognosis, further research is needed to investigate the molecular pathogenesis of urinary frequency, the increased risk of these symptoms later in life, and optimal pharmacological therapy for these patients.