1. Background
Although prostate-specific antigen (PSA) is the most commonly used tumor marker for prostate cancer detection, it has low specificity for cancer and cannot differentiate between indolent and significant prostate cancer (1, 2). The risk of prostate cancer in men with elevated PSA levels is estimated to be approximately 30%, with a range of 24 - 48% (3, 4). An increase in serum PSA is likely the result of cellular structure disruption in the prostate gland (5, 6).
Therefore, PSA can be elevated in many benign conditions unrelated to prostate cancer that are caused by any damage to the barrier afforded by the basal layer and basement membranes, such as in cases of prostate cancer, benign prostatic hyperplasia (BPH), prostatitis, as well as in prostate manipulations like prostate biopsy (7-10).
Urinary catheterization is one of the most common procedures in urology practice, often performed in patients with acute urinary retention (AUR). Despite some evidence suggesting an association between catheterization and prostatic inflammation with an increase in PSA levels (11-13), many studies have not shown such an increase, and the results are varied (14-16). Factors such as the duration of catheterization, pre-existing prostate conditions, and whether patients have AUR may influence these findings.
2. Objectives
We conducted this study to examine the influence of AUR on serum PSA and changes in PSA levels after urethral catheterization in men with AUR.
3. Methods
Between June and September 2023, a total of 56 men with BPH who presented to Razi Educational Hospital in Rasht and underwent urethral catheterization due to AUR were included in this prospective study using a quasi-experimental design to assess the PSA level before and after catheterization. Patients with a history of prostate cancer, pelvic urogenital operations, any urological manipulation within 6 weeks, abnormal digital rectal examination (DRE), or treatment with 5α-reductase inhibitors were excluded from the study. Written informed consent was obtained from each participant, and the research was conducted in accordance with the World Medical Association's Declaration of Helsinki.
All patients in our study underwent atraumatic urethral catheterization after sufficient lubricant was applied to the urethra. Blood samples were simultaneously obtained to measure serum PSA levels and free/total PSA ratios at the time of catheterization, and then 1 and 3 days after urethral catheter insertion. A PSA level of ≤ 4 ng/mL was considered normal. Additionally, abdominal ultrasonography was performed to calculate prostate volume and PSA density. Urine output after catheterization (UOAC) was also recorded. Urine samples were collected at the time of catheterization to rule out urinary tract infection (UTI). Data from patients who had a positive urine culture were excluded from the analysis.
3.1. Statistical Analysis
Considering a 95% confidence level, 90% power, and a dropout rate of 30%, a sample size of 15 patients was calculated based on the results of a study by Erdogan et al. (16).
Data were analyzed using IBM SPSS Statistics for Windows, version 24.0. Values of variables are presented as mean ± SD, median, minimum, maximum, and mean rank. The Kolmogorov-Smirnov test was used to measure the distribution of the variables. Repeated measures ANOVA was applied for all statistical analyses. However, the Mann–Whitney U test was used to compare differences in baseline total PSA levels between two groups based on age, prostate volume, and UOAC. Statistical significance was determined by P-values of ≤ 0.05.
4. Results
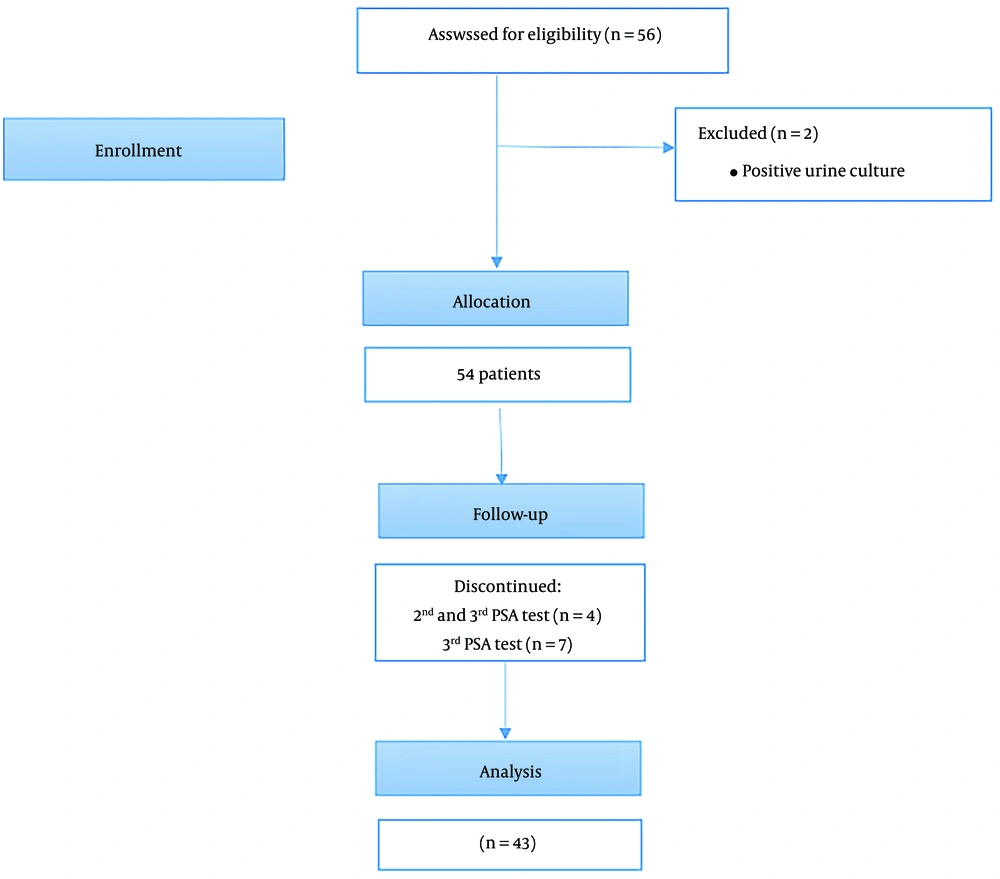
Of the 56 enrolled patients, 2 had a positive urine culture and 11 did not return for the 2nd and/or 3rd PSA test. In total, the data of 43 patients were analyzed (Figure 1). The mean age of the patients was 69.05 ± 9.45 years, ranging from 46 to 86. The mean prostate volume and UOAC were 60.51 ± 26.35 g (range 23 to 130) and 844.04 ± 341.66 mL (range 450 to 2300), respectively.
The mean baseline total PSA was 12.59 ± 17.71 ng/mL, with a median of 6.30 ng/mL. After 1 day of catheterization, the mean total PSA level increased to 13.73 ± 19.83 ng/mL (median = 4.80 ng/mL) and then declined to 11.57 ± 17.70 ng/mL (median = 4.40 ng/mL) after 3 days of catheterization (P = 0.38). As shown in Table 1, changes in free/total PSA and PSA density during these periods were not statistically significant (P = 0.44; 0.26, respectively).
| Variables | Before Catheterization | After 1 Day | After 3 Days | P-Value b |
|---|---|---|---|---|
| tPSA | 12.59 ± 17.71 | 13.73 ± 19.83 | 11.57 ± 17.70 | 0.38 |
| f/tPSA | 0.30 ± 0.13 | 0.25 ± 0.13 | 0.60 ± 2.40 | 0.44 |
| PSA density | 0.23 ± 0.38 | 0.24 ± 0.37 | 0.21 ± 0.34 | 0.26 |
Serum Prostate-Specific Antigen (PSA), Free/Total PSA and PSA Density Alteration Before and After the Catheterization a
No significant differences were found between mean baseline total PSA levels in two age groups (≤ 65 and > 65 years) (P = 0.150), prostate volume (≤ 60 and > 60 g) (P = 0.960), and UOAC (≤ 800 and > 800 mL) (P = 0.970) as shown in Table 2.
| Variables | Baseline tPSA | P-Value b |
|---|---|---|
| Age group | 0.150 | |
| ≤ 65 | 18.23 | |
| > 65 | 24.02 | |
| Prostate volume | 0.960 | |
| ≤ 60 | 22.07 | |
| > 60 | 21.88 | |
| UOAC | 0.970 | |
| ≤ 800 | 21.44 | |
| > 800 | 21.58 |
Baseline Total Prostate-Specific Antigen (PSA) in Two Groups of Age, Prostate Volume and UOAC a
Regarding the results in Table 3, changes in total serum PSA were compared in two groups based on their baseline total PSA level. No significant differences were found between PSA levels before, 1 day, and 3 days after catheterization in groups with total PSA ≤ 4 and total PSA > 4 (P = 0.37; 0.22, respectively).
| Variables | Before Catheterization | After 1 Day | After 3 Days | P-Value b |
|---|---|---|---|---|
| tPSA ≤ 4 | 2.20 ± 1.38 | 2.19 ± 1.58 | 2.91 ± 3.79 | 0.37 |
| tPSA > 4 | 21.62 ± 20.34 | 23.77 ± 22.84 | 19.11 ± 21.40 | 0.22 |
Serum Prostate-Specific Antigen (PSA) Alteration Before and after the Catheterization in two Groups with Baseline PSA ≤ 4 and Baseline PSA > 4 a
5. Discussion
Prostate-specific antigen is an androgen-regulated serine protease produced by both prostatic luminal epithelial cells and prostate cancer cells (17). Prostate biopsies are often performed to determine the cause of elevated PSA levels. Reports indicate that biopsies showed no evidence of prostate cancer in 47% of men with PSA levels above 10 ng/mL (18). Besides prostate cancer, any damage to the barrier provided by the basal layer and basement membranes within the normal gland may increase PSA levels in the blood (8).
Acute urinary retention is a condition characterized by a sudden inability to empty the bladder, which can be distressing for patients and often requires immediate medical intervention. The etiology of AUR is poorly understood, but prostate inflammation has been suggested as a possible underlying cause (19, 20). Catheterization is a common intervention performed in these patients to relieve urinary obstruction and has been associated with prostatic inflammation. Consequently, it is expected that patients with BPH who undergo catheterization due to AUR will have elevated PSA levels (21-23). However, a study conducted by Anand and Gupta on 80 patients with AUR who underwent catheterization found that PSA levels did not increase following AUR and showed no changes after catheterization (14). On the other hand, Aliasgari et al. (23) reported that the average PSA at the time of AUR and 2 weeks after bladder catheterization was 9.8 and 5, respectively, indicating that AUR can cause an approximately 2-fold increase in serum PSA levels.
In our study, we demonstrated that in patients with urinary retention due to BPH, an increase in PSA levels occurs prior to catheterization, and there was no significant change in PSA levels after urethral catheter insertion. This indicates that atraumatic catheterization has no effect on PSA levels.
The exact reason for the increase in PSA levels in patients with AUR before catheterization is not well-defined. Many researchers consider inflammation as the primary cause of elevated PSA levels (22, 24). Kefi et al. (22), in a retrospective case-control study, found chronic prostatic inflammation in 56% of transurethral resection of the prostate (TURP) specimens from AUR patients and 37% from non-AUR patients. In the AUR group, patients with prostatic inflammation had significantly higher mean PSA levels compared to those without, suggesting that prostatic inflammation significantly contributes to AUR. Conversely, Antunes et al. (25) argued that prostatitis cannot be the main factor in PSA elevation in patients with AUR. In their study, only 1.5% and 24.7% of patients showed acute and chronic prostatitis, respectively, in histological diagnoses. However, it should be noted that this study only examined prostate biopsy samples, which are fewer in number compared to surgical prostate samples. Furthermore, while some consider catheterization alone to contribute to inflammation and increasing PSA levels, others believe that this procedure does not contribute to the increase, and the main cause of elevated PSA is AUR itself. Supporting this view are data indicating an increase in PSA levels prior to catheterization and a subsequent decrease after a few days (21, 23, 26). Our findings also confirm the results of these studies.
In the present study, PSA levels in the group with a normal baseline PSA value (≤ 4.0 ng/mL) remained within the normal range throughout the measurement period after catheterization without any significant difference (P = 0.37). Also, no statistically significant changes were noted in serum PSA levels in the group with baseline PSA above 4 ng/mL.
Consistent with the results of our study, Matzkin et al. (27), in a prospective study with a mean catheter duration of 5.5 days, showed that changes in PSA following prolonged catheterization were not clinically significant, neither in men with a normal baseline PSA nor in those with an above-normal baseline PSA. However, Faris et al. (28) observed that catheterization in patients with AUR due to BPH only increases PSA levels in patients who had a higher baseline PSA level, and in individuals with normal baseline PSA, it does not cause a significant change.
In a study investigating the relationship between AUR and PSA concentration conducted on 34 patients who underwent suprapubic cystostomy, a dramatic increase in serum PSA levels was observed following urinary retention, with a subsequent reduction of over 50% after 48 hours. This study also indicates that the increase in PSA occurs during the process of urinary retention, given that none of the patients underwent urethral catheterization (26). However, in our study, PSA levels did not show a significant change after 3 days, suggesting the hypothesis that urethral catheterization may slow down the rate of PSA decline following urinary retention.
We also examined the effects of age, prostate volume, and UOAC on the serum PSA level in our study. Our findings showed that baseline PSA in patients with AUR is not affected by age, prostate volume, or UOAC. Although a positive correlation between serum PSA, age, and prostate volume has been confirmed (29, 30), it seems that elevated PSA before catheterization in patients with AUR is not influenced by age or prostate volume.
This study had some potential limitations. First, we were unable to determine whether PSA levels return to normal after catheter insertion and how long it would take to normalize. It has been reported that the effect of increased PSA due to urinary retention can persist for up to 2 weeks (23, 31). Second, the small sample size is a severe limitation of our study, although it was estimated to be sufficient with 85% power and a 5% significance level. Therefore, further studies are necessary to confirm these results.
5.1. Conclusions
In this study, we demonstrated that in patients with BPH who underwent urethral catheterization due to AUR, there is an initial elevation in PSA levels. However, no significant changes in total PSA levels or the free/total PSA ratio were observed after catheterization. Additionally, prostate volume, age, and UOAC did not influence the baseline PSA levels.