1. Background
Congenital or acquired urinary tract obstruction is the primary cause of chronic renal failure in children. Ureteropelvic junction obstruction (UPJO) is the most common congenital obstructive lesion of the urinary tract system in children, accounting for 35 - 50% of all significant prenatally detected uropathies and 10 - 35% of all pathological prenatal hydronephrosis. The prevalence of this abnormality is 1 in 1500 children. The etiology of UPJO is multifactorial and polygenic (1-3).
Currently available investigations, such as renal ultrasonography, radionuclide renal scan, and plasma creatinine concentration, are not always conclusive and accurate for diagnosing obstructive nephropathy, emphasizing the need for a new, noninvasive, and simple diagnostic biomarker in childhood (3, 4).
Recently, the evaluation of urinary biomarker excretion has gained interest as an adjunctive procedure to radiographic examination (5). Application of renal biomarkers may favor early identification of renal injury secondary to upper urinary tract obstruction (UTO), allowing for optimal therapeutic options and preventing or decreasing further renal damage. Additionally, these biomarkers might have higher prognostic value than serum creatinine for predicting long-term renal outcomes (1).
Urine neutrophil gelatinase-associated lipocalin (uNGAL), also known as lipocalin-2, siderocalin, and uterocalin, is one of the early and noninvasive biomarkers of acute kidney injury and progression to chronic kidney disease (3). It is a 25-KDa protein secreted by different types of human tissues, including the gastrointestinal tract, respiratory tract, and renal tubules. Increased uNGAL excretion has been suggested as a specific biomarker of genitourinary epithelial damage and impaired renal tubular reabsorption (6).
Urine neutrophil gelatinase-associated lipocalin has been identified as a potential diagnostic biomarker for pathologic conditions such as acute kidney injury, nephrotic syndrome, diabetic nephropathy, tubulointerstitial nephritis, IgA nephropathy, lupus nephritis, polycystic kidney disease, cyclosporine-A nephrotoxicity, contrast nephropathy, monitoring delayed graft function, and acute rejection after renal transplantation (3, 7).
Increased uNGAL excretion has also been reported in children with urinary tract infection, vesicoureteral reflux, reflux nephropathy, and obstructive uropathies (4, 8, 9).
Increased uNGAL concentration has been suggested as an independent predictive biomarker in children with urinary tract obstruction, especially those with differential renal function < 40%, due to increased intratubular pressure, renal tubular ischemia, and chronic tubulointerstitial damage (3, 4).
2. Objectives
The aim of this study was to investigate the alteration of uNGAL and uNGAL/Cr excretion as non-invasive diagnostic biomarkers of obstructive UPJO, and to evaluate their sensitivity and specificity for predicting obstructive UPJO.
3. Methods
3.1. Design
A cohort study was performed on 47 children (32 males, 15 females) with obstructive UPJO, diagnosed and managed in two pediatric surgery departments between 2020 and 2022. A control group of 47 healthy children (40 males, 7 females) with normal renal ultrasound was also included.
Renal ultrasonography for the initial diagnosis of hydronephrosis (HN) was conducted by a single pediatric radiologist using a SSA–280A scanner (Toshiba, Tokyo, Japan) equipped with a 3.5-MHz probe. Grading of HN was performed according to the Society for Fetal Urology (SFU) classification:
- Grade 0: No dilatation.
- Grade I: Renal pelvic dilatation with no calyceal dilatation and no parenchymal atrophy.
- Grade II: Renal pelvic and calyceal dilatation with retained pelvicalyceal pattern and no parenchymal atrophy.
- Grade III: Moderate renal pelvic dilatation, calyceal blunting, and mild cortical thinning.
- Grade IV: Gross renal pelvic dilatation, calyceal ballooning, and renal atrophy with cortical thinning.
Voiding cystourethrography (VCUG) was performed in all children to exclude vesicoureteral reflux. A renogram with 99mTc-DTPA diuretic renal scan was conducted in cases with negative VCUG to identify UPJO. Due to low GFR in newborn infants, isotope scanning was scheduled after the neonatal period. Obstructive UPJO was defined as pelvicalyceal isotope accumulation unresponsive to furosemide injection. Non-obstructive HN was represented as prolonged half-life clearance (t½) of radioisotope on DTPA renal scan, responsive to diuretics. A differential renal function of less than 45% was defined as decreased renal function.
Children aged 1 month to 14 years with obstructive UPJO identified by isotope renal scan and normal renal function estimated by the Schwartz formula were included in this study. Exclusion criteria included associated urologic abnormalities such as vesicoureteral reflux, non-obstructive UPJO, ureterovesical junction obstruction, lower urinary tract abnormalities, bladder dysfunction, history of urinary tract surgery, urolithiasis, UTI within the past 3 months, concomitant infectious or inflammatory disorders, ongoing antibiotic treatment, and increased blood pressure.
Centrifuged urine samples of children with complete obstruction were stored within 4 hours of collection at -80°C. UNGAL was measured using a commercially available ELISA kit (BioPorto Diagnostics, Gentofte, Denmark) according to the manufacturer's instructions, expressed as ng/ml, and normalized by urine creatinine (Cr).
3.2. Statistical Analysis
Analysis was performed using SPSS version 27 (SPSS, Chicago, IL) and MedCalc version 15.4. Categorical variables were expressed as frequency and percentage. Statistical measures such as mean ± SD and percentiles were used for numerical variables. Categorical variables were compared between the two groups using the chi-square test. Non-normally distributed variables were compared using the Mann–Whitney U test. Correlation between variables was performed using the Spearman correlation test. The receiver operating characteristic (ROC) curve was used to determine the cut-off value of uNGAL and uNGAL/Cr with the highest sensitivity and specificity. P-values < 0.05 were considered significant.
4. Results
A total of 94 children (mean age: 24.14 ± 32.10 months) were included in this study. Of these, 47 patients had obstructive UPJO (cases), and 47 were normal healthy children (controls). Males outnumbered females in both groups (76.6% vs 23.4%), with no significant difference (P = 0.051). The mean age at the time of the study showed no significant difference between the two groups (P = 0.517). The majority of patients (68.8%) were identified during the prenatal period, while 31.2% were detected due to evaluation of UTI, or cyclic and acute abdominal pain. The left kidney was more frequently affected than the right kidney (55.6% vs 44.4%). About 75.6% of patients had severe HN.
In addition, mean uNGAL and uNGAL/Cr levels were significantly higher in children with UPJO compared to the control group (P < 0.001) (Table 1). Based on the non-normal distribution of these variables, Q1 and Q3 were also reported, showing that uNGAL and uNGAL/Cr were significantly higher in cases compared to the control group (P < 0.001) (Table 2).
| Variables | Case | Control | P-Value |
|---|---|---|---|
| Mean age (m) | 25.50 ± 34.59 | 25.79 ± 29.73 | 0.517 |
| Gender (M/F %) | 68.1/31.9 | 85.1/14.9 | 0.051 |
| Mean uNGAL (ng/mL) | 92.37 ± 132.38 | 4.84 ± 5.34 | < 0.001 |
| Mean uNGAL/Cr (ng/mg) | 8.09 ± 9.38 | 0.42 ± 0.46 | < 0.001 |
Comparison of Variables in Two Groups of Patients a
| Variables (median) | Case | Control | P-Value | ||||
|---|---|---|---|---|---|---|---|
| Median | Q1 | Q3 | Median | Q1 | Q3 | ||
| UNGAL (ng/mL) | 2.30 | 0.05 | 10.85 | 43.00 | 17.00 | 101.00 | < 0.001 |
| UNGAL/Cr (ng/mg) | 0.11 | 0.01 | 0.95 | 1.28 | 4.61 | 9.60 | < 0.001 |
Comparison of Variables in two Groups of Patients (Median)
Binary logistic regression analyses showed that uNGAL [OR]: 1.42, 95% CI: 1.10 - 1.84, P = 0.008, and uNGAL/Cr [OR]: 2.98, 95% CI: 0.93 - 9.55, P = 0.049 were independent predictive markers of obstructive UPJO (Table 3).
| Variables | Univariate | Multivariate | ||
|---|---|---|---|---|
| OR (95% CI) | P-Value | OR (95% CI) | P-Value | |
| UNGAL (ng/mL) | 1.40 (1.9 - 1.66) | < 0.001 | 1.42 (1.10 - 1.84) | 0.008 |
| UNGAL/Cr (ng/mg) | 12.46 (3.106 - 49.55) | < 0.001 | 2.98 (0.93 - 9.55) | 0.049 |
Binary Logistic Regression Analysis of Variables for Predicting Obstructive Ureteropelvic Junction Obstruction
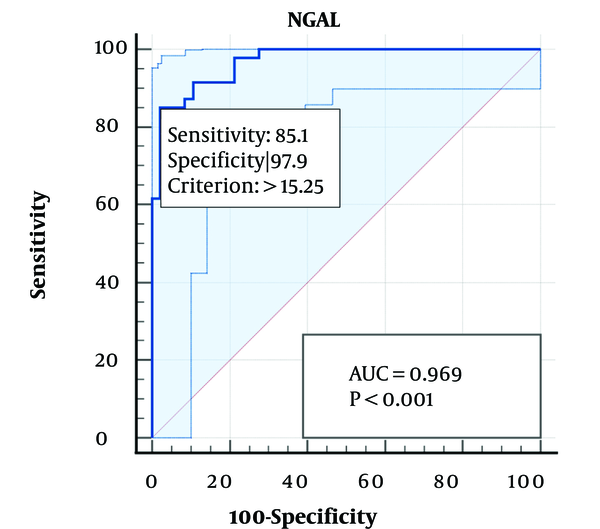
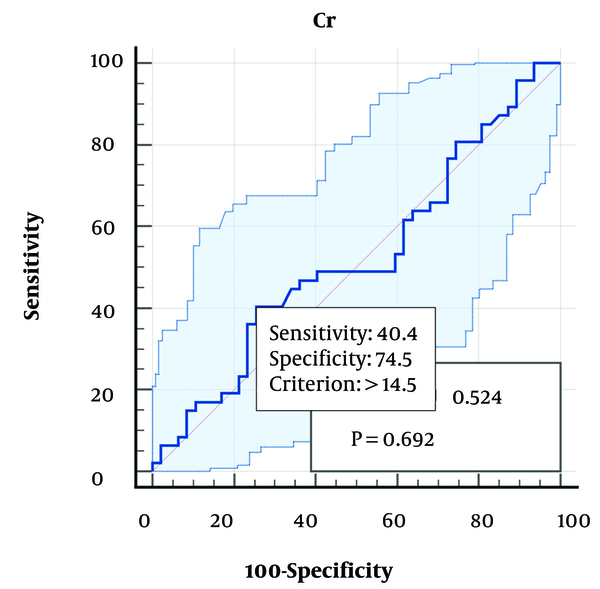
UNGAL had no significant correlation with severity, transit time (T1/2), and laterality of HN in our study. The optimal cutoff value of uNGAL (15.25 ng/mL) and uNGAL/Cr (1.08 ng/mg) had the highest sensitivity (85.11% vs 80.9%) and specificity (97.87% vs 95.7%) with significant accuracy (P < 0.001) for predicting obstructive UPJO, respectively (Table 4). The area under the curve (AUC) value from the receiver operating characteristic (ROC) curve analysis of uNGAL (0.969, P < 0.001, 95% CI: 0.911 - 0.994) and uNGAL/Cr (0.932, P ≤ 0.001, 95% CI: 0.860 - 0.973) are shown in Figures 1 - 2.
| Variables | Cutoff | Sensitivity | Specificity | AUC | 95% CI | Standard Error | P-value |
|---|---|---|---|---|---|---|---|
| UNGAL (ng/mL) | 15.25 | 85.11 | 97.87 | 0.969 | 0.911- 0.994 | 0.014 | < 0.001 |
| Cr (mg/dL) | 14.50 | 40.40 | 74.50 | 0.524 | 0.418- 0.628 | 0.060 | 0.692 |
| UNGAL/Cr (ng/mg) | 1.08 | 80.90 | 95.70 | 0.932 | 0.860- 0.973 | 0.024 | < 0.001 |
Receiver Operating Characteristic Curve Analysis of uNGAL for Predicting Obstructive Ureteropelvic Junction Obstruction
5. Discussion
Different tubular and glomerular biomarkers have been introduced for the diagnosis and management of various renal disorders. UNGAL is a biomarker expressed in neutrophil granules, monocytes, macrophages, and renal epithelial tubular cells. It is not detectable in a normal healthy kidney; however, increased uNGAL excretion has been reported in children with renal tubular damage, secondary to increased NGAL production and decreased NGAL reabsorption, corresponding to the severity of renal parenchymal damage. UNGAL has been identified as an early and sensitive biomarker of proximal tubular damage after acute kidney injury and chronic tubulointerstitial insults (6, 9). In addition, it has been suggested as a potential indicator of obstructive uropathy and renal damage in some studies.
In this study, uNGAL excretion was compared between two groups of children: Those with obstructive HN and a healthy control group. The majority of our patients were identified during the prenatal period with severe HN. UNGAL and uNGAL/Cr excretion were significantly higher in children with obstructive UPJO compared to the healthy controls, with no significant correlation to the severity and side of UPJO.
Bieniaś and Sikora found higher urinary NGAL excretion in patients with obstructive HN compared to those without obstruction, with a positive correlation to the severity of HN and deterioration of renal function. They suggested uNGAL as a promising biomarker of obstructive nephropathy (10).
UNGAL level was higher in obstructive nephropathies, with a good diagnostic profile in severe obstruction, compared to nonsurgical HN in some studies. They suggested uNGAL excretion as a valuable biomarker for anticipating timely surgical repair and predicting surgical response (11-14).
Madsen et al. showed significantly increased uNGAL excretion from obstructed kidneys compared to contralateral kidneys and healthy controls. UNGAL levels were higher in the perioperative and early postoperative phase and decreased after the first postoperative day. The authors did not observe a significant correlation between age and uNGAL excretion; however, there was a negative tendency (2).
Cost et al. identified increased uNGAL excretion in children with UPJO as a sensitive index for detecting proximal renal tubular damage, with a negative correlation to the relative renal function of the involved kidney, and normalized after surgical treatment. They indicated uNGAL as a noninvasive potential biomarker in patients at risk of decreased renal function, in addition to identifying the need for surgical repair (5).
McLeod et al. suggested that increased uNGAL excretion might continue due to ongoing tubular injury despite the relief of urinary obstruction, serving as an accurate biomarker for predicting chronic kidney damage in these patients (15).
Karakus et al. demonstrated that uNGAL levels were significantly increased preoperatively compared to the healthy control group and decreased significantly after surgical treatment, potentially predicting surgical outcomes. They found no significant difference in uNGAL concentration between the obstructive and non-obstructive groups undergoing conservative treatment, indicating the low value of uNGAL in distinguishing non-obstructive HN from obstructive dilation in unilateral HN, and highlighting the benefits of surgical treatment. Additionally, uNGAL was useful for detecting previous tubulointerstitial damage and for long-term postoperative follow-up (16).
Fendereski et al. showed a significant correlation between renal function deterioration and the prediction of surgical treatment in children affected by UPJO (17).
In Wasilewska et al.'s study, uNGAL excretion was higher in patients with obstructive UPJO than in the normal control group and non-obstructive HN, with an inverse correlation to decreased renal function, especially <40%, and compatible with the renal pelvic anteroposterior diameter of the involved kidney. They showed no correlation between uNGAL concentration and serum creatinine level or GFR (3).
However, Bolignano et al. showed a significant correlation between uNGAL excretion with serum creatinine or GFR in children with chronic kidney disease (18).
Meanwhile, uNGAL was not a significant predictor of urinary tract obstruction in Gerber et al.'s report. However, their study was performed with a small sample size of patients and needs a larger population (19). Similarly, uNGAL had no correlation with renal damage in obstructive UPJO and did not decrease after surgical treatment in other reports (20, 21).
In a meta-analysis by Sangeetha and Babu, uNGAL had 76% specificity and 77% accuracy for differentiating obstructive from non-obstructive pelvicalyceal dilatation. They recommended a panel containing uNGAL as the best diagnostic biomarker in children with obstructive UPJO (22). Similarly, uNGAL had high sensitivity and specificity with acceptable accuracy for the prediction of obstructive UPJO in our study.
5.1. Conclusions
The findings of our study suggest that uNGAL is a sensitive and noninvasive biomarker for predicting obstructive UPJO in children and should be considered an appropriate complement to radiographic or isotopic examinations of UPJO. The present study has some limitations. First, the relatively small number of patients does not allow for unequivocal conclusions. Additionally, uncorrected coding might have decreased the exact number of patients. Second, although we excluded known modifiers of urine NGAL excretion during sample collection, unknown biases might have affected the measurement of uNGAL. This issue necessitates further research on urine NGAL measurement. It is recommended to conduct multicenter studies with a larger number of patients to confirm the potential diagnostic application of uNGAL and its correlation with the severity and surgical outcomes of children with obstructive UPJO and renal parenchymal damage.