1. Background
Incidental renal findings are the most frequent extraspinal findings in lumbar MRI (33%), although they are the least reported findings (4%) (1, 2). Incidental findings (IF) in imaging modalities are usually asymptomatic abnormalities detected during radiological examinations that are irrelevant to the patient's chief complaint. Ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) frequently reveal cystic renal lesions. Epidemiological studies suggest that approximately one-third of people over 60 have unilateral or bilateral cystic renal masses (CRM).
Several studies have investigated extraspinal IF in lumbar spine MRI. The number of reported incidental findings in lumbar spine MRIs has increased in recent years following the implementation of the picture archiving and communication system (PACS) in most hospitals (3-6). The prevalence of extraspinal findings (ESFs) ranges from 22% to 68.7% (2, 7-9). Most IFs are benign, though their nature should be characterized to determine the risk and benefits (8). First, an image analysis is performed to confirm the renal mass. Poorly characterized renal masses should be evaluated in part because renal cell carcinoma (RCC) is most commonly diagnosed incidentally, and early disease detection can positively affect outcomes (10). The potential benefit of early RCC detection should be weighed against the risk of investigating or treating benign or small malignant renal masses of no clinical significance (11). Early detection and timely management of clinically significant incidental findings are associated with reduced morbidity and mortality.
Imaging modalities play crucial roles in the diagnosis, characterization, staging, treatment guidance, and post-treatment evaluation of RCC (12). The imaging-based approach to cystic renal masses has recently undergone a major revision. Based on the Bosniak classification version 2019 (BCv2019), CT and MRI are comparable regarding CRM classification, with no significant differences in diagnostic accuracy or reliability (13). MRI, and to some extent, ultrasound, is now included in the BCv2019. Magnetic resonance imaging is an important clinical modality for diagnosing cystic and solid renal masses. An unenhanced axial T2-weighted sequence often shows incidental renal lesions, but the characterization of these lesions in routine unenhanced MRI presents a diagnostic challenge. However, limited studies have been conducted on T2-weighted imaging features in lumbar spine MRI for incidental renal cysts.
2. Objectives
The present study aimed to assess the characterization of renal lesions in T2-weighted imaging of lumbar spine MRI and its ability to differentiate complex renal lesions from simple cysts.
3. Methods
The study was approved by the local university's ethics committee. Over 24 months, from March 2019 to March 2021, 206 renal lesions were prospectively identified in 206 patients. Patients with IV contrast allergies or contraindications for CT scans were excluded.
MRIs were performed using a General Electric 1.5 Tesla scanner (GE Medical Systems, Milwaukee, WI, USA) in a supine position. The studies included sagittal, axial, and coronal sections, including T1 and T2 sequences with a spine coil. The lumbar MRI protocol consisted of sequences of sagittal T1-weighted TSE images (TR/TE, 400/9 ms; slice thickness/interslice gap, 4/0.4 mm; NEX, 3), sagittal T2-weighted TSE images (TR/TE, 3000/120 ms; slice thickness/interslice gap, 4/0.4 mm; NEX, 3), and axial T2-weighted TSE images (TR/TE, 3000/110 ms; slice thickness/interslice gap, 4/0.4 mm; NEX, 3). Before performing the routine imaging sequences, scout images for lumbar spinal MRI were acquired. Axial section images were captured for lumbar MR imaging between the L1 and S1 vertebrae.
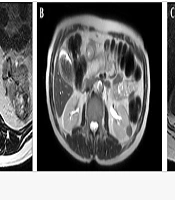
Patients with renal cysts on lumbar MRI with a minimum AP diameter of 1 cm were identified. The renal lesions were classified into simple cysts and complex lesions solely based on axial T2-weighted images. A complex renal lesion was described as a solid or cystic renal lesion not fulfilling the Bosniak I simple cyst criteria. Bosniak I cysts have thin walls (2 mm) and homogenous fluid signals (signal intensity similar to cerebrospinal fluid) without septa or calcifications (14). Complex renal lesions are characterized by the presence of nodules, heterogeneous signal intensity within the lesion, unclear margins, the presence of any thick septations, or low T2 signal intensity (compared to CSF within the spinal canal). Examples in Figure 1 illustrate the imaging characteristics used to identify complex renal lesions on T2-weighted MRI. In addition, the maximum axial diameter of the renal lesion was documented. The interpretation of imaging markers was made independently by a board-certified radiologist with 7 years of radiology experience. The interpreting radiologists were not aware of the clinical or imaging report information. Any disagreements were resolved by consensus after independent data collection. The body imagers reviewed the confirmatory imaging by consensus and were not provided with the interpretations made by the MRI lumbar spine interpreting radiologists.
Patients with simple cysts on MRI were examined using kidney ultrasound by an expert radiologist with a low-frequency (5 MHz) convex transducer of GE Voluson E10 (GE Healthcare), employing high-resolution B mode to determine the ultrasound characteristics of the cyst, including the nature of the cyst (simple or complex), the presence of septa, the wall characteristics, and the presence of calcification. For MRI complex cysts, patients underwent a CT scan with contrast, and the findings of the contrast-enhanced CT were compared with lumbar MRI. For each renal lesion in the study, radiologists with five years of experience reviewed cross-sectional imaging studies and results as confirmatory tests to make a final diagnosis. A simple cyst (Bosniak I) is defined as a cyst without septa and calcification, having a thin wall without solid parts, a low signal in the T1 sequence, and a high signal in the T2 sequence.
A 64-channel Toshiba Aquilion CT system (Toshiba America Medical Systems, Tustin, California) was used for abdominal CT scans. The study consisted of a non-contrast CT, corticomedullary phase (40 - 70 seconds), and excretory phase (7 - 10 minutes) conducted with a 2.5 mm section thickness after administering intravenous contrast.
The statistical analysis included assessing the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of T2-weighted imaging in identifying complex renal lesions on lumbar spine MRI. A two-tailed Fisher's exact test was also performed to examine the correlation between renal lesion size and the occurrence of complex renal lesions. The statistical analysis was performed using SPSS software (version 26), and a P-value below 0.05 was considered statistically significant.
4. Results
In 2,789 reviewed lumbar MRIs, 169 (6.05%) incidental renal cysts were reported (male to female ratio: 100: 69; average age: 54.6 years). Kidney cysts were slightly more common in males than in females, with a male to female ratio of approximately 1.44 to 1. The average age of patients with cysts was about 55 years. The cysts were on the right side in nearly half of the patients; about 42% had left-sided cysts, and the rest had bilateral cysts. Among the patients with cysts, about 30% had cysts larger than 30 mm. Patient demographics and the prevalence of renal lesions are provided in Table 1. According to the MRI reports, 12 patients (7.1%) had complex cysts, of which 2 cases (1.18%) were false positives (low signal in MRI but simple in CT scan), and 157 patients (92.89%) had simple cysts. The average size, represented by the mean axial diameter ± SD, of simple cysts was 21.92 ± 15.54 mm, while that of complex renal lesions was 40.50 ± 45.78 mm. Our analysis revealed a significant correlation between the size and type of renal lesion (simple or complex) (P < 0.01) (Tables 2 and 3). There was no significant difference between simple and complex cysts according to the age and sex of the patients (Table 2).
| Variables | Values |
|---|---|
| Age (y); N = 206 | 54.6 ± 13.7 |
| Sex | |
| Male | 118 (57.3) |
| Female | 88 (42.7) |
| Renal lesions | |
| Simple cyst | 194 (94.2) |
| Complex cyst | 12 (5.8) |
| The maximum diameter of cyst (mm) | |
| < 10 | 39 (19.8) |
| 10 - 19 | 75 (38.1) |
| 20 - 29 | 33 (16.8) |
| > 30 | 50 (25.4) |
| Location | |
| Right | 75 (49.7) |
| Left | 66 (43.7) |
| Bilateral | 10 (6.6) |
a Values are presented as mean ± SD or No. (%).
a Values are expressed as No. (%) or mean ± SD.
b Fisher’s exact test.
c Independent t-test.
| Cyst Type | Size | 95% CI for Mean | ||
|---|---|---|---|---|
| N | Mean ± SD | Lower Bound | Upper Bound | |
| Simple | 194 | 21.92 ± 15.54 | 19.71 | 24.12 |
| Complex | 12 | 40.50 ± 45.78 | - 7.54 | 88.54 |
| Total | 206 | 22.47 ± 17.23 | 20.07 | 24.81 |
The data presented in Table 4 pertains to the accuracy of lumbar spine MRI in identifying complicated renal lesions. From the axial T2-weighted image sequence alone, the readers of lumbar spine MRI categorized 169 renal lesions as simple cysts, while 12 were identified as complex renal lesions. A low T2 signal intensity on MRI (N = 9), septations of the lesion (N = 4), and nodularity of the lesion (N = 3) were the predominant findings on MRI that suggested a complex renal lesion in these cases. Using confirmatory testing as the benchmark, the lumbar spine MRI exhibited a reader sensitivity of 100% and specificity of 98% in detecting complex renal lesions. Additionally, the positive predictive value (PPV) was 83%, and the negative predictive value (NPV) was 100%.
| Characteristic | Values |
|---|---|
| Sensitivity | 100 |
| Specificity | 98 |
| Positive predictive value | 83 |
| Negative predictive value | 100 |
| True Positive | 10 |
| Bosniak 2 cyst | 2 |
| RCC | 6 |
| Angiomyolipoma | 1 |
| Adjacent lung cancer extent to kidney | 1 |
| False positive | 2 |
| Simple cyst | 2 |
| True negative | 194 |
| Simple cyst | 194 |
| False negative | 0 |
a Values are presented as No. (%).
5. Discussion
In recent decades, the use of diagnostic imaging has increased, and this rise in modalities such as CT scans and MRI has led to the detection of many incidental findings in patients. One of the relatively common findings in lumbar MRI is kidney cysts. In this study, we investigated the diagnostic value of MRI in identifying incidental cystic kidney lesions found in lumbar MRI compared to CT scans and ultrasound.
The results showed that incidental kidney cysts were present in 6.05% of all lumbar MRIs. Of these incidental cysts, 7.1% were complex. There were no significant differences in terms of age and sex between patients with simple and complex cysts.
In our study, the diagnostic value of MRI in differentiating complex cysts from simple cysts was investigated in comparison with ultrasound and CT scans. The sensitivity and negative predictive value of MRI in diagnosing complex cysts were calculated as 100%. Its specificity was 98.98%, and the positive predictive value was 83%. Therefore, it can be concluded that all complex cysts can be detected on MRI, and no complex cyst is reported as a simple cyst on MRI. However, MRI may report a simple cyst as a complex cyst. In other words, when a cyst is reported on MRI as complex, there is more than an 80% probability that the cyst is truly complex.
The presence of false positive cases has led to a slight decrease in specificity. Previous studies have mentioned that these false positive cases may be due to the presence of artifacts in MRI images, as respiratory movements and vascular pulses can lead to signals similar to septa and nodularity in the images (15). However, in our study, the false positive cases in MRI were not due to the presence of septa and nodularity, but rather the low signal nature of the cysts in the MRI led to their misdiagnosis as complex cysts.
The evidence supporting the use of MRI for diagnosing renal lesions as simple or complex is limited. This is especially true for lumbar MRIs because, in these cases, lesions may only be seen in axial T2 sequences, and there is no possibility of using T1 sequences to further evaluate the characteristics of the lesion and compare it with an internal fluid (such as CSF). However, in our study, it was shown that T2 images could have 100% sensitivity and nearly 99% specificity in distinguishing complex from simple lesions.
In a study conducted in 2019 by Nelson et al., 149 kidney lesions detected in lumbar spine MRI were evaluated. In their study, 72 lesions were diagnosed as simple cysts and 77 lesions as complex. They showed that the sensitivity of lumbar spine MRI was 94%, its specificity was 63%, and the positive and negative predictive values were 43% and 97%, respectively (15).
In our study, the diagnostic value of MRI was higher. Unlike Nelson's study, the mean diameter of simple and complex cysts was significantly different in our study. The size of the renal lesions seems to be a controversial factor in determining whether they are simple or complex, based on the type of lesions. According to Nelson et al.'s study, nodularity is the most common MRI finding in complex renal lesions. The most common finding in our study was a lower signal intensity than CSF. However, the conclusions of that study are largely consistent with this study. They showed that T2 images alone could probably detect neoplastic and potentially neoplastic complex renal lesions, suggesting that further investigation with modalities such as CT scans and ultrasound is unnecessary for cysts reported as simple on MRI. The updated Bosniak classification v.2019 includes an expanded class II for cystic renal masses.
The Bosniak II renal cysts are homogeneous renal masses that appear hyperintense on T2-weighted imaging (similar to cerebrospinal fluid) on non-contrast MR imaging. There is no need to further characterize lesions that meet this criterion, as they are commonly encountered on abdominal and spinal non-contrast MR imaging (15-17). Compared to the previous Bosniak classification, more renal masses can now be diagnosed as benign. This is clinically significant because it avoids costly workups for these masses that are unlikely to reveal malignancy (17, 18). Version 2019 of the Bosniak classification can significantly reduce overtreatment but at the cost of a significant sensitivity loss compared to version 2005 (19). Our results indicate that an additional modality is required to improve accuracy.
It should be noted that, despite the fact that simple and complex cysts seen on MRI can be differentiated with high accuracy, not reporting a lesion in the kidney on lumbar MRI cannot definitively rule out the existence of a lesion. In a study by Cho et al., the authors included 70 patients who had both lumbar MRI and abdominal CT scans. The results showed that the detection rate of renal cysts on lumbar MRI compared to CT scan was 46.5% for cysts larger than 5 mm and 68% for cysts larger than 10 mm (20).
Overall, it is important that radiologists pay attention to structures other than the vertebral column that are visible in the images when reviewing lumbar MRIs. In the study by Fu et al., which investigated the prevalence and etiology of extraspinal malignancies incidentally observed in MRI of the lumbar spine, the authors also stated that extraspinal structures should be accurately and systematically evaluated in lumbar spine MRI, especially if the spinal findings do not explain the patient's symptoms (10).
There are several limitations to our study. Due to the difficulty in precisely characterizing small lesions using specific renal imaging methods, we opted to disregard lesions smaller than 1 cm. Hence, our findings may not be relevant to smaller lesions. Moreover, we evaluated renal lesions solely through axial T2-weighted imaging. Implementing lumbar spine MRI protocols that incorporate additional unenhanced axial T1-weighted or coronal T2-weighted sequences could enhance diagnostic precision for identifying intricate renal lesions. The lack of T1 sequence images may be a limitation, as axial T2 at the disc level can miss many renal cysts. Therefore, the sensitivity and negative predictive value of negative lumbosacral MRI for renal cysts should be assessed. Additionally, there are only 12 patients with complex cysts, which is the category requiring further imaging evaluation. Most of the incidental findings identified during lumbar spine MRI scans could not be further verified clinically by follow-up examinations.
5.1. Conclusions
Our results show that simple cystic lesions and complex kidney lesions can be distinguished from each other with high accuracy in the T2 sequence of lumbar MRI. Based on these results, it may not be necessary to perform further examinations with ultrasound and CT scan in patients whose lumbar MRI shows a simple renal cyst. Our study could be reliably applied to abdominal and pelvic MRIs without significant performance degradation. This can lead to a significant decrease in low-diagnostic-yield follow-up examinations and lower healthcare costs.