1. Introduction
Renal stones are included in the third highest urological diseases after urinary tract infection and prostate disease. The stone's diameter would vary in the terms of treatment and outcome (1). Stones less than 10 mm in diameter tend to pass spontaneously, while stone diameters between 10 mm - 20 mm are favorable to undergo extracorporeal shockwave lithotripsy (ESWL) therapy (2). Percutaneous nephrolithotomy (PCNL) is the primary option for stones over 20 mm. Percutaneous nephrolithotomy offers the highest stone-free rate compared to ESWL or retrograde intrarenal surgery (RIRS) (3).
Percutaneous nephrolithotomy results are based on some factors and difficulties; one of them is stone location, obesity, and renal parenchyma thickness (3-5). Nonetheless, PCNL requires a skilled operator and highly advanced instruments that may not be available across developing countries, while open nephrolithotomy may result in a longer hospital stay and higher pain scores after surgery (6).
Minimally invasive surgery using laparoscopy is emerging in urology surgery. The wide availability of the instruments may increase the usage factor among operators (7). Laparoscopic nephrolithotomy may offer the same benefit as PCNL with less invasive techniques and advanced instruments used in surgery (8). However, laparoscopic nephrolithotomy has some limitations due to intraoperative bleeding management, especially in thick renal parenchyma (9). Hence, a highly skilled operator is needed to manage the risk of excessive bleeding in laparoscopic nephrolithotomy (5). Herein, we present a renal stone case with a thick renal parenchyma treated with laparoscopic nephrolithotomy with low intraoperative bleeding using only three trocar insertions.
2. Case Presentation
A 45-year-old male presented to the Emergency Department of Adam Malik State Hospital, Medan, Indonesia, with the chief complaint of acute colic pain in the right flank radiating to the groin for over a year, which had worsened in the last 6 hours. The patient had no relevant medical, family, or psychosocial history. A physical examination of the flank area did not reveal any abnormalities. Urinalysis and complete blood count were normal. The preoperative hemoglobin level was 17 g/dL. Serum urea and creatinine levels were 41 mg/dL and 1.32 mg/dL, respectively, indicating a slight decrease in renal function.
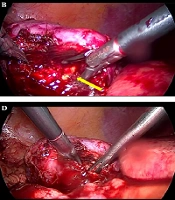
Abdominal ultrasonography showed a stone mass with an acoustic shadow in the right kidney (Figure 1A). This was followed by a kidney, ureter, and bladder (KUB) X-ray, which revealed a 3-centimeter right renal stone (Figure 1B). Subsequently, an abdominal non-contrast computed tomography (CT) scan was performed for better visualization of the renal stones and surrounding organs. The CT scan showed a 3-centimeter right pelvicalyceal stone with a thick renal parenchyma (Figure 1C). The patient had not undergone any previous surgical interventions. After obtaining informed consent, we decided to perform laparoscopic nephrolithotomy due to the patient's condition.
A, an abodminal ultrasonography showed a hyperechoic mass with accoustic shadow in right kidney; B, a KUB X-ray showed a radio opaque stone mass in right kidney (yellow arrow); C, an abdominal CT scan showed 3 centimeters renal stones in right kidney (yellow arrow) with thick renal parenchyma (red arrow).
2.1. Surgical Technique
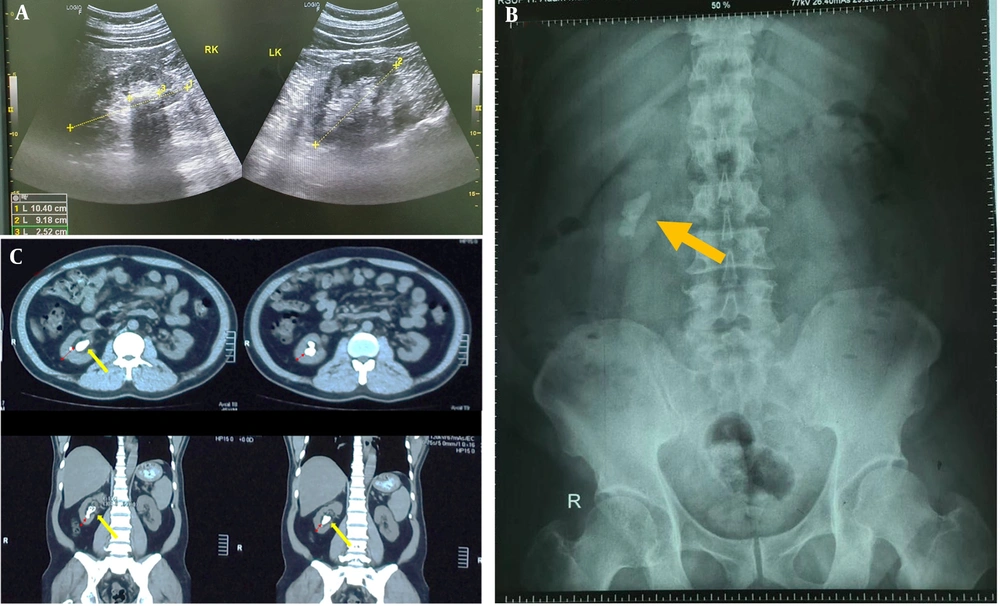
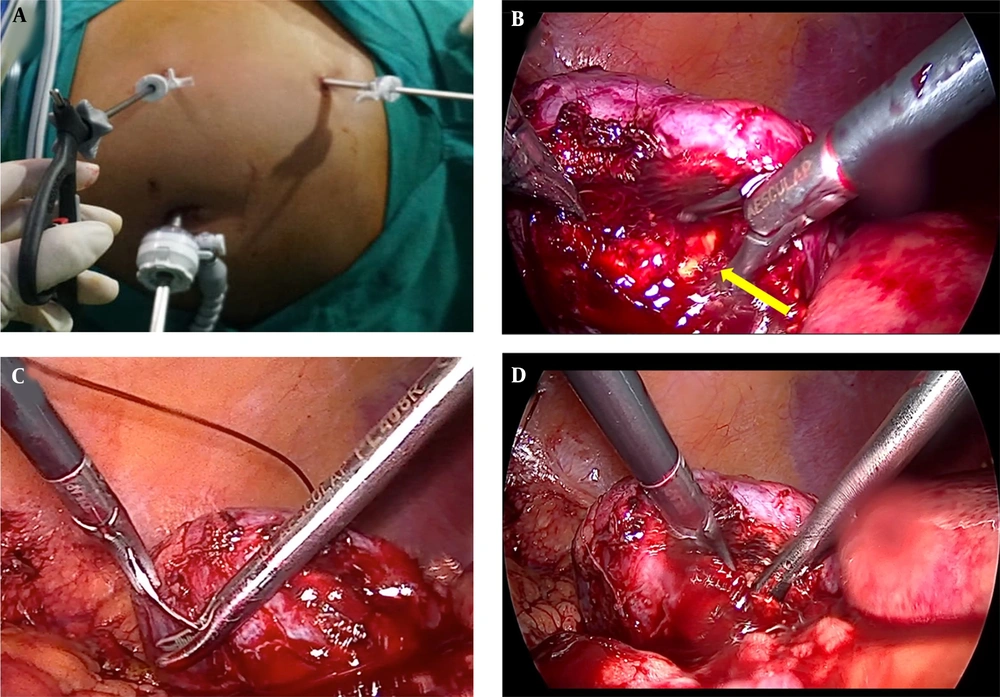
Under aseptic precautions, the patient was placed in the lumbotomy position under general anesthesia. Only three ports were used in this procedure. The first port, an 11-mm port, was inserted at the umbilicus using the direct Trocar insertion (DTI) technique. The second port, a 5-mm trocar, was placed subxiphoid, and the third 5-mm port was positioned in the right pararectus muscle. The abdomen was insufflated to maintain the position of all trocars (Figure 2A). A 30-degree laparoscopic camera was inserted through the 11-mm trocar at the umbilicus to guide the placement of the other trocars.
The kidney was separated from the surrounding tissue. A hypotensive technique was employed by anesthesia to minimize bleeding risk, followed by a parenchymal incision. Approximately a 2-centimeter incision was made using a hook at the Brodel's line (an avascular area) in the inferior pole of the kidney (Figure 2B). The stones were completely removed through the incision, which was then closed using 1 - 0 chromic catgut (Figure 2C). A suction drain was inserted through the 5-mm port in the abdomen. After desufflation, the 3-centimeter stones (Figure 3) were evacuated through the 11-mm trocar by adding an additional incision on the abdominal wall. A 6 Fr double J stent was introduced retrograde. The surgery took 120 minutes, and a total of 300 milliliters of blood loss was noted. No perioperative complications were found in this patient. Early mobilization was introduced 2 hours post-operatively. The Visual Analog Scale (VAS) score recorded was 5 and 3 on the first and second post-operative days, respectively.
No residual stones were visualized on the post-operative KUB X-ray (Figure 4). The post-operative complete blood count was normal, with hemoglobin recorded at 16.5 g/dL. The patient was discharged from the hospital 2 days after surgery.
The patient has agreed to the publication of their case, images, and supplementary laboratory reports in this case report through formal signed consent and the ethical committee of Adam Malik State Hospital, under registration number 874649.
3. Discussion
Renal stones are one of the most common diseases in urology, with an almost 50% recurrence rate (1) Therefore, treatment options vary widely, ranging from non-invasive and minimally invasive methods to open nephrolithotomy (2, 3). Each modality comes with different conditions and outcomes (2, 3, 6).
Percutaneous nephrolithotomy is one of the most common treatment modalities for large renal stones, offering high stone-free rates (3). However, PCNL and C-arm instruments may not be readily available in developing countries and require a highly skilled operator to manage the risk of internal bleeding (2). Open nephrolithotomy, while effective, may result in longer hospital stays and higher postoperative pain rates (10).
A meta-analysis reported that laparoscopic surgery for evacuating renal stones might offer similar benefits to PCNL (6). Thus, it is often suggested as an alternative to PCNL. However, laparoscopic nephrolithotomy is not routinely performed due to difficulties in managing bleeding from a laparoscopic view (2, 9). A previous case report described laparoscopic nephrolithotomy on patients with staghorn stones (7), but the technique used did not involve an incision in the Brodel’s line area and did not utilize a hypotension technique.
A patient presented with a 3-centimeter renal stone and a thick kidney parenchyma. As PCNL and C-arm instruments were not widely available across the country, we proposed performing laparoscopic nephrolithotomy to achieve better postoperative outcomes and shorter hospitalization compared to open nephrolithotomy.
A small incision on the kidney parenchyma using a hook was made to achieve better kidney function after surgery. A hypotension technique during the incision was used by the anesthesia team to reduce intraoperative bleeding. A total of 300 cc of blood loss was recorded during this operation. A meta-analysis of PCNL and open nephrolithotomy showed that average intra-operative blood loss might reach 500 milliliters per surgery. Although laparoscopic nephrolithotomy has a risk of excessive bleeding during the operation, our study showed that precise coordination between the operator and anesthesia team could result in better control of intraoperative bleeding.
Using only three trocars at the laparoscopic site, our study demonstrated that fewer trocars lead to better postoperative pain outcomes. A previous report indicated that most laparoscopic nephrolithotomies use five trocars to provide operator flexibility (11). However, our study showed that even with fewer trocars, a better postoperative and intraoperative outcome is still achievable.
Moreover, our laparoscopic nephrolithotomy also offers a shorter operation time, which may help prevent the patient from acute kidney injury (AKI) (12). A meta-analysis of PCNL reported an average operation time of 180 minutes, while our study only took 120 minutes(4). Previous reports also indicated that laparoscopic nephrolithotomy typically lasts around 100 - 120 minutes (13). These findings suggest that laparoscopic nephrolithotomy may offer better renal function and protection.
Finally, we believe that minimally invasive surgery using laparoscopy is the future for nephrolithotomy. It is more widely available compared to PCNL and offers better outcomes. Future studies should investigate all aspects of the advantages of using laparoscopic nephrolithotomy compared to other modalities.
3.1. Conclusions
Laparoscopic nephrolithotomy is safe and effective for removing renal stones with thick renal parenchyma, with no intraoperative or postoperative complications. Laparoscopic nephrolithotomy may be an alternative to PCNL and open nephrolithotomy when these options are not available.