1. Introduction
Vascular access is crucial for administering fluids, medications, and nutrition in neonatal care, especially for those requiring long-term hospitalization (1, 2). When peripheral veins are inaccessible through percutaneous efforts, central vein cannulation is necessary for administering large-volume fluids, high-osmolarity solutions, or parenteral nutrition (3).
The venous cutdown technique is valuable in neonatal emergencies when less invasive percutaneous attempts for venous access, such as the Seldinger technique, ultrasound-guided technique, and intraosseous vascular access, have failed (4, 5). This technique can be lifesaving in neonates and infants with fragile, non-palpable veins or collapsed vessels due to hypovolemic shock (6, 7).
The femoral vein, running from the ankle to the inguinal region, is one of the most preferred cutdown access sites in neonates. Its superficial and large structure makes it easily accessible for central venous access and emergency vascular line insertion (8-10). Additionally, inserting a venous line in this location keeps vital organs available for resuscitation maneuvers and respiratory support (11). However, medical staff should be aware of several life-threatening complications, including failed cannulation, accidental arterial perforation, hemorrhage, sepsis, vascular thrombosis, embolism, and hemo- and pneumothorax (4, 12). Practical skills, special qualifications, and serial follow-up examinations are essential to ensure proper insertion and prevent severe complications (13).
In this study, we report a neonatal case of catheter tip displacement following femoral vein cutdown, resulting in a scrotal hematoma. To our knowledge, this is the first case report of catheter dislocation after performing the femoral vein cutdown technique.
2. Case Presentation
A neonate was born at Yas Complex Hospital in Tehran, Iran, on 29 August 2022. His gestational age was 39 weeks, birth weight was 3740 grams, and his Apgar scores at the first and fifth minutes were 9 and 10, respectively. The delivery was a cesarean section due to maternal indications (lumbar disc herniation). The newborn gradually showed symptoms of mild to moderate respiratory distress, including grunting, nasal flaring, tachypnea, and intercostal and substernal retractions. He was immediately transferred to the neonatal intensive care unit (NICU), and oxygenation was initiated through nasal CPAP.
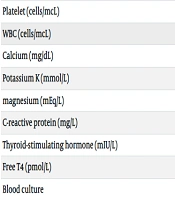
In the first minutes of NICU admission, the patient's condition worsened, with his respiratory distress score increasing to 7, necessitating intubation. Peripheral vascular access was established, and 2 ml of venous blood was collected and sent to the laboratory (results shown in Table 1). Endotracheal surfactant was administered based on the neonate’s general condition, chest X-ray results (congenital pneumonia), and blood gas findings. Intravenous fluid (dextrose water 10%) and antibiotic therapy (amikacin and vancomycin) were initiated due to congenital pneumonia. After approximately 5 hours, following symptom relief, the neonate was extubated, and respiratory support was continued through non-invasive positive pressure ventilation (NIPPV).
| Laboratory Test | Results |
|---|---|
| Hemoglobin (g/dL) | 12.7 |
| Platelet (cells/mcL) | 185000 |
| WBC (cells/mcL) | 10000 |
| Calcium (mg/dL) | 9.2 |
| Potassium K (mmol/L) | 9.2 |
| magnesium (mEq/L) | 2.2 |
| C-reactive protein (mg/L) | 56 |
| Thyroid-stimulating hormone (mIU/L) | 6 |
| Free T4 (pmol/L) | 0.8 |
| Blood culture | Negative |
| Direct Bilirubin (mg/dl) | 6.2 |
| Total Bilirubin (mg/dl) | 0.6 |
| Blood group | A positive |
| G6pd (u/g) | > 6.4 |
| pH | 28 |
| PCO2 (mmHg) | 58 |
| PO2 (mmHg) | 60 |
| HCO3 (meq/L) | 18.9 |
| Base excess (mEq/L) | -8 |
During the first two days of NICU admission, respiratory support was gradually reduced according to the patient's condition. On day 3, vascular access failed, and several attempts at percutaneous venipuncture were unsuccessful. Umbilical catheterization was not attempted due to umbilical inflammation and suspected omphalitis. To access central blood vessels, a pediatric surgeon was consulted. The surgeon recommended a surgical venous cutdown through femoral catheterization.
The neonate was prepared for the surgery, and after skin preparation (prep-drape) and under local anesthesia (using lidocaine 2%), a longitudinal incision was made on the right superolateral inguinal area. A 22-gauge catheter was inserted into the right femoral vein, with the catheter tip placed into the external iliac vein after guidewire removal (within the next half-hour). Appropriate insertion site examination showed blood flow in the catheter, which was then fixed using surgical silk suture 3/0. Intravenous fluid and antibiotics were continued through the cutdown catheter.
The neonate was under full observation for vital signs and health conditions. However, over the next 4 hours, right scrotal edema, discoloration, localized erythema, and clear fluid leakage from the right scrotum were observed during a diaper change (Figure 1).
These signs rapidly progressed to increased scrotal edema, inflammation, and ecchymosis within a few minutes of monitoring (Figure 2), although the neonate's vital signs remained stable. A consultation with the NICU neonatologist was performed, and the intravenous infusion was urgently clamped after the patient's visit by the specialist. A pediatric surgeon was then consulted, who recommended the removal of the catheter. The highly probable diagnosis was the displacement of the catheter tip and infusion into a false route, resulting in a scrotal hematoma and fluid leakage.
Five minutes after catheter removal, Color Doppler sonography was performed, confirming the diagnosis. The sonography examination showed scrotal soft tissue thickening and an avascular hypoechoic 11 × 10 × 4 mm region indicating a hematoma at the inferior pole of the right testis. Bilateral testicular parenchyma appeared normal, and there was no evidence of hydrocele. The neonate was monitored hourly for vital signs and local manifestations. He was managed with conservative treatment, which included applying zinc oxide cream to the affected area daily and conducting daily ultrasound examinations. The signs alleviated six days after catheter removal, and the neonate was discharged on the 10th day of NICU admission in good condition and without significant erosion at the catheterization site (Figure 3).
Follow-up visits, including physical examinations and ultrasound studies, were performed every two weeks for the first three months and then monthly for the next three months. No obvious complications or residual hematoma were revealed during the serial follow-ups.
3. Discussion
Although displacement of cannulation is not a rare catheter-related complication, this study uniquely presents an unusual risk consequent to femoral venous cutdown. In the case presented, we demonstrated the displacement of the catheter tip and false route fluid infusion resulting in vessel injury, scrotal hematoma, inflammation, and leakage of infused fluid through the skin. Immediate removal of the catheter, close monitoring, conservative therapy, and serial follow-ups effectively prevented the progression of local signs.
Despite caution and anatomical knowledge, catheterization failure, hemorrhage, infection, venous thromboembolism, and soft or neural tissue injuries are not uncommon risks associated with the venous cutdown procedure (6). Several investigations have reported injuries and complications during or after the venous cutdown technique. Chappell et al. noted the incidence of complications associated with venous cutdown procedures to be between 2 - 15%, with hemorrhage due to femoral vessel injury being a common complication (14). Kansay et al. reported a case of iatrogenic median nerve damage consequent to basilic venous cutdown surgery (15). Rhee et al. reported local cellulitis in a case requiring the ankle saphenous vein cutdown (16). Annetta et al. highlighted risks such as catheter displacement, venous thromboembolism, and dislodgment (11). Kirov et al. reported wound complications, lymphatic fistula, and lymphocele following femoral cannulation (17). No study has previously reported scrotal hematoma due to the displacement of the catheter tip after femoral vein cutdown, suggesting it is a very rare complication in this context.
Evidence suggests no need for radiologic confirmation in cases with central line access through the lower extremities. However, medical staff should be vigilant for any complications related to the displacement of central venous catheterization. The presence of an expert multidisciplinary team familiar with the procedure, the use of ultrasound-guided techniques, and the selection of an appropriate catheter with a soft tip and proper insertion length can help prevent unexpected complications (5, 18). Minimizing the neonate’s extremity movements and frequently checking the insertion site may reduce potential risks (13). Catheter removal is recommended in cases where local signs indicate catheter misplacement (6). Placing the patient in a left lateral decubitus or head-down position is suggested for suspected air embolism cases (10). It is advised that femoral catheters should not remain in place longer than 48 hours due to the risks of displacement and thromboembolism, and using the mid-thigh as the insertion site may decrease the risks of infection and thrombosis (11).
The case presented in this study revealed the potential for severe complications, such as scrotal damage, following femoral cutdown catheterization. This unexpected complication was effectively managed by the immediate removal of the catheter, close monitoring, conservative therapy, and serial follow-ups. To prevent complications associated with femoral cutdown cannulation, it is recommended to implement an expert multidisciplinary team, use ultrasound-guided techniques, choose an appropriate catheter with the proper insertion length, and be aware of potential testicular injuries. The use of fluoroscopy can also help alleviate consequent complications (10). Additionally, femoral cutdown catheterization should be replaced by less invasive vascular access methods like umbilical catheterization or peripherally inserted central catheter (PICC). Developing a protocol for alternative vascular access in NICUs would be beneficial. Finally, all NICU staff should be trained to improve catheterization skills and to prevent or manage catheterization complications.
3.1. Conclusions
This case report demonstrated scrotal damage following femoral cutdown catheterization. This unexpected complication was effectively managed by the immediate removal of the catheter, close monitoring, conservative therapy, and serial follow-ups. NICU staff should be aware of the potential for testicular injuries in these cases.