1. Background
Varicocele, defined as the abnormal venous dilation of the pampiniform venous plexus, is found in about 15% of the general male population (1). One of the main consequences of varicocele is infertility, affecting pregnancy outcomes in terms of sperm function and quality (2). The prevalence of varicocele in males with primary and secondary infertility is up to 35% and 80%, respectively (1). Although the exact pathophysiology of varicocele and its effects on testicular functions have not been determined, several mechanisms have been suggested: Hyperthermia, an increase in reactive oxygen species, and elevated apoptosis (3). Varicocele is asymptomatic in most cases, but in the remaining 10%, it can present with pain in the inguinal and scrotal regions and bulging dilated scrotal veins (4). The main diagnostic tools for varicocele are medical history and physical examination, while other modalities like ultrasonography and venography can be used for further evaluation (4). Various techniques for treating varicoceles exist, including laparoscopic and inguinal surgeries, embolization, and open retroperitoneal high ligation (2). Treatment is recommended only in cases with clinical varicocele and documented infertility, not for subclinical varicocele (2). Varicocele treatment can increase pregnancy rates by 29% and significantly improve sperm concentrations (5).
Living kidney donation is increasing globally due to the rising number of individuals with underlying conditions like end-stage renal disease who need kidney transplantation (6). Although there are some perioperative complications for living kidney donors and long-term risks, it is still considered a safe procedure (7, 8). The perioperative complication rate of kidney donation is about 17%, with serious adverse events being infrequent (7). Renal vascular variations are common in those who undergo nephrectomy, with accessory renal arteries or veins being the most prevalent (9). Furthermore, left-sided nephrectomy in living kidney donors can increase the diameter of the left pampiniform veins, predisposing these donors to varicocele (10). A prior study conducted in Iran evaluated the diameters of the pampiniform venous plexus and testis after nephrectomy (10). Another study compared the accuracy of different diagnostic techniques for varicocele, such as physical examination and ultrasonography, in the general population (11). However, none of these studies evaluated histological findings in those who underwent nephrectomy. More research is needed to report the prevalence of varicocele in different populations in recent years and to evaluate the effects of nephrectomy on varicocele using various diagnostic tools.
Despite the well-established link between varicocele and infertility, significant gaps remain in our understanding, particularly regarding the histological changes in the testis after nephrectomy and the variability in diagnostic accuracy among different techniques. Furthermore, the association between left-sided nephrectomy and the subsequent development of varicocele requires further investigation.
2. Objectives
Therefore, this study aimed to report the frequency of varicocele in a sample of kidney donors who underwent left-sided nephrectomy, quantify the agreement between physical examination, Doppler ultrasound, and histological analysis in diagnosing varicocele, explore discrepancies between diagnostic methods, investigate their clinical implications and potential contributing factors, and provide recommendations for the optimal use of diagnostic techniques in evaluating varicocele in kidney donors, considering the strengths and limitations of each method.
3. Methods
3.1. Study Design and Participants
This analytical cross-sectional study was conducted at Imam Reza Hospital, Tabriz University of Medical Sciences, Tabriz, Iran, from January 2021 to May 2023. We employed a purposive sampling strategy to select adult males who had undergone left-sided nephrectomy for living kidney donation at Imam Reza Hospital. This approach ensured that participants met the specific inclusion criteria relevant to the study objectives. The exclusion criteria included individuals under 18 years of age, those who were candidates for right-sided nephrectomy, and those with a history of left inguinal surgery, left orchiectomy, or left varicocele surgeries.
The sample size was calculated using the formula for cross-sectional studies, considering a confidence level of 95% and a margin of error of 5%. Based on previous studies, we estimated the prevalence of varicocele in kidney donors to be approximately 30%. This calculation determined that a minimum of 50 participants would be required to achieve adequate statistical power.
3.2. Ethical Approval
The study was approved by the Ethics Committee of Tabriz University of Medical Sciences (ethics code: IR.TBZMED.REC.1401.138). Before enrollment, the study protocol was thoroughly explained to all eligible participants, and written informed consent was obtained from each participant. Participants were assured that their data would be kept confidential and used solely for research purposes, in accordance with the Declaration of Helsinki and national guidelines.
3.3. Data Collection and Assessments
Candidates for living kidney donation were enrolled in the study. Demographic information and clinical data were obtained from their medical records. Clinical examinations were conducted to assess the presence and grading of varicocele. Additionally, ultrasound examinations were performed to assess the diameter of the pampiniform venous plexus. The maximum diameter was measured in millimeters (mm) before and after the Valsalva maneuver, with specific attention to central vein flow velocity. During left-sided nephrectomy, a portion of the left spermatic vein was sent to the pathology laboratory for histopathological evaluation. Histopathological findings regarding the condition of the venous valves were investigated. Pathology reports were then compared and analyzed with clinical examination and preoperative ultrasound findings.
Clinical examinations were performed after participants stood for five minutes in a warm room. Testicular contents, including volume, position, and consistency, were assessed. Each spermatic cord was palpated while standing at rest and during the Valsalva maneuver. Findings were classified according to the Dubin and Amelar system (12). To minimize bias, the examiners conducting the clinical examinations and ultrasound assessments were blinded to the participants' clinical history and previous examination results.
3.4. Definitions
The grading of varicocele was as follows:
(1) Grade I or mild varicocele: The veins are palpable under pressure, meaning they become palpable when the patient strains or when the abdominal area is compressed. The diameter of the vein in the spermatic cord or the pampiniform venous plexus is between 3 and 4 millimeters (mm), increasing by 1 mm during the Valsalva maneuver.
(2) Grade II or moderate varicocele: The veins are palpable in the standing position. The diameter of the vein in the spermatic cord or the pampiniform venous plexus ranges between 4 and 5 mm, increasing by 0.2 to 0.5 mm during the Valsalva maneuver.
(3) Grade III or severe varicocele: The veins are visible in the standing position. The diameter of the vein in the spermatic cord or the pampiniform venous plexus is more than 5 mm, increasing by more than 0.5 mm during the Valsalva maneuver.
(4) Subclinical varicocele: In this condition, the veins are not palpable on physical examination but are diagnosed through ultrasound. The diameter of the vein in the spermatic cord or the pampiniform venous plexus is between 2 and 3 mm.
In this method, patients were asked to stand for five minutes before the examination was performed. The maximum diameter of the scrotal veins and the velocity of the central vein flow were measured before and after the Valsalva maneuver (12).
3.5. Statistical Analysis
The data obtained from the study were analyzed using descriptive statistics, reported as mean and standard deviation (SD) for continuous variables and as frequencies and percentages for categorical variables. The chi-square test was used to compare categorical variables. Statistical analysis was conducted using the Statistical Package for the Social Sciences (SPSS) version 20.0 (IBM Corp., New York, USA). A P-value of less than 0.05 was considered statistically significant.
4. Results
4.1. Baseline Characteristics
In this study, 59 kidney donor candidates were initially enrolled, but nine individuals were excluded due to their history of left inguinal surgeries, varicocele surgeries, or orchiectomy. Subsequently, the remaining 50 patients underwent clinical examinations to assess the presence and grading of varicocele, as well as ultrasound evaluations to measure the diameter of the pampiniform venous plexus. All participants were male, with a mean age of 36.6 (SD: 5.7) years and a mean Body Mass Index (BMI) of 23.1 (SD: 3.2) kg/m2.
4.2. Physical Examination, Ultrasound
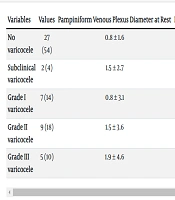
On physical examination, 29 (58%) participants had no varicocele, 6 (12%) had grade I, 9 (18%) had grade II, and 6 (12%) had grade III varicoceles. In the Doppler ultrasound investigation, 2 (4%) had subclinical varicocele, 7 (14%) had grade I, 9 (18%) had grade II, and 5 (10%) had grade III varicoceles. The diameter of the pampiniform venous plexus increased both in the resting state and during the Valsalva maneuver (Table 1).
| Variables | Values | Pampiniform Venous Plexus Diameter at Rest | Pampiniform Venous Plexus Diameter During Valsalva Maneuver |
|---|---|---|---|
| No varicocele | 27 (54) | 0.8 ± 1.6 | 1.1 ± 1.8 |
| Subclinical varicocele | 2 (4) | 1.5 ± 2.7 | 1.8 ± 2.7 |
| Grade I varicocele | 7 (14) | 0.8 ± 3.1 | 0.8 ± 3.6 |
| Grade II varicocele | 9 (18) | 1.5 ± 3.6 | 2.8 ± 4.6 |
| Grade III varicocele | 5 (10) | 1.9 ± 4.6 | 1.8 ± 5.4 |
a Values are expressed as No. (%) or mean ± SD.
4.3. Histopathological Findings
In the histopathological examination of the left internal spermatic vein, 27 (54%) had intact valves, 16 (32%) had lax and incompetent valves, and 7 (14%) had no valves.
4.4. Multivariate Analysis
After controlling for age and BMI through multivariate analysis, the association between physical examination and histological findings remained significant (P = 0.04). However, the association between ultrasound and histological findings was no longer significant (P = 0.07).
4.5. Association of Physical Examination and Ultrasound for Varicocele Diagnosis and Grading by Histological Findings
In the assessment of histopathological findings, among the 29 patients (58%) diagnosed without varicocele through clinical examination, 26 (52%) had intact valves, and 3 (6%) had lax and incompetent valves. Among the 6 patients (12%) diagnosed with grade I varicocele through clinical examination, 1 (2%) had intact valves, and 5 (10%) had lax and incompetent valves. Of the 9 patients (18%) diagnosed with grade II varicocele through physical examination, 7 (14%) had lax and incompetent valves, and 2 (4%) had no valves. Among the 6 participants (12%) with grade III varicocele diagnosed by physical examination, 1 (2%) had lax and incompetent valves, and 5 (10%) had no valves. There was a significant difference between the physical examination diagnosis of varicocele and the histological findings (P = 0.04) (Table 2).
| Variables | Varicocele Diagnosis by Physical Examination | Intact Valves | Lax or Incompetent Valves | No Valves | P-Value |
|---|---|---|---|---|---|
| No varicocele | 29 (58) | 26 (52) | 3 (6) | 0 (0) | 0.04 |
| Grade I varicocele | 6 (12) | 1 (2) | 5 (10) | 0 (0) | |
| Grade II varicocele | 9 (18) | 0 (0) | 7 (14) | 2 (4) | |
| Grade III varicocele | 6 (12) | 0 (0) | 1 (2) | 5 (10) |
a Values are expressed as No. (%).
When comparing the results of Doppler ultrasound and the histological findings, all those without varicocele had intact valves. Among the 2 participants (4%) with subclinical varicocele diagnosed by ultrasound, 1 (2%) had intact valves, and 1 (2%) had lax and incompetent valves. For those with grade I and II varicocele, lax and incompetent valves were the most common finding. All 5 participants (10%) with grade III varicocele diagnosed by ultrasound had no valves. There was no significant difference between Doppler ultrasound and histological findings (P = 0.07) (Table 3).
| Variables | Varicocele diagnosis by Doppler Ultrasound | Intact Valves | Lax or Incompetent Valves | No Valves | P-Value |
|---|---|---|---|---|---|
| No varicocele | 27 (54) | 27 (54) | 0 (0) | 0 (0) | 0.07 |
| Subclinical varicocele | 2 (4) | 1 (2) | 1 (2) | 0 (0) | |
| Grade I varicocele | 7 (14) | 3 (6) | 4 (8) | 0 (0) | |
| Grade II varicocele | 9 (18) | 0 (0) | 6 (12) | 3 (6) | |
| Grade III varicocele | 5 (10) | 0 (0) | 0 (0) | 5 (10) |
a Values are expressed as No. (%).
5. Discussion
Our findings indicated that among candidates for nephrectomy for kidney donation, most cases diagnosed through physical and ultrasound examinations had grade II varicocele. Comparing the histological findings with ultrasound and physical examination revealed significant differences between physical examination and histopathology for diagnosing varicocele, while the ultrasound results were consistent with the histological findings.
5.1. Prevalence of Varicocele
A population-based study involving more than 7,000 healthy males in six European countries showed a prevalence rate of 15.7% for grade I - III varicoceles from 1996 to 2010 (13). Our study found a prevalence of 42% for grade I - III varicoceles in adults who underwent nephrectomy. Notably, our study had a much smaller sample size of 50 participants compared to 7,035 in the European study. Larger sample sizes generally provide more accurate prevalence estimates (13). Additionally, the studies were conducted on different populations (healthy individuals vs. kidney donors) (13). Kidney donors may have a higher prevalence of varicocele. The frequency of subclinical varicocele in kidney donors has not been recently reported. In our study, 4% of participants had subclinical varicocele detected by Doppler ultrasound. Although there is some debate about the role of subclinical varicocele in male fertility, it remains an important factor in subfertility and should be monitored through Doppler ultrasound (14).
5.2. Histological Finding
Regarding histopathological findings, observations included an increase in connective tissue within both the adventitia and tunica media, as well as degradation of the outer longitudinal smooth muscle layer of the spermatic veins in patients with varicocele (15). Additionally, electron microscopy findings showed elongation of endothelial cells with signs of cellular damage, absence of the internal elastic lamina, and the presence of ghost bodies and degenerative vacuoles in the subendothelial layer (16). To our knowledge, previous studies have not reported the histopathological findings of varicocele among those who underwent nephrectomy for kidney donation. In our study, 32% of participants had incompetent valves, and 14% had no valves. Changes in the veins, such as dystrophy/hyperplasia of Leydig cells, endothelial atrophy, and lumen narrowing, predispose these individuals to infertility (17).
5.3. Comparison of Diagnostic Modalities
Before nephrectomy, the diameter of the pampiniform venous plexus ranged from 0.8 to 1.9 mm at rest and from 0.8 to 2.8 mm during the Valsalva maneuver. Consistent with our findings, the preoperative diameter of the left pampiniform veins in 54 kidney donation candidates was 1.37 mm (SD: 0.40) (10). In another study conducted in Iran between 2005 and 2006, out of 100 healthy kidney donors, the frequency of varicocele based on physical examination was 11%, with one, three, and seven cases having grade I, II, and III varicoceles, respectively (18). However, the frequency of varicocele based on physical examination in our study was much higher (42%), with most cases being grade II, whereas the previous study showed that most had grade III varicocele (18). Several factors could explain these differences. First, the mean age of participants in our study was higher (36.6 vs. 29.3 years). Since varicocele prevalence increases with advancing age (19), this could justify the higher frequency in our study. Second, other factors, such as height, BMI, and family history, are associated with the development of varicocele (20). Data on BMI and family history of varicocele were not reported in the aforementioned study (18). Third, the physician's experience in conducting physical examinations can affect varicocele diagnosis. For example, there is a higher specificity of physical examination for the diagnosis of varicocele among experienced urologists compared to urology residents (11). The study by Mokhtari et al. mentioned that urologists diagnosed varicoceles but did not specify their level of experience, which could also be a potential source of discrepancies (18).
5.4. Comparison of Histopathological Findings with Physical Examination
When we compared the histopathological findings with physical examination and Doppler ultrasound, we found that the ultrasound findings were compatible with histopathology. In contrast, diagnoses based on physical examination showed a significant difference with histopathology (P = 0.04). In this regard, the study by Cocuzza et al. used Doppler ultrasound as the gold standard for varicocele diagnosis. It revealed that the sensitivity, specificity, positive predictive value, and negative predictive value of physical examination for varicocele diagnosis were 55.6%, 74.6%, 75.5%, and 54.4%, respectively (11). There is ongoing debate regarding the gold-standard method for varicocele diagnosis and its clinical applications. Although venography is considered the gold standard for varicocele diagnosis, its use is limited in clinical practice (11). Some suggest that physical examination is the best tool for cases of clinically significant varicoceles (21). Lehner et al. conducted a study on 50 males with clinical and 52 with subclinical varicoceles to assess whether Doppler ultrasound could predict the varicocele grading system (22). They concluded that ultrasound is not significantly correlated with clinical grading and that diameter during the Valsalva maneuver was only clinically significant in distinguishing between grade I and II varicoceles (22). Overall, there is a need to develop clinical guidelines for diagnosing varicocele and to clarify how other modalities, especially Doppler ultrasound, can assist physicians in diagnosis (23).
The implications of our findings are significant for clinical practice. Given that Doppler ultrasound showed better alignment with histopathological results, we recommend its use as a first-line diagnostic tool for varicocele in kidney donors. Additionally, the identification of subclinical varicocele in 4% of our participants underscores the importance of routine Doppler ultrasound screening, as subclinical varicocele may contribute to male subfertility (14). Future research should focus on larger-scale studies to validate our findings and explore the impact of varicocele on fertility outcomes specifically in kidney donors. Investigating the relationship between varicocele and other demographic factors, such as BMI and family history, could provide further insights into its etiology. Moreover, developing standardized protocols for varicocele diagnosis that integrate both physical examination and Doppler ultrasound could enhance diagnostic accuracy and improve patient outcomes. A strength of our study was the inclusion of kidney donors who underwent nephrectomy, allowing us to compare the histological findings with physical examination and Doppler ultrasound, the commonly available tools for varicocele diagnosis. Additionally, we reported the frequency of varicocele in kidney donors.
5.5. Limitations
The findings of this study should be interpreted with caution due to several methodological limitations. The cross-sectional design of the study precludes the inference of causality between the diagnostic methods and histological findings. As this was a single-center study conducted at a tertiary referral hospital in Iran, the generalizability of the results to other populations, particularly those not undergoing kidney donation, is limited. The small sample size and the absence of semen analysis data may have affected the accuracy and statistical power of the results. The use of convenience sampling, while practical, may have introduced selection bias, as participants were selected based on their availability and accessibility rather than through a random sampling method. Despite our efforts to account for numerous identified confounding factors, the potential influence of unmeasured variables, such as comorbidities and genetic factors, cannot be ruled out. The diagnosis of varicocele was based on physical examination and Doppler ultrasound, which may not be as sensitive as more advanced techniques like venography. The lack of a standardized protocol for varicocele diagnosis across different examiners could have contributed to variability in the results.
5.6. Main Points
(1) There was a significant difference in varicocele diagnosis between physical examination and histological findings among kidney donors who underwent left-sided nephrectomy, highlighting the need for more accurate diagnostic methods.
(2) The study found that both physical examination and ultrasound revealed a high frequency of varicocele cases, primarily graded as grade II, emphasizing the importance of thorough evaluation in kidney donors post-nephrectomy.
(3) The notable discrepancy in varicocele diagnosis between different methods underscores the necessity for more extensive observational studies to assess this association and explore alternative methods for varicocele diagnosis in kidney donors.
5.7. Conclusions
In summary, in kidney donor candidates, there was a significant disagreement between physical examination and histological findings for varicocele diagnosis, suggesting that reliance solely on physical examination may lead to misdiagnosis in this population. In contrast, the findings were similar between Doppler ultrasound and histopathology, indicating its potential as a more reliable diagnostic tool. Considering the limitations of the current study, further large-scale observational studies evaluating other methods of varicocele diagnosis are recommended to determine the etiology of varicocele and improve pregnancy outcomes.