1. Introduction
Duplex kidney is a congenital fusion anomaly of the urinary tract characterized by the presence of two pelvicalyceal systems. Duplication can be incomplete, with the confluence of the two ureters occurring above the ureteric orifice, ranging from a bifid pelvis to Y-shaped duplication, or it can be complete (1). In cases of complete duplication, anomalies such as ureterocele and ectopic ureter predominantly affect the upper moiety, while anomalies such as vesicoureteric reflux and pelviureteric junction obstruction typically involve the lower moiety (2).
Pyonephrosis is a suppurative infection of the kidney associated with renal parenchymal damage. This condition often arises from an anatomical or functional obstruction of the urinary tract. Pyonephrosis can result in permanent renal function impairment, septic shock, and even death if left untreated. Rupture of pyonephrosis is an uncommon occurrence and, in most cases, the rupture is confined to the retroperitoneum. Spontaneous intraperitoneal rupture of pyonephrosis is exceedingly rare. To date, only eight cases of generalized peritonitis resulting from pyonephrosis rupture associated with urolithiasis have been reported.
We present a case of spontaneous intraperitoneal rupture of pyonephrosis secondary to urolithiasis in a 56-year-old female who presented with acute abdomen symptoms. This is the first reported case of intraperitoneal fistulization of pyonephrosis from a duplex kidney in the literature. Additionally, we share our successful treatment approach to managing this rare condition.
2. Case Presentation
A 56-year-old female presented to the emergency department with right flank pain associated with fever for 10 days and diffuse abdominal pain for 2 days. On examination, the patient was febrile (T=101°F), with a distended abdomen and signs of peritonitis. Her blood pressure and pulse rate were 116/68 mmHg and 110/min, respectively. Baseline investigations revealed a hemoglobin level of 9.1 g%, a total leukocyte count (TLC) of 20 × 10³/µL, and a serum procalcitonin level of 23.12 ng/mL. Serum amylase, lipase, creatinine, blood urea nitrogen (BUN), and liver function tests were within normal limits.
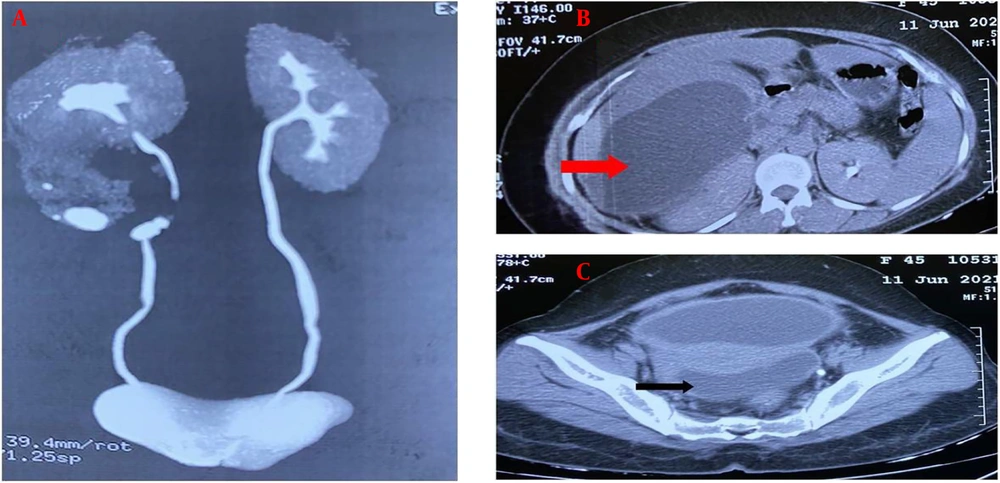
An abdominal ultrasound screening showed right lower calyceal dilatation and intraperitoneal free fluid collection. Contrast-enhanced computed tomography (CT) of the whole abdomen with urography phase revealed a right incomplete duplex kidney with a non-excreting, grossly hydroureteronephrotic lower moiety, and a 15 mm ureteric calculus (Figure 1A). Additionally, two other calculi were identified: One measuring approximately 15 mm in the lower calyx of the lower moiety and another non-obstructive calculus measuring 8 mm in the ureter of the upper moiety. The findings were associated with a right perinephric collection and large high-density fluid collections in the subhepatic, interloop, and pelvic regions, suggestive of a ruptured right lower moiety pyonephrosis (Figure 1B and C).
Empirical broad-spectrum antibiotics, including meropenem and amikacin, were initiated. Ultrasound-guided percutaneous drainage of the collections in the right subhepatic and pelvic regions was performed, along with a right lower moiety percutaneous nephrostomy (PCN). All three tubes drained frank, thick pus. Pus samples from all three tubes tested negative for acid-fast bacilli but showed growth of Escherichia coli.
After patient optimization and cessation of output in the intraperitoneal drains, indicating no intraperitoneal collections (Figure 2A), the patient underwent nephrectomy of the infected, non-excreting right lower renal moiety and ureterolithotomy via a right subcostal loin incision using a retroperitoneal approach. Intraoperatively, dense perinephric adhesions were encountered. A lower moiety ureteric calculus was identified just proximal to its confluence with the ureter of the upper moiety. Ureterotomy over the lower moiety ureteric calculus, extending up to the ureteric confluence, was performed, and stones from both ureters were removed. The ureterotomy was closed over a 6F double-J stent with the proximal coil placed inside the upper moiety. Subcapsular lower moiety nephrectomy was successfully completed (Figure 2B).
The post-operative period was uneventful, and the patient was discharged on the 4th postoperative day. The double-J stent was removed one month after the surgery. At a three-month follow-up, ultrasonography showed that the pelvicalyceal system of the right upper moiety kidney was compact, with maintained corticomedullary differentiation.
3. Discussion
A duplex kidney with incomplete ureteric duplication is the most common congenital anomaly of the urinary tract. Patients with this anomaly are at an increased risk of ureteroureteric reflux, recurrent urinary tract infections, and urolithiasis (3). Pyonephrosis is a rare complication of upper urinary tract obstruction. In cases of voluminous pyonephrosis, the elevated intrarenal pressure may result in forniceal or pelvic rupture, which is typically retroperitoneal as there is no anatomical communication with the peritoneal cavity. However, intraperitoneal fistulization of a pyonephrotic kidney, though extremely rare, is possible. Risk factors for pyonephrosis include immunosuppressive status and anatomical urinary tract obstruction, with 75% of cases being related to urolithiasis (4). In our case, the lower moiety pyonephrosis was caused by an obstructive calculus in the lower moiety ureter. The clinical presentation of a ruptured pyonephrosis may vary depending on the duration and site of rupture. A retroperitoneal collection may lead to a psoas abscess, while an intraperitoneal rupture may result in generalized peritonitis. Our patient presented with features of generalized peritonitis, mimicking a hollow viscus perforation. Forniceal rupture can be diagnosed through contrast extravasation into the retroperitoneum or intraperitoneum on computerized tomography (CT) urogram. However, diagnosis can be challenging, especially when the kidney is non-excreting, as in our case, where the lower moiety was non-excreting.
Jalbani et al. reported a similar case of acute abdomen where the diagnosis of renal forniceal rupture causing peritonitis was made only during laparotomy (5). Different management approaches have been reported by various authors. Shifti and Bekele described a case of intraperitoneal rupture of a pyonephrotic non-functional kidney secondary to pelviureteric junction obstruction, which was managed with exploratory laparotomy and nephrectomy (6). Similarly, E. Anouar and B. Ibrahim reported a case managed with initial percutaneous drainage followed by delayed nephrectomy (7). Adela and Moalwi documented a case of intraperitoneal rupture of pyonephrosis secondary to an obstructive distal ureteric calculus, managed initially with ureteric stenting followed by ureteroscopic lithotripsy (8). In our case, we initiated management with antibiotics and percutaneous drainage using multiple tubes and a lower renal moiety nephrostomy. Subsequently, we performed a nephrectomy of the infected, non-functioning right-sided lower renal moiety along with the removal of the ureteric calculi, successfully preserving the functioning upper renal moiety. The post-operative period was uneventful.
This is the first reported case of intraperitoneal pyonephrosis rupture in a duplex kidney in the literature. Our case also highlights the feasibility of managing such cases with initial percutaneous drainage followed by definitive surgery.
3.1. Conclusions
Spontaneous intraperitoneal rupture of a duplex kidney is an extremely rare occurrence, and the possibility of spontaneous intraperitoneal rupture of pyonephrosis should always be included in the differential diagnosis of generalized peritonitis. Effective management can be achieved through initial percutaneous drainage followed by nephrectomy.