1. Background
Varicocele is defined as a dilation of the Pampiniform venous network of the testis. Varicoceles are diagnosed on physical examination of the scrotum and are graded according to the following scale: Grade I varicocele (palpable only during the Valsalva maneuver), grade II (palpable in the standing position), and grade III (visible without palpation) (1). Varicocele occurs in 15% of adult men after puberty. Thirty-five percent of these individuals experience primary infertility, and 70 to 80% experience secondary infertility. Varicocele is a common cause of male infertility. Despite numerous studies in animals and humans, the exact mechanism by which varicocele causes testicular dysfunction is not fully understood. However, it has been observed that even small changes in temperature can negatively impact spermatogenesis and sperm quality. In animal studies, restoring normal testicular blood flow and repairing varicocele have been shown to improve testicular temperature regulation (2-4). The exact cause of varicocele is not known, but experts have suggested a few theories. One theory is that there is an issue with the valve of the left internal spermatic vein when it connects to the left renal vein. This can cause blood to flow back into the spermatic vein, leading to increased pressure and dilation. Another theory involves the Pampiniform plexus and increased hydrostatic pressure in the left internal spermatic vein due to its longer length compared to the right side. However, some experts disagree with these theories (5-7). The connection between varicocele and the impairment of Leydig cell function in testosterone production is not well understood. Furthermore, the impact of varicocelectomy on enhancing Leydig cell function and testosterone levels in the bloodstream has not been fully established in studies (7). Despite extensive research, none of the theories have been proven. The most widely accepted theory is the impact of heat on the testicles due to a blood circulation disorder. This theory is supported by experiments in animal models which showed that creating varicocele and increasing testicular temperature weakened sperm production. Beyond its mechanism, varicocele appears to play a role in reducing testicular function and sperm quality in many men seeking infertility treatment (8, 9). With changes in the reference ranges and laboratory evaluation methods for human semen, there is a need to clarify the relationships between varicocele and semen parameters. The evidence from animal and human studies suggests that varicocele has an impact on sperm quality. It has been observed that experimental varicocele can lead to dysfunction of the testis and epididymis, affecting both the endocrine and exocrine processes. This may help to explain why men with varicocele often experience infertility. Furthermore, varicocele has been shown to have a negative effect on various sperm parameters, including sperm count, motility, and morphology (10-12). However, only 35 to 50 percent of men who undergo varicocele treatment show a positive semen response to varicocele treatment, and others show a negative response to varicocele treatment due to varicocele recurrence, genetic disorders, and technical failure (13).
2. Objectives
The impact of varicocele on testosterone production and sperm parameters and causing infertility is an important issue; however, this challenge is still a matter of debate. This study aims to examine the effect of varicocelectomy on serum testosterone levels and sperm parameters.
3. Methods
3.1. Study Design
This study was conducted on infertile men with varicocele of any grade who were referred to Golestan and Imam Khomeini hospitals in Ahvaz. A control group, consisting of men without varicocele who have children, was included for comparison. The second group comprised patients with varicocele. This study was conducted based on the ethical protocol of the institution where the research was conducted. Informed consent was obtained from the patient, and all patient information is protected (IR.AJUMS.HGOLESTAN.REC.1402.189). Exclusion criteria for this study included conditions and diseases other than varicocele that can cause testosterone changes. These conditions encompassed cortisone use, malnutrition, acute illness, alcoholism, cirrhosis, diabetes, any cancer, chemotherapy or radiotherapy, obesity, testicular damage, and AIDS. The inclusion criteria were patients with varicocele who did not meet any of the exclusion criteria.
3.2. Determination of Varicocele Grade
The varicocele was graded based on clinical examination. Grade 2 varicocele was diagnosed during the clinical examination without performing the Valsalva maneuver, by palpating the varicose veins without any movement. Grade 3 varicocele, the severe stage of this complication, was determined by the presence of enlarged bluish veins visible from inside the scrotum.
3.3. Testosterone Level Determination
Testosterone levels were determined in the control group and in the group of varicocele patients (before and after varicocelectomy). First, a venous blood sample was taken from the patient, then the samples were centrifuged at 4000 rpm for 10 minutes, and the supernatant containing serum was collected using a sampler and immediately transferred to -20 temperatures. Testosterone serum levels were measured by ELISA method with Monobind kit (Tehran, Iran) according to the manufacturer's instructions.
3.4. Varicocelectomy
Varicocelectomy was performed by subinguinal method. After the operation, a color Doppler ultrasound was performed to check the effectiveness of the operation.
3.5. Analysis of Semen
Semen analysis was done with the SQA II CP sperm analyzer before and after varicocelectomy. Normal semen factors were considered according to World Health Organization (WHO) 2010 reference. SQA II C-P conducted a routine semen analysis to assess sperm concentration (in millions/mL), sperm motility, and sperm morphology. Following the WHO guidelines, participants were categorized into four groups: Normozoospermic, oligozoospermic, asthenozoospermic, and azoospermic. In this study, the number of samples collected from each group was as follows: Normozoospermics – 80, asthenoteratozoospermics (AT) – 25, oligoasthenoteratozoospermics (OAT) – 26, and azoospermics – 19.
3.6. Statistical Analysis
We used Graph Pad Prism version 8 software for all data analysis. A P-value of less than 0.05 indicates a significant difference. First, we used the Kolmogorov-Smirnov test to check for normality of the data. Then, we analyzed the data using an Independent samples t-test or Mann-Whitney U.
4. Results
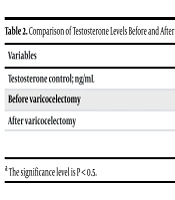
The results of this experimental study are presented as mean ± SEM or percentages with a 95% confidence interval as follows. In this study, the average age of patients with varicocele was 33.06 ± 8.04. Out of the 50 patients participating in this study, 37 had Grade 2 varicocele, and 13 had Grade 3 varicocele (Table 1). Testosterone levels in healthy individuals were significantly higher than those in individuals with varicocele before and after varicocelectomy (Table 2). The testosterone level of the varicocele group was significantly lower before varicocelectomy compared to after varicocelectomy. There was no significant difference in testicular volume before and after varicocelectomy (Table 3). Testosterone levels in the varicocele group before and after varicocelectomy were not found to be correlated with varicocele grade (Table 4). The study results indicated that there was no significant difference in the volume of semen before and after varicocelectomy. Similarly, there was no significant difference in sperm count before and after the procedure. However, the number of rapidly progressive sperms after varicocelectomy was found to be significantly higher than before (P < 0.05). There were no significant differences in sperm survival, concentration, and normal morphology before and after varicocelectomy (Table 5).
| Variables | Mean ± SEM; N = 50 | P-Value a |
|---|---|---|
| Testosterone control; ng/mL | 613.2 ± 25.87 | - |
| Before varicocelectomy | 444.5 ± 27.32 | 0.00 |
| After varicocelectomy | 528.3 ± 29.04 | 0.01 |
Comparison of Testosterone Levels Before and After Varicocelectomy Compared to the Control Group
Effect of Varicocelectomy on Levels of Testosterone and Testis Volume in Patients
| Variables | Varicocele Grade 2 | Varicocele Grade 3 | P-Value a |
|---|---|---|---|
| Testosterone before varicocelectomy | 465.7 ± 31.81 | 373.7 ± 54.03 | 0.14 |
| Testosterone after varicocelectomy | 541.9 ± 32.46 | 463.2 ± 60.41 | 0.23 |
Effect of Varicocele Grade on Levels of Testosterone and Testis Volume in Patients
| Variables | Before Varicocelectomy | After Varicocelectomy | P-Value |
|---|---|---|---|
| Semen volume; mL | 2.90 ± 0.17 | 2.93 ± 0.15 | 0.82 a |
| Sperm count ; 106/mL | 113.6 ± 8.45 | 119.4 ± 7.81 | 0.43 a |
| Motility (rapid) (in 100 examined sperms) | 36.94 ± 1.79 | 44.80 ± 1.40 | 0.00 b |
| Viability (in 100 examined sperms) | 61.81 ± 3.45 | 63.63 ± 4.48 | 0.46 a |
| Functional sperm concentration | 20.76 ± 4.59 | 28.65 ± 4.36 | 0.09 a |
| Normal morphology (in 100 examined sperms) | 37.95 ± 4.08 | 32.85 ± 4.39 | 0.39 a |
Effect of Varicocelectomy on Semen Parameters in Patients
5. Discussion
Varicocele can impair Leydig cell function and is a significant risk factor for hypogonadism. Symptomatic hypogonadal men with varicoceles have two treatment options: Testosterone replacement therapy or varicocele treatment, each with its advantages and disadvantages. About 90% of men on exogenous testosterone remain azoospermic, posing fertility challenges, and 35% may experience irreversible azoospermia even after stopping treatment. For men wanting children, stimulating the hypothalamic-pituitary-testicular axis with gonadotropins and clomiphene citrate can be challenging. The effectiveness of varicocele repair in increasing testosterone levels is uncertain and may vary based on the treatment method and potential complications like recurrence and testicular atrophy (14). The study found that testosterone levels in healthy subjects were significantly higher than in those with varicocele before and after varicocelectomy. Before varicocelectomy, the testosterone level of the varicocele group was significantly lower than after the procedure. There was no significant difference in testicular volume before and after varicocelectomy. Testosterone levels before varicocelectomy did not correlate with varicocele grade, and the same was true for testosterone levels after the procedure. The study also revealed that semen volume, sperm count, normal sperm concentration, and morphology did not differ significantly before and after varicocelectomy. However, there was a significant increase in the number of fast-moving sperm after the procedure. Varicocele affects the secretory function of the Leydig cells in both testicles, leading to a noticeable decrease in testosterone levels. This results in changes in the secretory function of Sertoli cells as well. The decrease in testosterone content in the testis and the activity of androgen-related proteins disrupts spermatogenesis, affecting the sperm maturation process in the epididymis. Testicular testosterone is the main source of testosterone in the epididymis, and varicocele leads to bilateral disorders in the activity of testicular spermatogenesis and sperm maturation in the epididymis. These disorders, along with factors such as reduced acrosin content, oxidative stress, and sperm DNA damage, indicate a link between varicocele and reduced fertility in men (15, 16). There are still some unanswered questions regarding varicocele. While some varicocele patients have abnormal sperm parameters and are infertile, many others have normal sperm parameters and fertility (17). Harrison et al. suggested that complications caused by left varicocele may be due to an increase in testicular extracellular fluid, leading to testicular extracellular edema. This may not occur if there is an efficient testicular lymphatic drainage system. It's also possible that the fertility of some men with varicocele may be temporarily affected, even if they have had children, and they may become infertile at an older age without realizing it (18). To answer the question of improving the quality of semen or the fertility potential of men with varicocele treatment, the results of different studies are very different. For example, the results of a study did not show any significant improvement in sperm parameters, including morphology and progressive movement of sperm in operated men compared to the untreated control group during 53 months (19). On the other hand, the results of different studies have shown that the treatment of varicocele in the population of infertile men suffering from varicocele has improved sperm parameters and fertility rate (20-24). In our study, semen volume, sperm count, normal sperm concentration, and morphology before varicocelectomy did not differ significantly from after varicocelectomy. However, the number of fast-moving sperm after varicocelectomy was significantly higher than before. It has been suggested that varicocelectomy during adolescence can lead to the progressive improvement of testicular growth in affected individuals, and an increase in testicular volume after varicocele treatment has been reported in adolescents. However, varicocelectomy is associated with the risk of wound infection, hydrocele, varicocele recurrence, and rarely testicular atrophy. Scrotal numbness and long-term pain are potential complications of varicocelectomy (25). By performing varicocelectomy in teenagers with hypotrophy of the left testicle before the operation, 69% growth was observed in 28 months (16-26). In our study, the testicular volume after varicocelectomy was not significantly different from that after varicocelectomy, which is due to the short period of testicular volume measurement after varicocelectomy, and it is necessary to examine patients for a longer time. The results of the study suggest that varicocelectomy may improve testosterone levels and enhance sperm motility, although other sperm parameters did not show statistically significant differences. One limitation of our study was the lack of a larger number of patients. More comprehensive studies investigating molecular mechanisms are recommended.