1. Background
Bladder cancer (BC) is a significant global health concern, ranking as the tenth most common cancer worldwide (1). Approximately 75% of BC cases involve non-muscle-invasive bladder cancer (NMIBC) (2). Timely and effective management of NMIBC is crucial to optimize patient outcomes, reduce the risk of recurrence, and prevent progression to muscle-invasive bladder cancer (MIBC) (3). To enhance patient care and improve cost-effectiveness, the use of unnecessary medical interventions should be minimized (4).
To address the challenges associated with NMIBC management, clinical practice guidelines (CPGs) have been developed by numerous national and international organizations (3). Transurethral resection of bladder tumors (TURBT) remains the gold standard for the primary treatment of NMIBC and is the most frequently performed urological cancer surgery (5). Despite the availability of CPGs, adherence to guidelines for NMIBC treatment is generally low, leading to frequent recurrences, often within the first year following primary TURBT (6). These recurrences increase both healthcare costs and patient burden due to the need for repeated surgeries and frequent cystoscopy surveillance (7).
To address the inconsistencies among existing guidelines for NMIBC treatment, four major organizations (American Urological Association/Society of Urological Oncology, European Association of Urology (EAU), National Comprehensive Cancer Network, and National Institute for Health and Care Excellence) developed a unified "Guideline of Guidelines" in 2017, which was subsequently updated in 2020 (8). Adherence to these globally recognized guidelines is expected to improve patient outcomes. Previous studies (N = 10,575 NMIBC patients) investigating urologist treatment patterns through surveys have consistently reported low compliance with NMIBC guidelines worldwide (9, 10). Factors contributing to this discrepancy include physician characteristics, hospital systems, and patient-related factors (11). The gap between implemented treatment and guideline recommendations can adversely affect patient quality of life, prognosis, and outcomes (12).
2. Objectives
Given the significance of this treatment gap and the lack of similar studies in our country, this research aimed to evaluate the compatibility of applied treatment methods for NMIBC patients with established guideline recommendations.
3. Methods
This cross-sectional study analyzed patients with NMIBC treated at Imam Khomeini Hospital, Urmia, Iran, between 2021 and 2022. Urmia Imam Khomeini University Hospital has a Bacillus calmette-guérin (BCG) therapy clinic. This clinic provides post-transurethral resection (TUR) BCG therapy for patients with various urological malignancies, regardless of the treatment center. The prescribing physician determines the appropriate BCG therapy regimen, including dosage and duration. This unique setting offers an ideal opportunity to evaluate the clinical practices of urologists in the province regarding the management of non-invasive bladder tumors, without interfering with the diagnostic, surgical, or post-operative treatment processes. By analyzing prescription patterns and treatment durations, we can assess the compatibility of local clinical practices with established guidelines.
Eligible patients were identified through a review of medical records and recruited using a convenience sampling method. Inclusion criteria were patients with NMIBC treated in the BCG therapy clinic, and exclusion criteria were incomplete medical records, unwillingness to participate in the study, and a history of systemic or intravesical chemotherapy. Informed consent was obtained from all participants prior to data collection. Missing data were supplemented by direct patient interviews. A total of 134 patients met the inclusion criteria and participated in the study.
Data collected included patient demographics (age, sex), medical history (underlying diseases), intravesical therapy details, imaging results (ultrasound, CT scan, cystoscopy), cytology findings, surgical procedures (TURBT, RETURBT, biopsy), and physician experience. Perioperative intravesical chemotherapy with mitomycin C, and post-TURBT BCG therapy including induction and maintenance regimens and durations, were also recorded.
To evaluate treatment adherence to guidelines [the used guidelines are national, American Urology Association (AUA), and EAU guidelines, and the items to be reviewed are similar in all three guidelines], the collected data were compared to the 2019 AUA guidelines for BC (13). While these guidelines are largely similar, the American guideline offers more specific recommendations for intravesical chemotherapy in high-risk patients and the duration of maintenance treatment. In this study, patient risk was categorized according to the American guideline, and standard treatment durations were defined as one year for intermediate-risk patients and three years for high-risk patients (Table 1).
| Groups and Tumor Type | Therapeutic Action |
|---|---|
| Low-risk | Intravesical chemotherapy after TURBT |
| Solitary tumor, LG, Ta and primary < 3 cm | |
| Intermediate- risk | Intravesical chemotherapy after TURBT + induction therapy + maintenance therapy for one year or induction therapy + maintenance therapy for one year |
| Recurrence within 1 year and LG TA | |
| Solitary tumor and LG TA and > 3 cm | |
| Multifocal and LG TA | |
| HG TA and ≤ 3 cm | |
| LG T1 | |
| High-risk | Induction therapy + maintenance therapy for one to three years or radical cystectomy surgery |
| HG T1 | |
| Recurrence and HG TA | |
| HG TA and > 3 cm | |
| CIS | |
| Any BCG failure in HG | |
| Variant histology including micropapillary, plasmacytoid, sarcomatoid, etc. | |
| LVI | |
| Any HG involvement of the prostate urethra |
Abbreviations: LVI, lymphovascular invasion; TURBT, transurethral resection of bladder tumors; BCG, Bacillus calmette-guérin.
Guideline compatibility was evaluated for various treatment components. Compliance was determined as 'compatible' if performed as recommended or 'incompatible' if not. The first four criteria were used for accurate risk stratification, while the remaining focused on treatment strategy compatibility. A scoring system was developed to quantify adherence:
(1) Cystoscopy reporting: Accurate documentation of tumor size, number, location, and shape (0.25 points each).
(2) TURBT and biopsy of base of tumor: Performance of TURBT and submission of tumor base biopsy for pathological examination (1 point each).
(3) Pathological staging and grading: Accurate determination of tumor stage and grade for risk stratification (2 points total).
(4) Urine cytology: Appropriate use of urine cytology in intermediate- and high-risk patients only (1 point).
(5) Intravesical chemotherapy: Correct use of mitomycin C in low-risk patients only (1 point).
(6) Re-TURBT: Timely performance of re-TURBT within 2 - 6 weeks of TURBT in high-grade (T1/Ta) or T1 patients (1 point for low-risk non-adherence, 0.5 points for intermediate/high-risk non-adherence or incorrect timing).
(7) Induction treatment: Appropriate use of BCG vaccine for intermediate- and high-risk patients, initiated within 2 weeks of TURBT and administered weekly for six weeks. Incomplete treatment (less than 6 doses) was considered incompatible (1 point for low-risk non-adherence, 0.33 points for intermediate/high-risk non-adherence or incorrect timing/dosing).
(8) Maintenance treatment: Appropriate duration of maintenance treatment (1 or 3 years) for intermediate- and high-risk patients, respectively (1 point for low-risk non-adherence, 0.5 points for intermediate/high-risk non-adherence or incorrect treatment duration).
This scoring system allowed for a quantitative assessment of guideline adherence.
To calculate the overall guideline adherence score, individual scores for pre-treatment interventions (stages I - IV) and treatment strategies (stages V - VIII) were summed. These scores were then normalized by dividing by their respective maximum values (5 and 4) and multiplying by 100. The combined score was further normalized by dividing by 9 and multiplying by 100, resulting in a final score ranging from 0 to 100. A score of 80 - 100 was considered excellent, 60 - 79 good, and < 60 poor. The frequency of each score category within the study group was reported.
Cystoscopy results were evaluated based on the completeness of reporting. Complete reporting of tumor number, size, site, and shape was considered fully compatible with guidelines. Partial reporting (1 - 3 criteria) was classified as moderately compatible, while reporting only tumor presence without defining characteristics was deemed incompatible. Mitomycin C was recommended for low-risk patients and was also considered an option for intermediate-risk patients. However, its use was contraindicated in high-risk patients.
The study was approved by the Ethics Committee of Urmia University of Medical Sciences (code: IR.UMSU.REC.1399.339), and all participants provided written informed consent. Ethical considerations outlined in the latest version of the Declaration of Helsinki were strictly adhered to throughout the study.
Statistical analysis was performed using IBM SPSS Statistics for Windows version 20.0 (IBM Corp., 2011, Armonk, NY). Descriptive statistics were calculated for all variables. Continuous variables were summarized by mean ± standard deviation, while categorical variables were presented as frequencies and percentages. Independent t-tests were used to compare the means of normally distributed quantitative variables. Fisher's exact test was used to compare the frequencies of categorical variables.
4. Results
Of the 134 participants with a mean age of 65.0 ± 11.5 years, 106 (79.1%) were male. Women (n = 28) had a mean age of 63.4 ± 15.3 years, while men had a mean age of 65.4 ± 10.3 years. There was no significant difference in age between men and women (P = 0.428) (Table 2).
| Variables | Values |
|---|---|
| Mean age (y) b | 45 ± 11.5 |
| Gender | |
| Male | 106 (79.17) |
| Female | 28 (20.93) |
| Place of treatment | |
| University-affiliated centers | 64 (47.8) |
| Private centers | 61 (45.5) |
| Governmental centers | 9 (6.7) |
| History of BC | |
| Yes | 73 (54.5) |
| No | 61 (45.5) |
| Underwent intravesical therapy | |
| Yes | 56 (41.8) |
| No | 78 (58.2) |
| Tumor type | |
| Transitional cell carcinoma | 130 (97) |
| Carcinoma in situ | 4 (3) |
| Tumor number by ultrasound | |
| Indeterminate | 17 (12.7) |
| Single | 68 (50.7) |
| Two | 28 (20.9) |
| Three | 9 (6.7) |
| Four and more | 12 (9) |
| Tumor size by ultrasound | |
| Indeterminate | 18 (13.4) |
| < 3 | 78 (58.2) |
| ≥ 3 | 38 (28.4) |
| Mean tumor size (mm) | 29.1 ± 16.9 |
| Tumor number by cystoscopy | 95 (70.9) |
| Indeterminate | 39 (29.10) |
| Single | 36 (26.9) |
| Two | 19 (14.2) |
| Three | 14 (10.4) |
| Four and more | 26 (19.4) |
| Tumor size by cystoscopy | 70 (52.2) |
| < 3 | 49 (70) |
| ≥ 3 | 21 (30) |
| Mean tumor size (mm) | 28.9 ± 13.5 |
| Tumor site by cystoscopy | 40 (29.9) |
| Tumor shape by cystoscopy | 38 (28.4) |
| TURBT performed during cystoscopy | |
| Tissue sampling | 61 (45.5) |
| Tumor size by pathology | |
| < 3 | 96 (71.6) |
| ≥ 3 | 28 (28.4) |
| Mean tumor size (mm) | 26.4 ± 12.9 |
| Tumor grade by pathology | |
| TA | 81 (60.4) |
| T1 | 53 (39.6) |
| Tumor stage by pathology | |
| Low | 97 (72.4) |
| High | 37 (27.6) |
Abbreviations: TURBT, transurethral resection of bladder tumors; BC, bladder cancer.
a Values are expressed as No. (%) unless otherwise indicated.
b There was no significant difference in age between men and women (P = 0.428).
Most patients were treated at university-affiliated centers (n = 64, 47.8%) or private centers (n = 61, 45.5%), with only 9 (6.7%) receiving treatment at governmental centers. A positive history of BC was reported in 73 patients (54.5%), of whom 41.8% (n = 56) underwent intravesical therapy. The predominant tumor type was transitional cell carcinoma in 130 patients (97%), with only a few cases (n = 4, 3%) of carcinoma in situ (Table 2).
Ultrasound examination revealed that tumor number was indeterminate in 17 patients. Among the remaining patients, 68 (50.7%) had a single tumor, 28 (20.9%) had two, 9 (6.7%) had three, and 12 (9%) had four or more tumors (Table 2).
Tumor size was not determined in 18 patients. In the remaining 116 patients, the mean tumor size was 29.1 ± 16.9 mm (range: 5 - 90 mm). Of these, 78 patients had a tumor size less than 3 cm as measured by ultrasound (Table 2).
All patients underwent cystoscopy. Of the 134 patients, tumor number was reported in 95 (70.9%), size in 70 (52.2%), site in 40 (29.9%), and shape in 38 (28.4%). Among the 95 patients with determined tumor numbers, 36 (26.9%) had a single tumor, 19 (14.2%) had two, 14 (10.4%) had three, and 26 (19.4%) had four or more tumors. The mean tumor size was 28.9 ± 13.5 mm (range: 10 - 70 mm), with 49 patients having a tumor size less than 3 cm (Table 2).
Transurethral resection of bladder tumors was performed for all patients during cystoscopy. However, tissue samples from the base of the tumor were obtained in only 61 patients (45.5%), indicating partial compliance with guidelines. Pathological examination revealed a mean tumor size of 26.4 ± 12.9 mm (range: 5 - 60 mm), with 96 patients having tumors less than 3 cm. The majority of patients (60.4%, n = 81) had stage Ta tumors, while the remaining had stage T1 tumors. In terms of tumor grade, 72.4% (n = 97) were classified as low grade, and the remaining 27.6% (n = 37) were classified as high grade (Table 2).
Using the risk stratification criteria outlined in the methodology, 34 patients (25.4%) were classified as high-risk, 18 (13.4%) as low-risk, and 82 (61.2%) as intermediate-risk. The frequency of urine cytology performed within each risk group is presented in Table 2. Adherence to guidelines for urine cytology was observed in 59.7% of patients (36 / 61) who were intermediate- or high-risk. However, when considering the recommendation to avoid urine cytology in low-risk patients, the overall guideline compatibility for urine cytology was 40.3% (Table 3).
| Groups | Cytology | ||
|---|---|---|---|
| Total Number | Not Performed | Performed | |
| Low-risk group | 18 | 18 (100) | 0 |
| Intermediate-risk group | 82 | 64 (78) | 18 (22) |
| High-risk group | 34 | 16 (47.1) | 18 (52.9) |
| Intermediate- and high-risk group | 116 | 80 (69) | 36 (31) |
Guidelines indicated re-TURBT for 60 patients. However, among the 37 patients with high-grade tumors (Ta/T1), re-TURBT was performed in only 11 (29.7%), and among the 23 patients with low-grade T1 tumors, it was performed in only 7 (30.4%). This resulted in an overall compatibility rate of 30% for re-TURBT performance in patients with indications. Additionally, 43 patients with indications did not undergo re-TURBT, further reducing compatibility to 32.1%. Conversely, 72 patients without indications underwent re-TURBT, leading to a compatibility rate of 67.9%. Regarding the timing of re-TURBT, 19 patients underwent the procedure within the recommended timeframe, with 14 (73.7%) performed appropriately and 5 (26.3%) performed after 6 weeks (Table 4).
| Variables | Re-TURBT Not Performed (N = 115) | Re-TURBT Performed (N = 19) | Total |
|---|---|---|---|
| High-grade tumor | |||
| Ta | 6 | 1 | 7 |
| T1 | 20 | 10 | 30 |
| Low-grade tumor | |||
| Ta | 73 | 1 | 74 |
| T1 | 16 | 7 | 23 |
Abbreviation: TURBT, transurethral resection of bladder tumors.
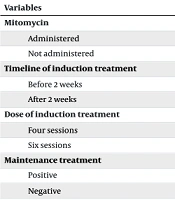
The frequency of mitomycin C administration is presented in Table 4. According to guidelines, mitomycin C is recommended for low-risk patients and may be considered for intermediate-risk patients. However, among the 18 patients treated with mitomycin C, only 1 was classified as low-risk, while 13 were intermediate-risk. Conversely, 17 low-risk patients did not receive mitomycin C, resulting in a compatibility rate of 14.7%. Additionally, 4 high-risk patients were treated with mitomycin C, which is not recommended. This indicates an overall compatibility rate of 15.7% for mitomycin C treatment in relation to guidelines (Table 5).
| Variables | Low-Risk Group (n = 18) | Intermediate-Risk Group (n = 82) | High-Risk Group (n = 34) |
|---|---|---|---|
| Mitomycin | |||
| Administered | 1 (5.6) | 13 (15.9) | 4 (11.8) |
| Not administered | 17 (94.4) | 69 (84.1) | 30 (88.2) |
| Timeline of induction treatment | |||
| Before 2 weeks | 1 (5.6) | 7 (8.5) | 1 (2.9) |
| After 2 weeks | 17 (94.4) | 75 (91.5) | 33 (97.1) |
| Dose of induction treatment | |||
| Four sessions | 0 | 1 (1.2) | 0 |
| Six sessions | 18 (100) | 81 (91.5) | 34 (100) |
| Maintenance treatment | |||
| Positive | 1 (5.6) | 43 (52.4) | 21 (61.8) |
| Negative | 17 (94.4) | 39 (47.6) | 13 (38.2) |
| Duration of maintenance treatment | |||
| One year | 1 (5.6) | 42 (51.2) | 6 (17.6) |
| Three years | 0 | 1 (1.2) | 15 (44.1) |
| Compatibility of total treatments | |||
| Good | 0 | 13 (15.9) | 13 (38.2) |
| Intermediate | 4 (22.2) | 31 (37.8) | 9 (26.5) |
| Poor | 14 (77.8) | 38 (46.3) | 12 (35.3) |
Induction therapy was administered to all patients in this study, demonstrating an 86.6% adherence to guidelines. While not indicated for low-risk patients (n = 18), induction therapy was initiated prior to the recommended 2-week timeframe in 8 of 82 patients (7/75 intermediate-risk, 1/34 high-risk), resulting in a 93.1% adherence rate for timing. The prescribed dosage was compatible in 99% of cases (Table 5).
Maintenance therapy was administered to 43 of 82 intermediate-risk patients (52.4%) and 21 of 34 high-risk patients (61.8%), as well as 1 of 18 low-risk patients (5.6%). Overall, maintenance therapy was performed in 55% of patients with indications. The duration of maintenance therapy is detailed in Table 4, with an overall adherence rate of 55.2%.
Overall adherence to guidelines was evaluated for both pre-treatment interventions and treatment strategies. Findings indicated that 25.4% of patients (n = 34) exhibited good compatibility with pre-treatment guidelines, while only 11.2% (n = 15) demonstrated good adherence to treatment strategies (total: 26 patients, 19.4%). Moderate compatibility was observed in 42.5% (n = 57) of patients for pre-treatment interventions and 38.1% (n = 51) for treatment strategies (total: 44 patients, 32.8%). However, poor compatibility was more prevalent, with 32.1% (n = 43) exhibiting poor adherence to pre-treatment interventions and 50.7% (n = 68) demonstrating poor adherence to treatment strategies (total: 64 patients, 47.8%). The distribution of overall treatment strategy compatibility based on patient risk is summarized in Table 5.
5. Discussion
Clinical practice guidelines are evidence-based recommendations designed to optimize patient care (14). These guidelines are developed through a systematic review of the available evidence and a careful assessment of the potential benefits and harms of various treatment options (15). By promoting standardized and evidence-based practices, CPGs can help to reduce unwarranted variations in care, facilitate the translation of research findings into clinical practice, and ultimately improve healthcare quality and patient safety when developed and implemented according to international standards (14). Given the importance of CPGs, it is reasonable to expect a high degree of alignment between medical practice and guideline recommendations. However, this study evaluated the extent to which diagnostic and treatment strategies implemented at the study centers were compatible with two (international and national) guidelines.
To date, a comprehensive comparative analysis of clinical guideline development and utilization practices across European countries is lacking. The most systematic attempt to address this issue remains the 2011 survey conducted by Legido-Quigley et al. This survey involved 80 respondents from 29 European countries and explored various aspects of clinical guideline development, including the regulatory framework, development process, quality control mechanisms, implementation strategies, and evaluation methodologies (16).
The majority of European countries lacked a formal legal framework for the development and implementation of clinical guidelines (14). Only 13 countries reported having an officially established mechanism for guideline development, although implementation often remained voluntary (17). Notable examples include the French Health Authority (Haute Autorité de Santé, HAS) (18) and the National Disease Management Guidelines Programme in Germany (Programm für Nationale Versorgungsleitlinien, NVL) (19). These organizations are responsible for developing, disseminating, and evaluating clinical guidelines within their respective healthcare systems. While France has established national regulations for clinical guideline development, adherence to these guidelines is not mandatory, and initial efforts to enforce compliance through financial penalties were discontinued. In Germany, the NVL program is jointly managed by the German Medical Association, the National Association of Statutory Health Insurance Physicians, and the Association of the Scientific Medical Societies in Germany. These organizations represent the highest authorities in the self-governance of physicians in Germany and play a crucial role in the development and implementation of clinical guidelines.
The present study compared the proposed guidelines (13) with the current practices of urologists at Urmia Imam Khomeini Hospital. While similarities were observed, discrepancies were also evident. Ultrasound and cystoscopy were the most commonly used diagnostic methods (12), aligning with current practice. However, complete reporting of all four tumor characteristics (number, size, site, and shape) during cystoscopy was observed in only 15.7% of patients, indicating a significant gap. Cystoscopy is an invasive procedure associated with potential complications, including urinary tract infection, bleeding, bladder perforation, scar tissue formation, and urinary retention, particularly in men with pre-existing urinary problems (20, 21).
For accurate diagnosis and tumor grading, TURBT is a crucial diagnostic modality. Transurethral resection of bladder tumors enables risk stratification and can inform prognostication and long-term outcomes (22), guiding subsequent treatment decisions. Complete TURBT is the preferred initial treatment for any bladder tumor (23), followed by instillations based on risk stratification in NMIBC. A second TURBT may be considered for high-risk NMIBC tumors, either before or after intravesical therapy (24). In cases with very high-risk features, such as multiple grade 3 T1 tumors with TIS or increased depth of invasion, cystectomy may be warranted (25). For TIS or high-grade T1 tumors that fail BCG therapy, cystectomy should be considered due to the high risk of progression (26).
In our study, primary TURBT was performed for all patients, aligning with guideline recommendations. However, tissue sampling from the tumor base was only performed in 45.5% of cases. A cohort study in Iceland, including only patients with confirmed NMIBC based on TURBT, reported a 62% adherence rate to guidelines regarding sample resection from the tumor base during primary TURBT (27), which is higher than the rate observed in our study.
Another area of low adherence identified in this study was urine cytology (28). A previous study of 4545 BC patients found that 42% of urologists failed to perform at least one cytology, with only one patient receiving all recommended cytology procedures (29). In the present study, cytology was not performed in all patients with intermediate or high risk, resulting in a 40% incompatibility rate with guidelines, similar to the findings of Chamie et al. (29). A review of 7896 physicians' perspectives from nine European countries revealed that urine cytology was used in 30 - 70% of intermediate-risk and 50 - 80% of high-risk NMIBC patients (12), aligning with the present study and indicating low guideline adherence in this regard.
Conversely, some studies have reported overuse of cytology, particularly in low-risk patients, with rates as high as 60% in France, Italy, and Austria and 10 - 40% in other countries (12). This excessive use can lead to resource depletion and potentially mislead physicians in treatment decision-making. A study conducted in New York reported that 53% of patients underwent routine urine cytology, exceeding recommended usage, particularly in low-risk groups (30). Fortunately, our study demonstrated adherence to guidelines, as urine cytology was not performed in low-risk patients. It is important to emphasize that urine cytology should be ordered only when indicated and avoided as a routine procedure (31).
Given the high rate of residual tumor after primary TURBT (approximately 42%) (26), guidelines recommend re-TURBT for patients with high-grade (T1/Ta) or T1 tumors within 2 - 6 weeks of the initial procedure. In our study, the overall compatibility for performing re-TURBT was 30%, indicating poor adherence. Rates of re-TURBT performance vary across countries, with some reporting rates as high as 76 - 98% and others reporting lower rates (49 - 55%) for high-risk patients (12). Additionally, some studies have reported re-TURBT rates of 67 - 75% in patients with T1 tumors (27). Similar to our findings, these studies suggest that re-TURBT may be performed in a higher proportion of low-risk patients than necessary (12), potentially indicating incomplete resection during primary TURBT or inappropriate treatment decisions.
The clinical knowledge and experience of the medical team play a crucial role in optimizing treatment outcomes (32). A study in France involving 410 NMIBC patients found that 37% of high-risk patients (with indications) underwent re-TURBT, with patient and urologist factors influencing these decisions (6). Other studies have reported much lower rates (10 - 20%) for re-TURBT in high-risk patients (33). As re-TURBT is essential for successful radical surgery, it is crucial to perform this intervention in patients with the recommended indications (34).
Mitomycin C instillation should be performed only when indicated, considering the potential complications associated with this chemotherapy (35). In the present study, overall compatibility with mitomycin C guidelines was 15.7%. Studies have reported varying rates of mitomycin C use across different regions, with lower rates in northeastern countries and higher rates in Asian and other countries (29). Some studies have reported routine perioperative mitomycin C use after TURBT in up to 63% of patients (36), which is significantly higher than the rate observed in our study. Another study found that only 7.5% of low-risk patients received a single dose of chemotherapy with mitomycin C (9). In a French study, only 14% of intermediate-risk patients received mitomycin C (6). Additionally, some studies have reported single-dose chemotherapy in 21 - 74% of high-risk patients, which is contrary to guidelines (9).
Both underuse and overuse of mitomycin C can have significant implications. Therefore, it is essential for urologists to adhere to the recommended guidelines for its administration.
Several studies have suggested comparable efficacy between chemotherapy and induction therapy in terms of disease recurrence, progression, and patient survival (37, 38). In cases of failed BCG treatment, alternative therapies such as chemotherapy or interferon may be considered (39). Bacillus calmette-guérin is a widely used intravesical treatment and is considered the standard of care (40). The mechanism of action involves the internalization of BCG into resident immune cells, normal cells, and tumor urothelial cells, leading to the activation of innate immunity (including cellular immunity and cytokines) (41).
The results of the present study demonstrated high compatibility for induction therapy (93%) and maintenance therapy (70%) in indicated patients, indicating moderate-to-good adherence. Other studies have reported similar rates of induction therapy with BCG in NMIBC patients, with one study finding a 94% adherence rate (36). However, a study conducted in the United States observed induction therapy in only 59% of high-risk patients (11). Additionally, some studies have reported as low as 26% or 24% compliance rates for postoperative BCG instillation (29, 41).
Regarding maintenance therapy, while our study found acceptable rates [similar to those reported in other studies (9, 12)], some have reported low rates as low as 15% (6). Given the critical role of effective treatment in patient outcomes, it is imperative to prioritize adherence to guidelines for both induction and maintenance therapies.
5.1. Strengths and Limitations of the Study
A limitation of this retrospective study is the difficulty in determining the precise reasons for guideline deviations. Additionally, the study did not include regional comparisons, did not correlate data with demographic variables, did not evaluate intermediate tumors in depth, lacked a detailed review of pathological data, and did not investigate factors influencing treatment decisions, such as access to ideal treatment, financial constraints, patient preferences, or urologist preferences.
The study benefits from a diverse patient population, including referrals from various academic urologists and both private and public hospital physicians. This broad patient base provides a comprehensive representation of clinical practices in Urmia. Additionally, the researcher's lack of involvement in patient treatment and the absence of bias in questionnaire-based studies enhance the objectivity and reliability of the findings.
5.2. Conclusions
The present study revealed suboptimal adherence to guidelines across various aspects of NMIBC management, particularly in low-risk patients. A wide gap between guideline-recommended treatment and routine practice was observed, which may be attributed to patient-related factors, urologist decisions, or a lack of available resources. Despite these findings, higher compatibility rates were noted in certain therapeutic areas.
Given the critical impact of guideline adherence on patient outcomes, it is imperative to prioritize efforts to enhance urologists' knowledge and ensure the appropriate implementation of guideline recommendations. Strategies to improve guideline adherence at the care provider level are urgently needed. Guideline courses at national and international meetings, national adoption of international guidelines, regular updates of the AUA and EAU guidelines, and increased use of social media could all serve to increase awareness. Ultimately, patients deserve the benefits of optimal, evidence-based treatment.
Future research should investigate the factors associated with non-adherence to specific aspects of NMIBC diagnosis and treatment to identify and address the underlying obstacles that impede guideline implementation.