1. Background
Hypospadias, one of the most common congenital anomalies of the male genitalia, is characterized by the abnormal ventral placement of the urethral meatus proximal to its typical anatomical position (1). In Iran, the prevalence of hypospadias is estimated at 4 per 1,000 live births (2). The optimal timing for surgical intervention is generally between 6 and 12 months of age, although some studies suggest that surgery can be performed up to 36 months with comparable outcomes (3).
Tubularized incised plate (TIP) urethroplasty is a widely adopted surgical technique for hypospadias repair. In this procedure, a U-shaped incision is made along the ventral aspect of the penis, flanking the urethral plate, and extending distally toward the urethral meatus. The incised edges are then tubularized to create a neourethra. A critical aspect of TIP urethroplasty is the coverage of the suture line to prevent complications, such as urethral fistula and meatal stenosis.
The Byars flap, utilized in approximately 95% of hypospadias cases, is a common method for ventral coverage. This technique involves dividing the prepuce into two flaps through a midline incision, which are then transposed ventrally to cover the neourethra (4-8). However, the Byars flap technique has limitations, particularly the alignment of its suture line with that of the TIP procedure, which may increase the risk of fistula formation. In contrast, the buttonhole flap technique preserves the prepuce intact, allowing for potential reuse in cases of postoperative complications, such as fistula formation. This distinction underscores the theoretical advantage of the buttonhole flap over the Byars flap in reducing complications.
Despite the widespread use of the Byars flap, there is limited comparative evidence on the efficacy of alternative techniques, such as the buttonhole flap, in minimizing postoperative complications. This study aims to address this gap by evaluating the buttonhole flap as a potential alternative to the conventional Byars flap technique.
2. Objectives
2.1. Hypotheses
(1) The preputial buttonhole flap technique is associated with a lower incidence of urethral fistula compared to the Byars flap technique.
(2) The incidence of meatal stenosis is not significantly different between the two techniques.
The present study primarily aimed to compare the postoperative complications associated with the buttonhole flap and Byars flap techniques in hypospadias repair. Specifically, we aimed to assess the incidence of urethral fistula, meatal stenosis, and the need for repeat surgery in patients treated at Imam Reza Hospital in Ardabil, Iran, between 2020 and 2021.
2.2. Study Setting
This cohort study was conducted at Imam Reza Hospital, affiliated with Ardabil University of Medical Sciences, in Ardabil, Iran, between January 2020 and December 2021.
3. Methods
3.1. Study Population and Sampling
This study included all patients aged 12 - 36 months diagnosed with hypospadias who were referred to Imam Reza Hospital in Ardabil, Iran, for reconstructive surgery between 2020 and 2021. A total enumeration sampling method was employed, ensuring that all eligible patients undergoing hypospadias repair during the study period were included. The final sample consisted of 40 patients, with 20 patients undergoing surgery using the preputial buttonhole flap technique and the remaining 20 treated with the Byars flap method. Allocation to the two techniques was randomized.
3.2. Surgical Techniques
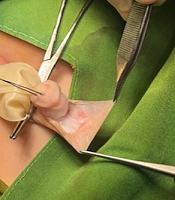
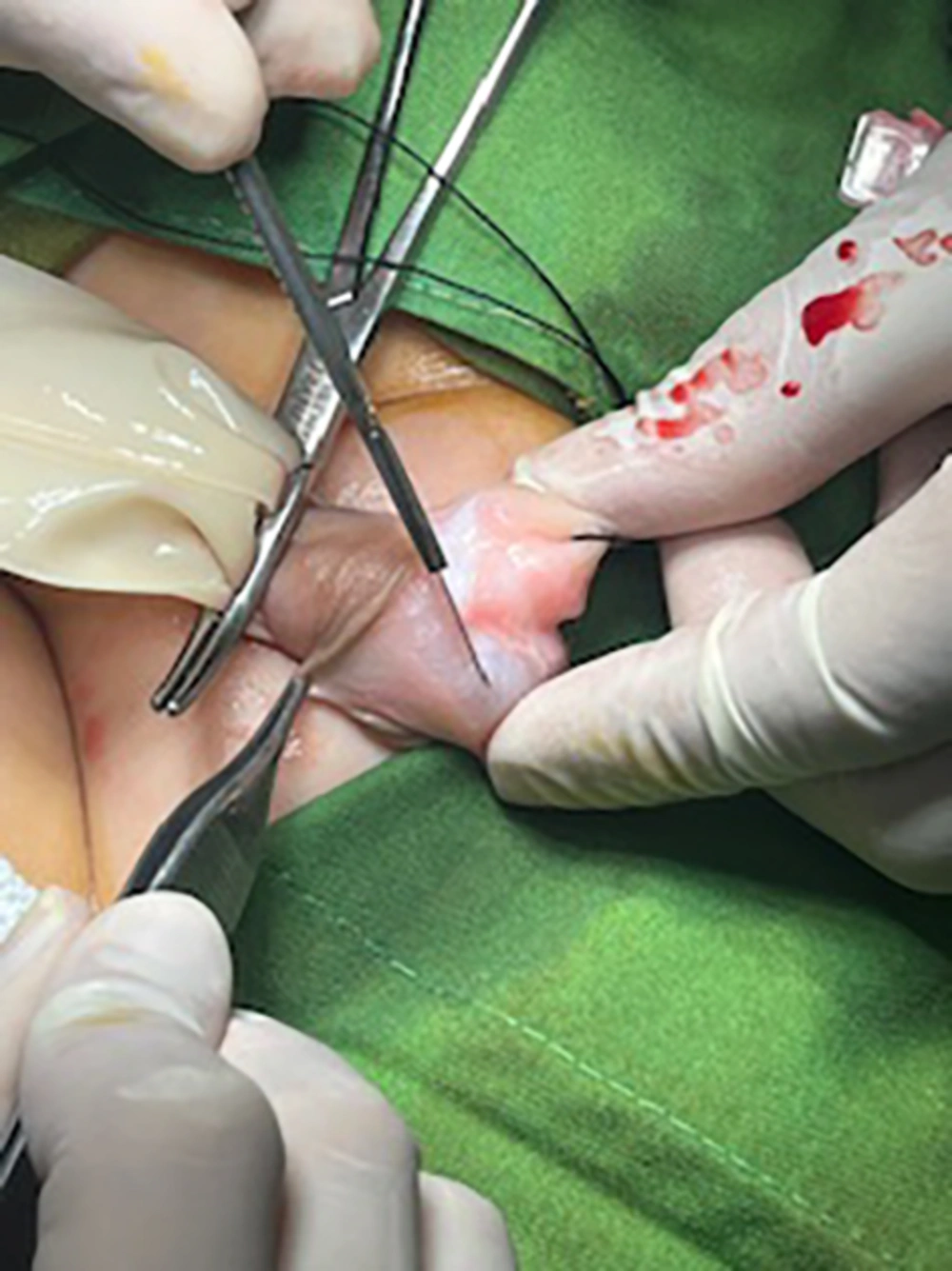
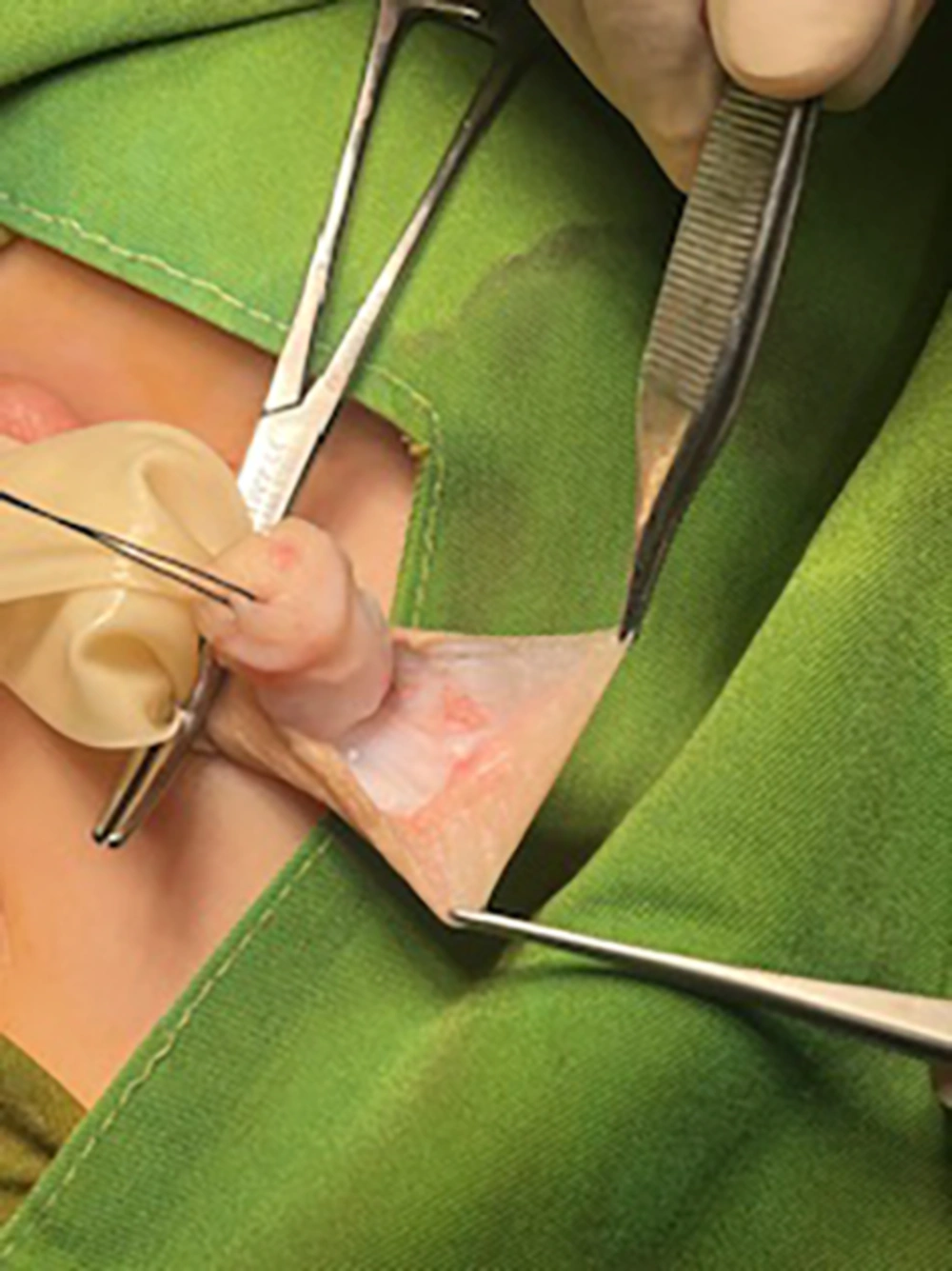
All patients underwent urethroplasty using the Snodgrass (TIP) technique. For skin coverage, the preputial buttonhole flap technique was used in half of the cases, while the Byars flap method was employed in the other half. The preputial buttonhole flap technique involved preserving the prepuce intact, whereas the Byars flap technique required dividing the prepuce into two flaps, which were then transposed ventrally to cover the neourethra. Figures 1 - 5 provide a detailed illustration of the buttonhole flap surgical technique.
3.3. Data Collection and Outcome Measures
Data were collected prospectively using a standardized checklist during a six-month postoperative follow-up period. The primary outcomes assessed included wound infection, penile rotation, urethral fistula formation, and meatal stenosis.
3.4. Statistical Analysis
Data were analyzed using SPSS version 21. Descriptive statistics were used to summarize patient demographics and clinical characteristics. Comparative analyses between the two surgical techniques were performed using the chi-square test, Fisher’s exact test, and Mann-Whitney test, as appropriate. A P-value of less than 0.05 was considered statistically significant.
3.5. Ethical Considerations
The study was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki. Patient confidentiality was maintained throughout the study, with all data anonymized and accessible only to the physician and project manager. The study protocol was approved by the Institutional Review Board of Ardabil University of Medical Sciences (IR.ARUMS.MEDICINE.REC.1401.093).
4. Results
This study included 40 patients who underwent reconstructive surgery for hypospadias. The patients’ ages ranged from 12 to 36 months, with a mean age of 26.1 ± 8.5 months. Medical records indicated that one patient had a history of cryptorchidism, while the remaining patients had no documented comorbidities. The majority of the patients (n = 37, 92.5%) presented with distal hypospadias, while three patients (7.5%) had proximal hypospadias. All three patients with proximal hypospadias were treated using the buttonhole flap technique.
4.1. Definition of Hypospadias Categories
In this study, distal hypospadias was defined as a meatus location distal to the coronal sulcus, while proximal hypospadias included penoscrotal, scrotal, and perineal locations.
4.2. Postoperative Complications
Postoperative complications included meatal stenosis in 11 patients (27.5%) and urethral fistula in seven patients (17.5%). No cases of penile rotation or wound infection were observed in the cohort.
4.3. Demographic Data
Demographic data, including age, weight, height, BMI, and socioeconomic status of the families, were collected and compared, with no significant differences found between the two groups.
5. Discussion
This study aimed to compare the complications associated with two surgical techniques for hypospadias repair: The preputial buttonhole flap and the Byars flap. The primary focus was on the occurrence of urethral fistula, a common complication following conventional hypospadias repair. Theoretically, the buttonhole flap technique is associated with a lower risk of fistula formation due to its unique approach to covering the suture area.
5.1. Statistical Power
The statistical power of this study was calculated to be 0.7, indicating a moderate ability to detect true differences between the two surgical techniques.
5.2. Comparative Analysis of Surgical Techniques
The buttonhole flap technique involves creating a hole in the prepuce and transposing it to the ventral aspect of the penis for suturing. This method has been reported to yield favorable outcomes, including reduced penile rotation and improved cosmetic results. In our study, out of 20 patients treated with the buttonhole flap technique, seven (35%) developed meatal stenosis, and two (10%) developed a urethral fistula. Notably, both patients who developed a urethral fistula had proximal hypospadias, while none of the patients with distal hypospadias experienced this complication. This finding aligns with previous studies, which have consistently reported a higher incidence of urethral fistula in proximal hypospadias compared to distal hypospadias (9, 10).
In contrast, among the 20 patients treated with the Byars flap technique, five (25%) developed a urethral fistula, and four (20%) developed meatal stenosis. Although the incidence of urethral fistula was higher following the Byars flap technique compared to the buttonhole flap technique, this difference was not statistically significant (P = 0.407). However, when considering only distal hypospadias, the buttonhole flap technique demonstrated a clear advantage, with no cases of urethral fistula compared to five cases (25%) in the Byars flap group. This difference was statistically significant, suggesting that the buttonhole flap technique may be more effective in preventing fistula formation in distal hypospadias (Table 1).
| Study | Technique | Sample Size | Urethral Fistula (%) | Meatal Stenosis (%) | Key Findings |
|---|---|---|---|---|---|
| Present study | Buttonhole flap | 20 | 10 | 35 | Higher meatal stenosis; no fistula in distal hypospadias |
| Present study | Byars flap | 20 | 25 | 20 | Higher fistula rate in distal hypospadias compared to buttonhole flap |
| South Korea (11) | Buttonhole flap | N/A | N/A | N/A | Success rates: 87% (glandular), 77% (coronal), 66% (midshaft), 50% (penoscrotal) |
| Serbia (12) | Dorsal Dartos flap | N/A | 0 | N/A | Effective in preventing fistula; meatal stenosis managed by dilatation |
| Germany (13) | Buttonhole flap | 41 | 9.8 | N/A | Urethrocutaneous fistula in 4 cases |
| Iraq (14) | Dorsal Dartos flap | 35 | 2.8 | 8.5 | Low fistula rate; meatal stenosis in 8.5% of cases |
Summary of Key Findings and Comparative Studies a
5.3. Confidence Intervals
The 95% confidence interval for the difference in fistula rates between the Byars flap and buttonhole flap techniques in distal hypospadias was -52.3% to -2.7%, further supporting the potential benefit of the buttonhole flap technique.
5.4. Comparison with Previous Studies
Our findings are consistent with several studies that have evaluated the outcomes of the buttonhole flap technique. For instance, a South Korean study (11) reported an overall success rate of 75% for the buttonhole flap technique, with success rates varying by hypospadias type (87% for glandular, 77% for coronal, 66% for midshaft, and 50% for penoscrotal). Similarly, a Serbian study (12) highlighted the effectiveness of the dorsal dartos flap, transposed using the buttonhole technique, in preventing fistula formation. These studies, along with others from Germany (13) and Iraq (14), have consistently identified urethrocutaneous fistula as the most common complication, with meatal stenosis being the second most frequent. A systematic review and meta-analysis by Wu et al. (15) further corroborated our findings, identifying urethral fistula as the most common complication following hypospadias repair. This aligns with our observation that the incidence of urethral fistula was significantly higher in proximal hypospadias (P = 0.02), with an incidence-to-non-incidence ratio of 2.0 compared to 0.15 in distal hypospadias.
5.5. Age as a Risk Factor
Our study also identified age as a significant risk factor for postoperative complications. The mean age of patients who developed a urethral fistula (29 ± 6.8 months) was significantly higher than that of patients who did not (18.7 ± 8.26 months; P = 0.034). Similarly, the mean age of patients who developed meatal stenosis (22.32 ± 8.8 months) was higher than that of patients who did not (19.81 ± 8.47 months), although this difference was not statistically significant (P = 0.55). These findings suggest that delaying surgery may increase the risk of complications, particularly urethral fistula. However, this contrasts with the findings of Snyder et al. (16), who reported no correlation between patient age and complication rates (Table 2).
5.6. Conclusions
This study compared the outcomes of the preputial buttonhole flap technique and the Byars flap method for hypospadias repair, focusing on postoperative complications such as urethral fistula and meatal stenosis. The findings revealed no significant difference in the overall incidence of urethral fistula and meatal stenosis between the two techniques. However, for distal hypospadias, the buttonhole flap technique demonstrated a significantly lower incidence of urethral fistula compared to the Byars flap method. In contrast, proximal hypospadias was associated with a significantly higher risk of fistula formation, underscoring the complexity of surgical repair in these cases.
Additionally, older age at the time of surgery was identified as a significant risk factor for postoperative fistula formation, suggesting that delayed surgical intervention may increase the likelihood of complications. These findings highlight the importance of early surgical repair and the potential advantages of the buttonhole flap technique for distal hypospadias. Further studies with larger sample sizes and longer follow-up periods are needed to validate these results and refine surgical approaches for hypospadias repair.
5.7. Limitations
This study has several limitations, including a small sample size, a relatively short follow-up period, and the lack of data on long-term cosmetic outcomes. The absence of proximal hypospadias cases treated with the Byars flap technique further limits the generalizability of our findings. Additionally, because the study was conducted at a single center with a relatively homogeneous population, the findings may not be generalizable to broader, more diverse populations. Variation in surgical expertise and postoperative care across institutions could influence outcomes, and future multicenter studies are warranted to validate and generalize these findings. The relatively short follow-up period may not capture late-onset complications or long-term functional and cosmetic outcomes. Future studies with larger sample sizes and longer follow-up periods are needed to confirm these results and provide more robust evidence.
5.8. Generalizability
The results of this study may be most applicable to settings with similar patient populations and surgical expertise.