1. Introduction
Renal lymphangiectasia is a rare renal condition characterized by dilatation of perirenal, per pelvic, and intrarenal lymphatic vessels (1, 2). This condition can be found in children and adults of both sexes and can be unilateral or bilateral (3-5). Isolated case reports are the only available source of information about this condition. Familial, developmental, and acquired causes have been suggested. Clinical signs and symptoms are non-specific and characteristic findings on ultrasonography (USG), computerized tomography (CT), and magnetic resonance imaging (MRI) arethe mainstay of diagnosis.
2. Case Presentation
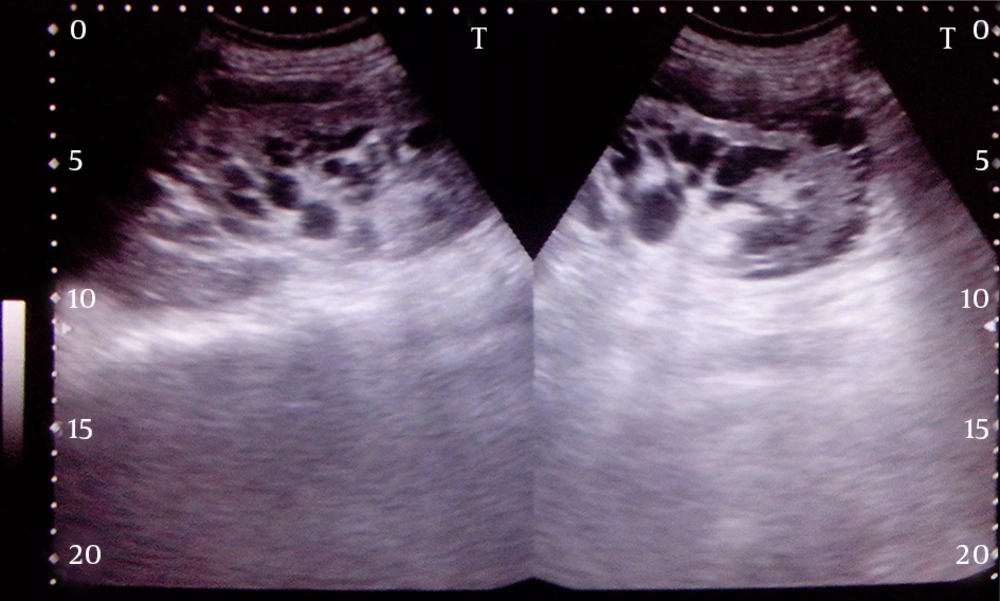
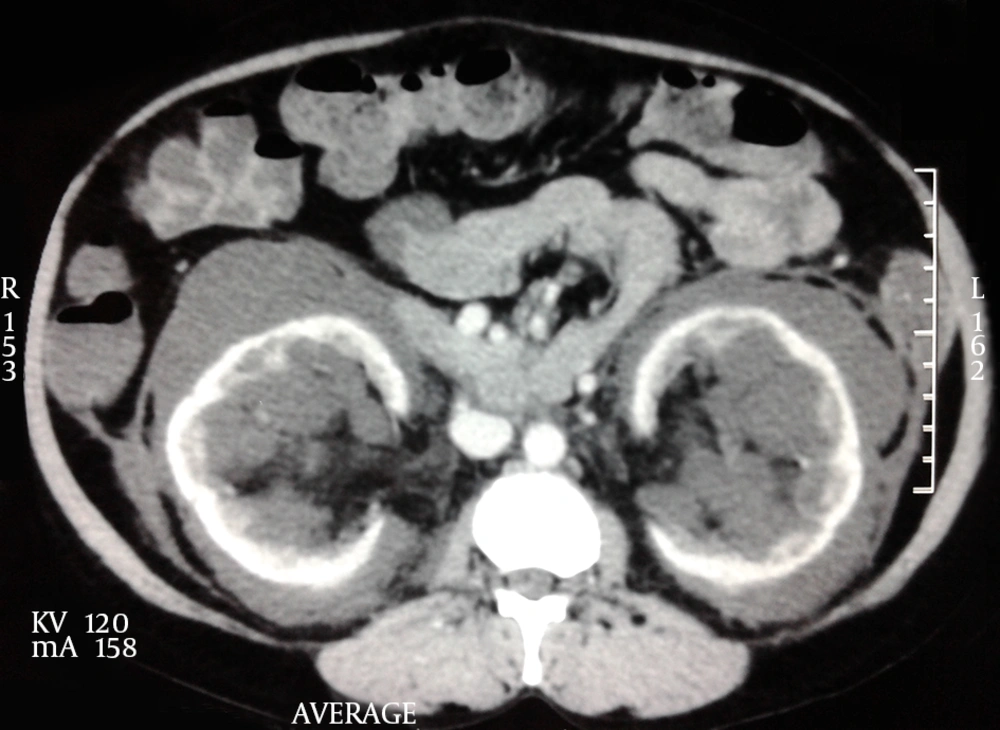
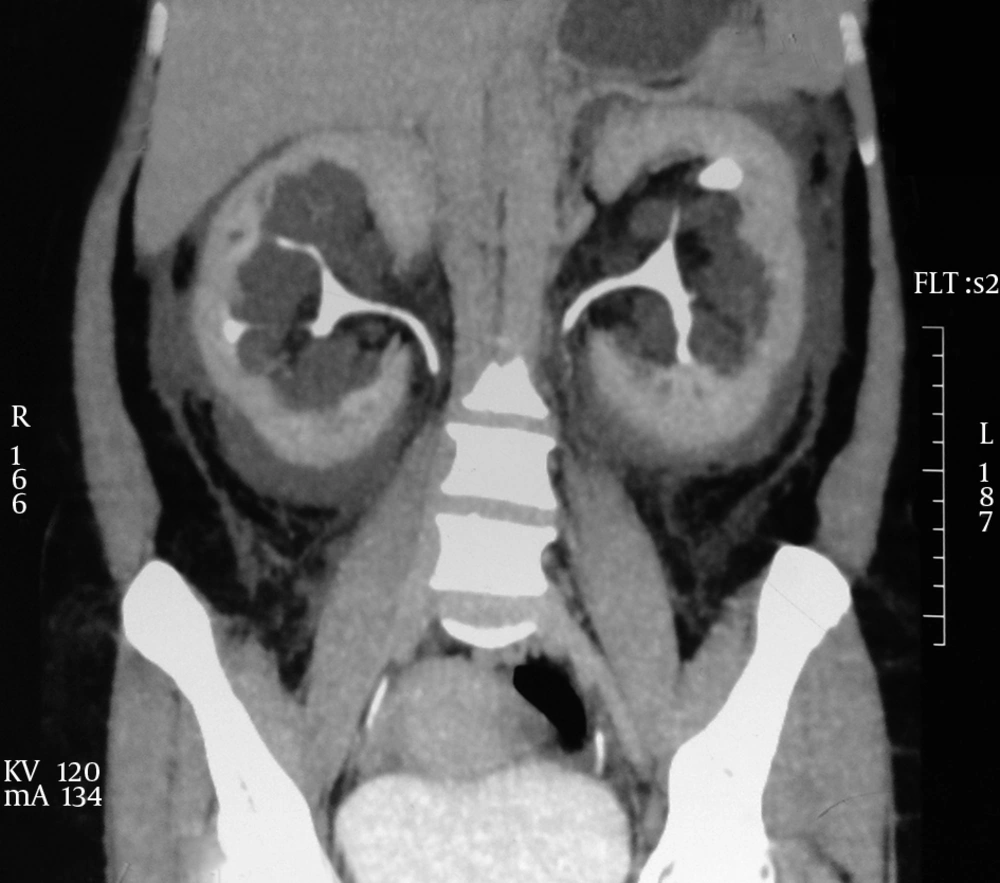
A 32-year-old womanpresented with recent history of intermittent low-grade bilateral flank pain. She had no history of any medical illness and family history was not significant. Physical examination findings were normal. Her blood pressure was 160/90 mm Hg. Urinalysis results were normal. Laboratory analysis revealed normal renal function. Ultrasonography revealed bilateral perirenal and parapelvic septate collections with increased echo texture and enlarged kidneys. Subsequent CT scan of abdomen showed per pelvic collections of various densities with indentationon renal capsule. Collecting systemis splayed without dilatation. Excretory phase had normal excretion of contrast without any extravasation, ruling out any communication with pelvicalyceal system. Analysis of USG-guided aspirated fluid showed few lymphocytes with abundant protein and high levels of renin. No organism was isolated from aspirated fluid. A diagnosis of bilateral renal lymphangiectasia was made. Patient was treated with angiotensin-converting enzyme (ACE) inhibitors, 50 mg of Diclofenac SOS, and salt restriction. On follow-up, her blood pressure came down to 130/80 mm Hg. She was advised for long-term follow-up. Pain gradually subsided without any surgical intervention (Figures 1-4).
3. Discussion
Renal lymphangiectasia is an uncommon benign condition associated with disturbances in lymphatic drainage of perirenal and hilar areas causing cystic dilatation of perirenal and peripelvic lymphatics (6, 7). Although the exact pathophysiology is unclear, both developmental malformation and acquired obstructive inflammatory causes has been suggested. Familial association has been also found in a few cases. Clinical manifestation is non-specific. Patients might present with flank pain, abdominal mass, lower extremity edema, gross hematuria, ascites, or hypertension (7). Renal function is usually well preserved. The cause of hypertension is presumed to be compression of renal parenchyma by the subcapsular collection resulting in excessive renin release. Differential diagnosis of this condition includes polycystic kidney disease, multicystic dysplastic kidneys, multilocular cystic nephroma, and urinoma depending upon clinical presentation. Diagnosis can be made on the basis of characteristic findings on USG, CT-scan, and MRI. Needle aspiration of chylous fluid from the perinephric fluid collections confirms the diagnosis.
Asymptomatic cases do not require treatment. Percutaneous aspiration of perinephric collection has been done to relieve pain not responding to analgesics (8). Marsupialization has been also reported to make communication with peritoneal cavity to drain fluid (9). Hypertension is controlled with ACE inhibitors. A diuretic is used to control the ascites. Rarely, renal lymphangiectasia is associated with renal vein thrombosis and needs nephrectomy (10).