1. Background
Occult Hepatitis B virus (HBV) infection (OBI) is defined as the presence of HBV-DNA in the liver or serum with undetectable hepatitis B surface antigen (HBsAg) with or without HBV antibodies (1). Serum HBV-DNA level should be less than 200 IU/mL. A serum level greater than 200 IU/mL is interpreted as an infection caused by escape mutants, not an OBI (2). While the exact mechanism of OBI is unclear, several explanations have been proposed. One probable theory is genetic variations in the S region of the HBV genome, which inhibit HBsAg production and viral replication. Different studies showed numerous mutations in the HBV genome of OBI patients. However, biological significance of these mutations is still unclear (3-5). In some cases, these mutants are characterized by a glycine to arginine mutation at residue 145 (G145R) within the "a" determinant region of the HBV S region (6). OBI patients are at risk of progression to liver disease, transmitting infection to others through dialysis, blood transfusion and organ transplantation or early death as a result of disease complications such as acute exacerbation of chronic hepatitis B, fulminant hepatitis and development of hepatocellular carcinoma (7, 8). Hemodialysis (HD) patients are at risk of acquiring parenterally transmitted infections such as HBV, because of the large number of received blood transfusions, invasive procedures they undergo, shared dialysis equipment, impaired host immune response and lower response rates to HBV vaccination (3, 9). OBI patients were classified as seronegative (both hepatitis B surface antibody (anti-HBs) and hepatitis B core antibody (anti-HBc) have negative results) and seropositive (anti-HBc has a positive finding with or without anti-HBs positivity) (10). Occult HBV infection is most frequently seen in patients with anti-HBc as the only HBV serological marker (isolated anti-HBc) (11, 12) and the HBV-DNA detection rate is highest in subjects who are anti-HBc positive but anti-HBs negative (7). Therefore, isolated anti-HBc can be considered as a sentinel marker of occult HBV infection (12, 13). Iran is a low endemic area of HBV infection (14). A nation-wide study in Iran showed the prevalence of HBsAg as 1.7%, ranging from 0 to 3.9% in different provinces (15). In a study by Eslamifar et al. 6.49% of Iranian HD patients had HBV infection (16). In another study by Rostami et al. prevalence of HBsAg among Iranian HD cases decreased from 2.6% in 2006 to 2.1% in 2011 (17). In two studies on the rate of OBI in healthy blood donors in Iran, OBI was detected in 12.2% and 0% of anti-HBc-positive subjects (18, 19)
2. Objectives
We previously conducted a study in hemodialysis patients with isolated anti-HBc and OBI was detected in 50% of these patients (20). Nevertheless, according to the above explanation, we decided to perform another investigation to determine the prevalence of OBI among all HBsAg negative HD patients. Besides, we evaluated mutations in the S region of the HBV genome in OBI cases.
3. Patients and Methods
In this cross-sectional study, 100 HBsAg negative HD patients were consecutively recruited from a main dialysis unit in Tehran, Iran from January 2013 to January 2014. A questionnaire was used to collect epidemiologic and clinical data such as age, gender, duration on dialysis and previous medical history. This project was approved by the Pasteur Institute of Iran ethics committee (No: 615) and informed consent was obtained from all patients. Dialysis unit monitored patients regarding viral infections at the time of admission and every three months. Blood samples were collected before dialysis, in the dialysis day and plasmas were stored at -80°C. All samples were tested for HBsAg, anti-HBs and anti-HBc by enzyme-linked immunosorbent assay (ELISA). The commercial enzyme immunoassay kits used were as follows: HBsAg and anti-HBs (Hepanostika Biomerieux, Boxtel, The Netherlands) and anti-HBc (Dia. Pro Diagnostic Bio Probes, Milan, Italy). Liver enzymes [Alanine aminotransferase (ALT) and Aspartate aminotransferase (AST)] were determined in all patients. All assay protocols, cutoffs and result interpretations were performed according to the manufacturers’ instructions. HBV-DNA was extracted using High Pure Viral Nucleic Acid kit (Roche Diagnostics GmbH, Mannheim, Germany) according to the manufacturer’s instructions. HBV-DNA was determined by real-time PCR using
HBV Real time PCR (Genome Diagnostics, New Delhi, India) on the Rotor-Gene 6000 real-time thermal cycler (Corbett Research, Sydney, Australia). The detection limit of the kit was 100 IU/mL according to the user manual.
3.1. Amplification of HBV S-ORF and Sequencing Assay
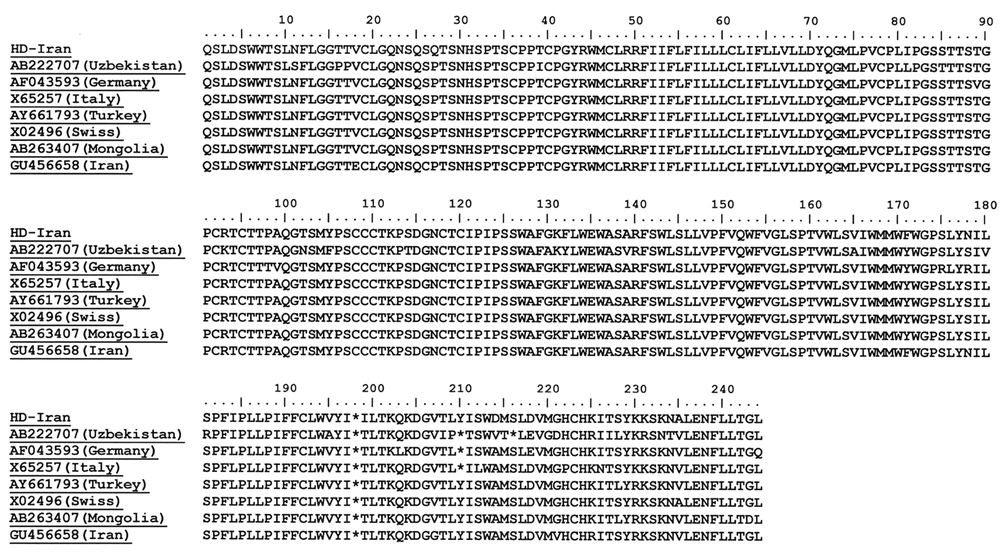
The most conserved regions of S gene sequences were amplified by nested PCR, using the primers S1A (5-GTTCAGGAACAGTAAGCCC-3) and antisense (5-GAAAGGCCTTGTAAGTTGGCG-3). Nested PCR was performed to increase the sensitivity of detection and to provide an amplicon (730 bp) for sequence analysis using the primers sense (5_GGTGGACTTCTCTCAATTTTCTAGG-3_) and S2 (5-ACTTTCCAATCAATAGGCC-3) (21). A 10-μL of extracted DNA was added to an amplification mixture containing 5 μL of 10× PCR buffer, 1.5 μL of MgCl2 (50 mM), 1 μL of dNTP mix (100 mM each), 1 μL (2.5 U) of Taq polymerase (CinnaGen, Tehran, Iran) and 2 μL of each of outer primers (10 pmoL) witha total volume of 50 μL. The PCR profile was an initial three-minute denaturation at 94°C, followed by 35 cycles of amplification including denaturation for 30 seconds at 94°C, annealing for 30 seconds at 56°C and extension for 40 seconds at 72°C. Strand synthesis was completed at 72°C for 6 minutes. A 2-μL of the first-round PCR products was subjected for the second-round PCR under the same conditions, but annealing temperature of 50ºC. Second-round PCR products were subjected for bidirectional automated sequencing using both forward and reveres inner primers (Pasteur Institute of Iran, Tehran, Iran). Nucleotide sequences were aligned with CLUSTALW program using BioEdit software (BioEdit Sequence Alignment Editor Software, Department of Microbiology, North California State University). Variants were compared with original sequences of this genotype to identify mutations. Nucleotide sequences of HBV isolate reported in this article can be found in the GenBank database under the accession number of KC344385.
3.2. Statistical Analysis
Chi-square and t2-tests were used by SPSS 16 Package software for statistical analysis (Chicago, IL, USA). Clinical and demographic variables were presented as median (IQR) and categorical variables were demonstrated as absolute number and percentage.
4. Results
A hundred HBsAg negative HD patients with a median age of 60 (IQR: 45-70) years were enrolled in this study. Fifty-seven percent of patients were male and 43% female. All patients had a history of HBV vaccination according to the standardized vaccination schedule, 40 μg of the recombinant HBV vaccine (Pasteur Institute of Iran, Tehran, Iran) at 0, 1, 2 and 6 months. The duration of HD was 3 (IQR: 1-6) years. In total, 54% of cases had a history of blood transfusion approximately every three months and none of them had organ transplantation. The median of ALT and AST levels were 17 (IQR: 13-24) and 17 (IQR: 13-23) IU/L, respectively. None of patients had a history of previous liver disease. Anti-HBs and anti-HBc were found in 57% and 2% of patients, respectively. Isolated anti-HBc (HBsAg negative, anti-HBs negative and anti-HBc positive) was detected in two (2%) patients. HBV-DNA was detected in one (1%) of HBsAg negative HD cases. This patient was a 57-year-old female with a history of HD from five years ago. She had a history of blood transfusion every six months and had hypertension. She had positive results foranti-HBc and anti-HBs and negative foranti-HCV and anti-HIV. She had normal levels of ALT and AST. In this patient, genotype of HBV and surface gene mutations were analyzed. In this patient, genotype of HBV and surface gene mutations were analyzed. The phylogenetic analysis showed that this isolate was clustered in the genotype D, sub genotype D1 and subtype ayw2. No “a” region mutation was found. The most common amino acid substitutions found in this isolate were P56Q, L213I and T228I. Positions of amino acid substitutions found in this isolate were shown in Figure 1.
5. Discussion
Detection of HBV-DNA in the absence of HBsAg, regardless of presence of other HBV serological markers (anti-HBc and/or anti-HBs) is defined as occult HBV infection (21, 22). In general, about 20% of OBI individuals have negative results for all HBV serological markers (seronegative group), and 80% have positive results for serological markers of previous infection with HBV (seropositive group) (20). In total, 35% of OBI patients have positive results for anti-HBs and 42% of them show anti-HBc positivity (24). HBV-DNA detection rate is higher in individuals with positive results for anti-HBc, but negative for anti-HBs (13). The prevalence of occult HBV infection is variable in different populations and parallel with the general prevalence of HBV infection in that region (8, 23). Prevalence of OBI can be affected by sensitivity and specificity of HBV-DNA detection methods (24). The prevalence of occult HBV infection in dialysis patients ranged from 0% to 58% in different surveys (25-31). Cabrerizo et al. (27) showed that occult HBV infection was found in 57.6% of HD patients, but Dueymes et al. (31) reported this rate as 13.9% and Fabrizi et al. (28) demonstrated no OBI in a large cohort of Italian chronic dialysis patients. It can be due to differences in the composition of study populations, diverse prevalence of HBV infection in different countries and within different dialysis units and the level of sensitivity of the HBV-DNA assay (20). Iran is in a low endemic area of HBV infection. The prevalence of HBsAg in Iran was reported 1.7%, ranging from 0% to 3.9% in different provinces (15). Improvement of people’s knowledge about risk factors of HBV transmission and national vaccination program decrease HBV incidence in the general population and hemodialysis patients (14). The prevalence of HBsAg in HD patients decreased from 4.3% in 2002 to 2.8% in 2008 and 2.1% in 2011 (17, 32). In our previous study in hemodialysis patients in Tehran, 6.2% of them had isolated anti-HBc and OBI was detected in 50% of HD patients with isolated anti-HBc (20). In the current study after about three years, patients had a lower rate of isolated anti-HBc (2%) and OBI was observed in 1% of HBsAg negative HD patients. It can be due to HBV vaccination of HD patients, regular surveillance of HBV infection and employment of appropriate anti-infective universal precautions, which all together reduce the spread of HBV in the dialysis population. Besides, isolated anti-HBc is an important marker for occult HBV infection and the HBV-DNA detection rate is highest in these subjects, so this serologic condition can reflect occult HBV infection in high-risk groups (12). Therefore, another cause for lower rate of OBI in this study can be attributed to lower rate of isolated anti-HBc in our dialysis patients and determination of the prevalence of OBI among all HBsAg negative HD patients, not only patients with isolated anti-HBc. Mutations in the HBV surface gene have been reported in a variety of OBI cases. Many of these mutations affect the amino acid sequence of the antigenic “a” region of the S gene (3, 4, 6). The result of genotyping this isolate was in agreement with previous reports on genotype/subtype distribution in different regions of Iran (33, 34). No “a” determinant mutations were detected, but several substitutions were identified. Because only one isolate was detected, definitive conclusions cannot be made in this case. In conclusion, this study showed decreased rate of isolated anti-HBc and occult HBV infection in HD patients. It can be due to improvement of people’s knowledge about HBV transmission routes, HBV vaccination of HD patients and regular surveillance of HBV infection, all together reduce HBV spread in dialysis patients. A limitation of our study was its relatively small sample size. Therefore, our results cannot be generalized to all dialysis centers and further studies are needed regarding this issue. However, we suggest performing abovementioned conditions in all dialysis centers to decrease the rate of occult HBV infection in HD patients.