1. Introduction
Leiomyosarcoma is a malignant soft tissue tumor that can arise from any tissue containing smooth muscle. Leiomyosarcomas arising in paratesticular tissues are extremely rare and approximately 10% of all paratesticular sarcomas are leiomyosarcomas (1). Primary paratesticular tumors constitute 7% to 10% of all intrascrotal tumors (2). Generally these tumors present as asymptomatic, firm, palpable, and slow-growing paratesticular masses (3). These type of lesions are reported in all age groups, but are mostly diagnosed in the sixth and seventh decade of life (4). Radical inguinal orchiectomy and high ligation of the cord is the standard primary surgical procedure (3-6).
2. Case Presentation
A 75-year-old man presented with a history of painless lump in the right hemiscrotum. He had sensation of heaviness in right hemiscrotum. He had no history of trauma, previous hospitalization, specific drug use, or familial disease. Clinical examination findings were normal and no pathologic finding was observed in chest X-ray. Abdominal examination showed no palpable masses or ascites. Local examination of scrotum and inguinal showed a diffused enlargement of right hemiscrotum. The spermatic cord was thick and hard. Tumor markers level such as α-fetoprotein, LDH, and β-human chorionic gonadotropin were within normal limits. The findings of routine blood investigations were normal and there were no specific findings in urinary test. The patient was candidate for right testicular orchiectomy. Upon operating, we discovered a hard tumoral lesion in spermatic cord. The resected specimen of testis, measuring approximately (4 × 3 × 3 cm), had no pathologic changes. A nodular tumor lesion with 9.5-cm length and 4-cm diameter was observed in the spermatic cord. It had monotonous gray-white appearance with no evidence of bleeding or necrosis.
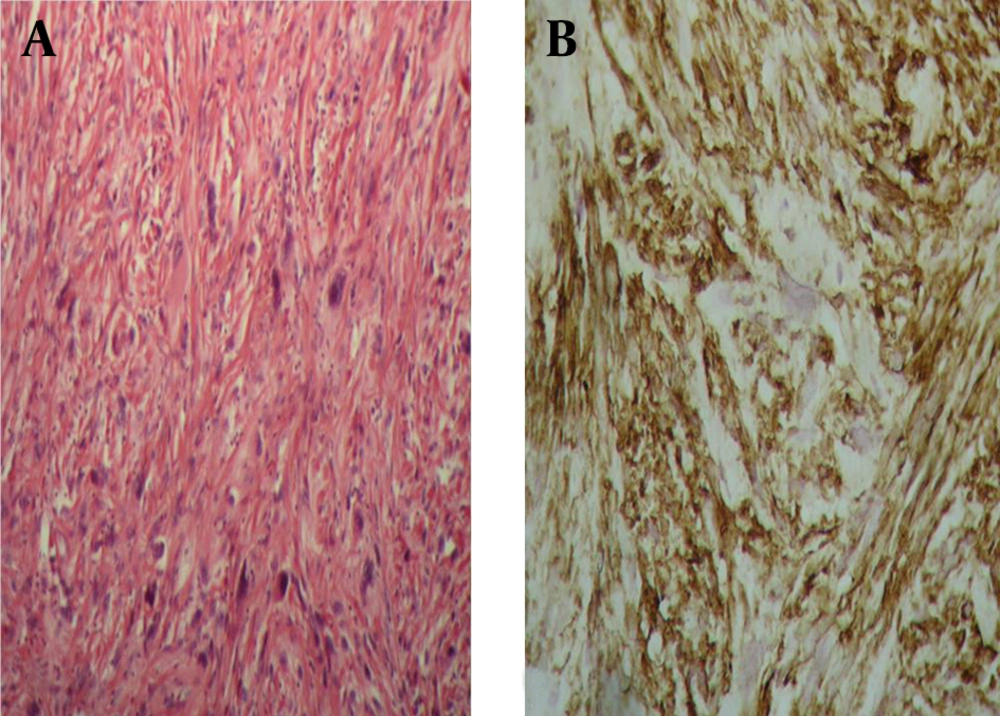
Histopathologic findings showed a neoplastic tissue with mesenchymal origin, which had arisen from smooth muscle cells. Microscopic examination revealed a highly cellular lesion composed of spindle cells with vesicular chromatin. Pleomorphic nuclei were arranged in condensed cellular groups. Neoplastic multinucleated giant cells with bizarre shape were encountered in different areas with two to three mitoses per high power Field (2-3/HPF). Alpha-smooth muscle actin (α-SMA) marker was positive in neoplastic cells. These pathologic features confirmed a leiomyosarcoma of the spermatic cord.
3. Discussion
Leiomyosarcoma constitute 5% to 10% of soft tissue sarcoma. Paratesticular leiomyosarcomas are rare malignant neoplasms originating from scrotum, spermatic cord, or epididymis (7, 8). Leiomyosarcomas of the spermatic cord are uncommon tumors of non-testicular origin, which drain into the retroperitoneal lymph nodes, and have been reported in less than 150 cases in the literature until now (9). This type of leiomyosarcoma arises from undifferentiated mesenchymal cells of the cremasteric muscle and vas deferens. Although this type of lesion is seen in all age groups, peak incidence of spermatic cord leiomyosarcoma is in the sixth and seventh decades of life. Preoperative diagnosis of spermatic cord type is difficult and is commonly made by histopathologic examination and immunochemical staining (7-10). The standard treatment for all types of non-testicular leiomyosarcomas is radical orchiectomy. Our patient had grade 1 spermatic cord leiomyosarcomas. The prognosis after radical orchiectomy is usually good in tumors of grade 1 and 2 (9, 11).
In summary, leiomyosarcoma of the spermatic cord are rare malignant tumors, which are treated with radical orchiectomy, and clinicians should notice them in differential diagnosis of a firm and hard solid mass in the cord. However, a large number of spermatic cord leiomyosarcoma are low-grade hard tumor with good prognosis, long-term follow-up is needed to prevent recurrence and metastasis.