1. Background
Impotence and ejaculation disorders are the most common sexual diseases in men. Sexual dysfunction tends to increase with age and is more common among elderly patients with comorbidities such as cardiovascular disease and diabetes mellitus (1). Probably imbalance between testosterone and serotonin plays a role in PE. PE may affect men of all age groups and does not usually occur with other diseases (2, 3). In a survey that uses the premature ejaculation diagnostic tool (PEDT), the prevalence of premature ejaculation was up to 40% in men aged 40 - 70 years, and usually correlated with erectile dysfunction (ED) (4-6). It may be primary or acquired but can cause a considerable negative effect on sexual relationships and decrease sexual partners’ quality of life. Behavioral therapy and/or several medications that are conventionally used for PE may be helpful in extending the ejaculatory latency time by some degrees (7).
No clear accepted definition of PE has been established, and this allows us usually to accept a patient-dependent definition or patient-decided diagnosis. This is why multiple definitions are used today for PE, while simple and reliable criteria are needed to evaluate the results of treatment for such patients (8). In the present study, patient-reported outcome measures are used to diagnose and evaluate conditions such as ED and erection hardness score, for which physiological measures are not readily available (9). For these reasons, any form of PE definition by the patients will be the main source of information about the condition.
At present, the only valid criteria of PE are the measures stated in the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) (10). The DSM-IV-TR definitions of PE include “shortly with minimal sexual contact or just after vaginal intromission,” as an ELT criteria, and “causes marked distress and interpersonal sexual difficulty” as a measure for the negative psychological outcomes of PE (11).
PE is often defined in terms of intravaginal ejaculatory latency time (IELT) in clinical researches, which is the time between the start of vaginal intromission and the start of intravaginal ejaculation (12). IELT is an important criteria suggested for evaluation of treatment outcomes, but using this measure alone will not accurately characterize PE. PE may also be defined based on partner satisfaction and/or the orgasm quality of both partners, so IELT alone does not consider all aspects of PE (13, 14).
PE could be primary (lifelong) or secondary (acquired). Primary PE begins when a male first becomes sexually active (i.e., post puberty) (15). Most secondary premature ejaculations can be associated with some known acquired causes such as physical, pharmacological, and psychological factors. However, in rare cases, hyperexcitability might relate to men with lower than normal age-matched levels of circulating testosterone that well responds to testosterone normalization with the administration of hormonal and psychotropic drugs. It is also related to organic diseases such as clinical varicoceles and chronic prostatitis that resolves when these pathologies are improved or drugs are withdrawn (16-21). Most secondary cases of PEs are idiopathic premature ejaculation because of their unknown etiology, although psychological conditions or different value threshold responses to androgenic hormones are suggested in most of them. Idiopathic PE necessitates more attention because of intractability and persistent disease that could cause psychological outcomes.
Among the common medications mostly prescribed for idiopathic PE patients are selective serotonin reuptake inhibitors (SSRIs), which have known effects of postponing ejaculation and improving premature orgasm (19, 21). SSRIs sometimes may cause sexual dysfunction, especially in long-term uses as in cases of depression (reported with various rates), ranging from small percentages to more than 80%, as in cases of use for inhibited orgasm (4% - 10%), ED (4% - 10%), premature ejaculation (35%). They may also have harmful effects on semen parameters (20, 22).
Recent studies have shown the critical role of androgens in regulating the sexual behavior in human males and different sexual behavior responses to different androgenic hormone levels, suggesting the necessity for evaluation of the precise role of sexual hormones in male sexual habits (23, 24).
Clomiphene citrate, which has an anti-estrogenic property, can produce higher free testosterone levels that could reverse the functional suppression of the central hypothalamic-pituitary axis (25). In addition, clomiphene provides better sexual function for younger men with fewer medical risk factors and with lower than normal age-matched levels of testosterone by normalization of free testosterone level (26). Taylor and Levine (2010) compared between treatment with testosterone replacement and treatment with clomiphene for hypogonadal men. Their study showed better effects of clomiphene after 4 months, with fewer side effects and lower cost than testosterone gel replacement therapy (19).
2. Objectives
In this case-control study, we assessed and compared between the effect of clomiphene and that of placebo as treatment for challenged idiopathic PE patients.
3. Patients and Methods
Among 178 married men who presented to a men’s health program, aged 24 - 57 years with idiopathic PE (without any known etiologies), 126 (70.78%) completed the course of study. Premature ejaculation was defined according to the DSM-IV. None of the patients had a prior history of psychiatric problems such as depression and anxiety. The luteinizing hormone (LH), follicle-stimulating hormone (FSH), thyroid-stimulating hormone (TSH), prolactin, and the total and free testosterone levels were assayed before and after the intervention. Blood samples were obtained early in the morning (8:00 - 10:00 AM), at the first visit.
The subjects were randomized into 2 groups by using computer-generated random numbers and assigned to receive clomiphene 50 mg/day (group 1 = 62) or placebo orally (group 2 = 64).
All couples had been recommended to record the number of sexual attempts, successes at intercourse, and about PE in a questionnaire. The satisfaction of their partners in more than 75% of attempts was considered successful complete intercourse, and that in from 50% to 75% of attempts was considered as partial success.
None of the participants reported any side effect by clomiphene citrate during the study course. For both groups of patients, LH, FSH, prolactin, and total and free testosterone levels were evaluated, and the patients were prospectively followed up for 12 weeks. The questionnaires (International Index of Erectile Function [IIEF], PHS penile hardness score (PHS), IELT, and QOL) were completed before and after therapy. Collected data were compared before and after the therapies, between the two groups, and within each group.
Statistical analysis was conducted by using the SPSS Version 18 statistical software for Windows, using the paired t test and one-way analysis of variance. Significant differences between the appropriated groups were considered when P was < 0.05.
4. Results
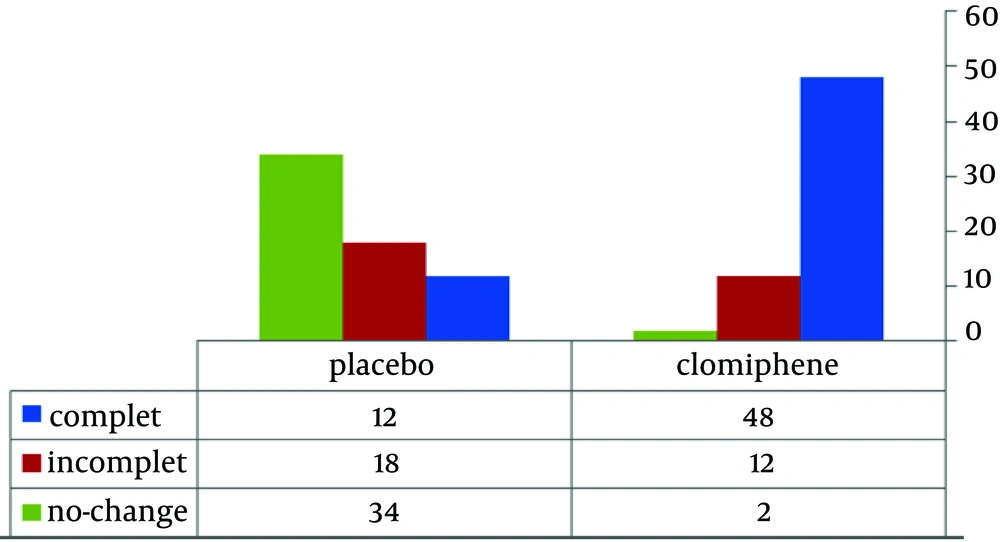
The mean age of the patients who completed the study (126 = 54.78%) was 52.5 ± 6.2 years. Figure 1 shows the comparison of the response rates to treatment of PE in groups 1 and 2. The complete response rates with a regular intercourse were 77.41% and 18.75%, the partial response rates were 19.35% and 28.12%, and no change was observed in 3.22% and 53.12% in groups 1 and 2, respectively.
The results of this study showed that serum LH, FSH, prolactin, and total-testosterone levels in both groups were unchanged after therapy. However, the plasma free testosterone level, which is an indicator of available circulating androgen activity, in the clomiphene group was higher than that in the placebo group (78.7 ± 12.2 vs. 30 ± 18.4 nmol/L, P < 0.05). Tables 1 and 2 show sexual function indexes and QOL before and after therapy in both groups. IELT, the main outcome of this study, was significantly improved in the study group (P < 0.01). The other data such as the sexual indexes and QOL were better in the clomiphene group than in the placebo group (Table 3).
a Not significant.
b QOL: Quality of life.
5. Discussion
This study evaluated the efficacy of clomiphene on the treatment of idiopathic PE. Currently, the etiologies of PE are not well understood; but according to possible causes, some traditional treatments for physiological premature ejaculation have been recommended, such as pharmacological management with paroxetine, sertraline, clomipramine, dapoxetine, and local lidocaine cream. Some physical maneuvers are also recommended, such as the squeeze technique, and mental distraction, with varied success rates. The treatment of premature ejaculation was changed dramatically after the introduction of selective serotonin reuptake inhibitors (SSRIs), as the American Urological Association considered SSRIs as first-line systemic therapy for PE (27). In 1994, paroxetine was the first SSRI to be used for PE (28). From that time onward, most SSRIs such as clomipramine and fluoxetine are used in the treatment of ejaculation delay. Recently, dapoxetine was considered as the first prescription treatment of PE and strongly suggested for use in younger men with primary PE. Dapoxetine is the latest and most effective SSRI. It is structurally similar to fluoxetine, so naturally, being an SSRI, it will have some drawbacks related to the nature of SSRIs. In particular, it induces or worsens existing ED, for which most researchers usually recommend the use of phosphodiesterase type 5 inhibitors in combination with this drug in PE patients (6, 29, 30).
However, patients who have taken SSRIs for various reasons may experience acute and long-term side effects other than decreased sex drive, dry mouth, nausea, headache, diarrhea, anxiety, restlessness, sweating, weight gain, sleepiness, or fatigue, which sometimes cause treatment discontinuation (31).
PE, unlike ED, is not age related and is prevalent in all ages. However, when it is observed in comparison with ED, especially in older objects, there may be hormonal imbalances such as hypogonadism or hypothalamic-pituitary-gonad axis abnormalities. Our study showed that most idiopathic PE patients had subclinical ED, as the responses to the questionnaires revealed that ED was not their main complaint). After treatment with clomiphene, their free testosterone levels were improved significantly. Besides the improvement in PE, ED also improved in terms of the abnormal indexes. However, androgen deficiency symptoms were reported despite normal testosterone levels, chiefly in aging males. In aging males, androgen deficiency symptoms may be reported under normal testosterone levels and symptom-specific testosterone thresholds may change. Thus, under these conditions, aging may be an important confounder of these factors (32).
In the presence of all hypogonadisms, psychotic statuses such as anxiety and depression are well known to have high prevalence rates and to cause related sexual disorders such as ED and PE. Treatment of these hypogonadal patients by using hormonal replacement would improve their sexual statuses (33, 34).
Therefore, in this study, in order to find an appropriate and new drug with fewer side effects in the treatment of idiopathic PE, we assessed the efficacy of clomiphene in comparison with that of placebo. We demonstrated that clomiphene, via the regulation of hormonal profiles and, probably, the subsidence of anxiety owing to the improvement of free testosterone levels, improved the ED indexes, PE, and QOL in the idiopathic PE patients.
Clomiphene citrate, a selective estrogen receptor modulator that by inhibiting negative feedback on the hypothalamus, increases the production of pituitary hormones and enhances the natural production of testosterone (18). It is not a biologically identical agent, so the adverse drug reactions associated with it, such as vasomotor symptoms (commonly called “hot flashes”), abdominal discomfort, visual symptoms (blurring), and/or reversible ovarian pathology in females (cyst formation and hypertrophy), are rare (≤ 1% of cases) and usually are minor and dose dependent (9, 18).
Clomiphene citrate also has been found to be highly effective in the treatment of central or secondary male hypogonadism in recent reports (35-37). According to these reports, premature ejaculation may be associated with hypogonadism, and PE may be the first presentation of hypogonadism. Finally, ED and ejaculatory dysfunctions frequently overlap. In some studies were considered ED as an important risk factor of PE and vice versa. For this reason, clomiphene therapy for such cases is preferred to other medical treatment options such as testosterone replacement therapy or psychotherapy (37-39). Clomiphene appears to be a useful agent in the pharmacological treatment of idiopathic premature ejaculation compared with the patients receiving placebo.