1. Background
Bladder cancer is the second most frequent cancer of the genitourinary system, the fourth most common cancer in men, and the seventh most common of all (1). Hematuria is the most prevalent symptom that occurs in 80% - 90% of cases and is usually presented without other urinary symptoms (called painless hematuria) (2). After diagnosis, the disease is treated with surgery, chemotherapy, or radiotherapy based on the patient’s particular condition, but recurrence is very common (3-5). Many drugs have been used in recent decades to lower the recurrence rate, such as bacillus Calmette-Guerin (BCG), mitomycin C, doxorubicin, and thiotepa.
About forty years ago, Heuson indicated that there is a relationship between diabetes mellitus (DM) and cancer (6), and other investigators claimed that disorders of intracellular signaling pathways, insulin resistance, and treatment with anti-diabetic drugs can affect cancer incidence and progression (7-10). One such drug is metformin. Metformin is a semi-synthetic agent that is derived from galegine and is administered to lower blood sugar. Today, this drug is used for the treatment of diabetes mellitus and the prevention of cardio-vascular disease and polycystic ovarian syndrome (PCOS) (11, 12).
Preliminary evidence shows that metformin can lower the incidence rate of some cancers (including those of the breast, colon, liver, lung, prostate, and pancreas) in type 2 diabetic patients (13-15). Metformin activates protein kinases and decreases rapamycin signaling (mTOR) which can then lower blood sugar (16). Based on current evidence, cancer cell growth in bladder cancer requires activation of mTOR (17, 18), so it seems that inhibition of this pathway could be an effective way to treat or prevent bladder cancer.
2. Objectives
This study was designed for the assessment of metformin usage in the prevention of bladder cancer recurrence after the trans-urethral resection of a bladder tumor (TUR-T).
3. Patients and Methods
3.1. Patient Selection and Data Collection
From April 2013 to September 2014, all patients referred to Baqiyatallah hospital with the diagnosis of a bladder tumor who underwent TUR-T were included in this study. There were 65 patients and they were divided into two groups: group 1 included 32 patients who were administered metformin as part of their treatment plan, and group 2 included 33 patients who did not take the drug. Patients with hepatic dysfunction and a history of chemotherapy or radiation were excluded. Data on sex, age, history of smoking, diagnosis of DM, size and number of tumors, histology of tumor cells, and grade and stage of resected tumors were collected before surgery.
3.2. Metformin Administration
Metformin was administered in doses of 1000 mg per day (2 doses 500 mg) for the 32 patients in group 1.
3.3. Follow Up
All patients were followed up with ultrasonography and cystoscopy every 3 months for a 1 year period.
3.4. Statistics
For analyzing the data, SPSS software version 20 was employed. Then, a chi-square test and Spearman’s rank correlation coefficient were used to determine qualitative parameters, and an independent t-test was used for assessing the quantitative parameters. In all tests, a P value of less than 0.05 was considered significant.
4. Results
4.1. Demographic and Past Medical History
Group 1 (metformin) included 32 patients with an age range between 46 and 91 years and a mean age of 63.44 ± 11.71 years. In this group, 11 patients were female (34.4%) and 21 were male (65.6%). Group 2 (control) included 33 patients with an age range between 23 - 83 years and a mean age of 62.06 ± 14.88 years. Of these patients, 8 were female (24.2%) and 25 were male (75.8%).
Other demographic characteristics are shown in Table 1. According to this it it is evident that smoking, DM, previous surgery on the genitourinary tracts, tumor histology, and stage and grade were not statistically different between the 2 groups, but the tumor pedicle type (papillary or sessile) was statistically different (P value < 0.05).
| Group 1 | Group 2 | P Value | |||
|---|---|---|---|---|---|
| Female | Male | Female | Male | ||
| Smoking | 0.148 | ||||
| + | 0 | 9 (43) | 1 (13) | 14 (56) | |
| - | 11 (100) | 12 (57) | 7 (87) | 11 (44) | |
| DM | 0.423 | ||||
| + | 2 (18) | 3 (14) | 2 (25) | 1 (4) | |
| - | 9 (82) | 14 (86) | 6 (75) | 24 (96) | |
| Previous surgery | 0.857 | ||||
| + | 6 (55) | 4 (19) | 2 (25) | 9 (36) | |
| - | 5 (45) | 17 (81) | 6 (75) | 16 (64) | |
| Number of tumors | 0.138 | ||||
| Single | 9 (82) | 15 (71) | 7 (87) | 12 (48) | |
| Multiple | 2 (18) | 6 (29) | 1 (13) | 13 (52) | |
| Pedicle | 0.016 | ||||
| Papillary | 9 (82) | 9 (43) | 7 (87) | 20 (80) | |
| Sessile | 1 (9) | 9 (43) | 1 (13) | 3 (12) | |
| Both | 1 (9) | 3 (14) | 0 (0) | 2 (8) | |
| Stage | 0.810 | ||||
| T1 | 6 (55) | 9 (43) | 6 (75) | 12 (48) | |
| T2 | 1 (9) | 9 (43%) | 0 (0) | 8 (32) | |
| Ta | 4 (36) | 1 (5%) | 2 (25) | 2 (8) | |
| CIS | 0 | 0 | 0 | 1 (4) | |
| Undefined | 0 | 2 (9) | 0 | 2 (8) | |
| Grade | 0.803 | ||||
| Low | 8 (73) | 9 (43) | 5 (62) | 14 (56) | |
| High | 1 (9) | 9 (43) | 2 (25) | 8 (32) | |
| PUNLMP | 2 (18) | 1 (5) | 1 (13) | 1 (4) | |
| Chronic cystitis | 0 | 0 | 0 | 1 (4) | |
| Undefined | 0 | 2 (9) | 0 | 1 (4) | |
aValues are expressed as No. (%).
None of patients showed any side effects of metformin use, including abdominal or stomach discomfort, cough or hoarseness, decreased appetite, diarrhea, fast or shallow breathing, fever or chills, general feeling of discomfort, lower back or side pain, muscle pain or cramping, painful or difficult urination, or drowsiness.
4.2. Tumor Size
In group 1, the tumor size was between 0.5 - 5 cm with a mean size of 1.90 ± 1.13, and in group 2, it was 0.5 - 11 cm with a mean of 2.14 ± 1.79. There was no statistical differences between the 2 groups (P value = 0.535).
4.3. Tumor Recurrence
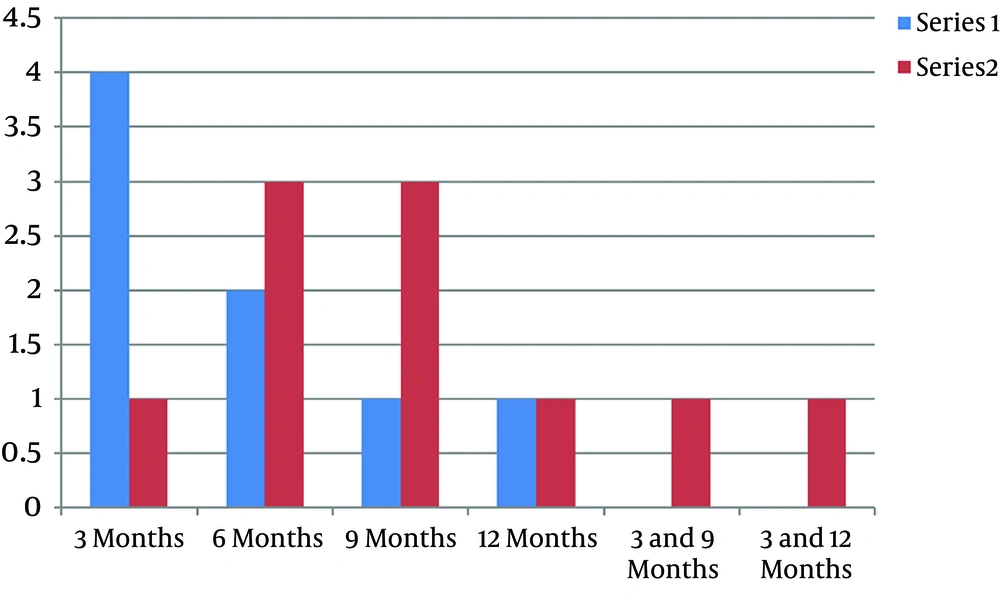
It was revealed that 8 (25%) patients in group 1 and 10 (30.3%) in group 2 had tumor recurrences during the 1 year follow-up period, and this rate is not statistically different (P value = 0.633). The time of recurrence (as shown in Figure 1) is longer in group 1 but the prevalence of the recurrence time is not different (P value = 0.5430).
The results of a correlation test between recurrence and demographic characteristics are shown in Table 2. There was no correlation between sex, DM, and tumor grade with tumor recurrence, but age and tumor size had a weak positive correlation with recurrence in group 1, and a weak negative correlation with recurrence in group 2. However, neither of these correlations were statistically significant (P value > 0.05).
| Sex | Age | Smoking | DM | Tumor Grade | Tumor Stage | Tumor Size | |
|---|---|---|---|---|---|---|---|
| Group 1 | |||||||
| Correlation | 0.190 | 0.231 | -0.040 | -0.050 | -0.121 | -0.017 | 0.275 |
| P Value | 0.298 | 0.204 | 0.827 | 0.287 | 0.510 | 0.927 | 0.127 |
| Group 2 | |||||||
| Correlation | 0.089 | -0.288 | -0.205 | 0.021 | 0.094 | 0.275 | -0.336 |
| P Value | 0.624 | 0.104 | 0.253 | 0.908 | 0.603 | 0.122 | 0.056 |
5. Discussion
To our knowledge, the present study is the first one to evaluate the efficacy of metformin on bladder tumor recurrence after TUR-T. Our results show that metformin cannot reduce bladder tumor recurrence, but it can prolong the time to recurrence, although such intervals are not statistically significant. This result is in contrast to those of many other studies (13, 19-22).
Currie in 2009 claimed that in diabetic patients using insulin and metformin, the incidence of colorectal and pancreatic cancer was lower than the corresponding rates among the normal population (13). In similar studies, the survival rates of diabetic patients who were treated for colorectal or pancreatic cancer were 30% higher than those of diabetic patients who received other anti-diabetic agents (19-21). Furthermore, Wright and colleagues found in their study on Caucasian men that metformin can reduce the risk of prostate cancer by up to 44% (22). This discrepancy between our results and other studies may be due to our small sample size or the relatively short time of metformin administration and follow up (13, 19-22).
In 2010, Patel studied diabetic patients who had undergone radical prostatectomy and claimed that there is no association between metformin usage and the recurrence of prostate cancer; indeed, the recurrence rate was 55% higher in diabetic patients (23). These differences in the results may be due to the various risk factors that can affect incidence, progression, and recurrence of cancers, such as age, sex, obesity, smoking, genetics, and the environment. For example, it has been shown that smoking can increase the risk of developing bladder cancers by 3.89% and 4.65% in men and women, respectively (24), but this correlation was not shown in our study.
The precise effects of metformin on cancer are unclear, but some suggestions include the following: (1) it might stop the mTOR signaling pathway through AMP-activated protein kinase (AMPK) (25-27); and (2) it might decrease the insulin level by way of reducing the insulin-like growth factor-1 (IGF-1) (26, 28). Furthermore, it is clear that metformin can increase poly (ADP-ribose) polymerase (PARP)-dependent cell death and caspase-dependent apoptosis in breast cancer. Metformin has also been shown to decrease the activity and expression of HER2 in cancer cells, which is dose dependent and can be seen in higher administered doses of metformin (29-31). This may be the cause of the ineffectiveness of metformin in our study.
5.1. Conclusions
It seems that metformin can prolong the recurrence interval of bladder cancer, but the recurrence rate itself is not affected. This may be due to the small sample size and the short time of both administration and follow up in our study. Therefore, more studies with a greater sample size and longer administration and follow up times are needed.