1. Background
Due to increased life expectancy worldwide, complaints about lower urinary tract symptoms (LUTS) are becoming more common than before in males. In some western communities, 72.3% of males report at least one symptom (1, 2). According to an urologist, anatomical changes in the urinary tract and the decision of whether surgery is needed to treat the damage and disorders are mostly considered. However, a problem arises when the damage is functional and urodynamic pathology exists. In these situations, if the main pathology is not considered, surgeries (whether extensive or conservative) will likely fail.
There are various diagnostic tests for LUTS, but what is most important for the patient and the physician is the quickness, easiness, cheapness, specificity, and non-invasiveness of these tests (2). Urodynamic tests were initially developed for physiological investigations and once were the gold standard for the diagnosis of urological disorders due to their low risk of urinary tract infection, minimal effort required by the patient, and affordability. These tests have also gradually entered hospitals and clinics as useful paraclinical tests for investigating patients with urinary dysfunction. LUTS are not a measure of diagnosis for determining the pathophysiology of this system; due to the high prevalence of symptoms of the lower urinary tract and the diversity of urinary dysfunction, it is necessary to diagnose and classify patients based on diagnostic urodynamic tests to facilitate the best treatment. Because mixed disorders require multiple combined treatments, recognizing these mixed disorders is vital to ensure that the proper diagnostic tests, such as urodynamic ones (3) are ordered. These tests are useful for their ability to distinguish diseases of the lower urinary tract and also to suggest the need for appropriate treatment with respect to recognizing underlying causes; in this manner, both the control and treatment are conducted favorably.
In published studies, a diversity of symptoms and disorders has been shown; the need for diagnostic urodynamic tests has become evident because some patients did not have a good response to treatment. For instance, urodynamic testing was used to assess incontinent patients with a non-neural origin, prolapse of pelvic organs, and incontinence after prostatectomy test with stress incontinence; its advantages were obvious (4-7). The results from other studies suggest the importance of urodynamic tests in the diagnosis of bladder disorders due to Parkinson’s, multiple sclerosis, Friedreich’s ataxia, musculoskeletal disorders, primary nocturnal enuresis, bladder stenosis following shaving of the prostate gland, diuretic therapy in patients with cardiovascular diseases and diabetes, and patients with detrusor-sphincter dyssynergia (8-14). These studies showed that if the treatment is recommended based solely on patient symptoms, the results would not be satisfactory. In contrast, to find the main pathology, an investigation of the functions and dynamics of the urinary system is necessary and has been made possible through urodynamic tests.
2. Objectives
Due to the importance of these tests and their advantages, this study was performed to assess urodynamic test to diagnose symptoms of the lower urinary system.
3. Patients and Methods
In this descriptive study, 407 male patients with LUTS were referred to the urology clinic of Baghiayatallah hospital from April 2011 to March 2013 and underwent urodynamic studies. Exclusion criteria were a lack of cooperation at any stage of the study or having an indwelling catheter. Information including the chief complaint, symptoms of the present illness, past medical history, and paraclinic data (laboratory and imaging results) was recorded on special sheets, and then a standard urodynamic study was performed that included uroflowmetry (the measurement of the urine’s speed and volume), the filling phase (measurement of the urine’s speed and volume), the voiding phase (evaluation of voiding parameters, including voided urine, detrusor pressure, voiding speed, etc.), and post-void residue measurement (the amount of urine that remained in the bladder after voiding). The quantitative data were analyzed using the statistical package for the social sciences (SPSS) version 20 and expressed as means.
4. Results
The mean age of patients in the study was 50.88 years, and the third decade (20 - 30 years) had the highest incidence among patients. Urinary frequency (28.8%) and terminal dribbling (1.43%) were the most and least common complaints by patients, respectively. In total, 56.97% of patients had one symptom, 29.27% had two, and 13.76% had three or more symptoms.
4.1. Storage Phase
The systometric capacity was assessed by a gradual filling of the bladder via a normal saline injection into the bladder. A normal bladder capacity ranges from 300 - 500 mL; the mean systometric capacity of patients in this study was 366 ± 0.97 mL.
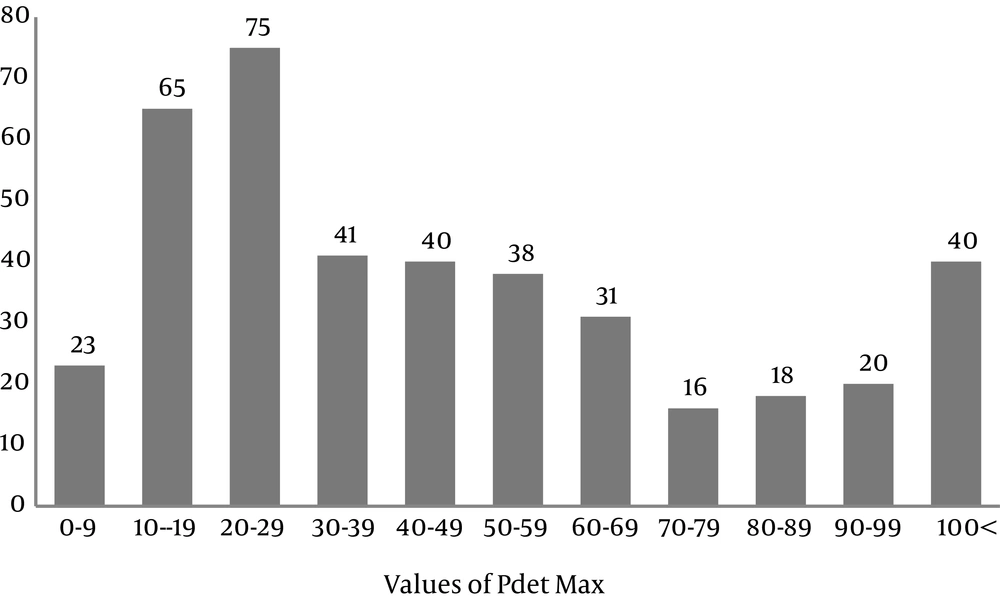
The pdetMax (maximum pressure of the detrusor) parameter was used for diagnosing the obstruction intensity both before and after the treatment:
1) Values more than 40 cm H2O suggest an obstruction.
2) Values below 20 cm H2O had no obstruction.
3) Values from 20 - 40 cm H2O were classified as undetermined.
In this study, 49.88% of patients had an obstruction, 21.62% had no obstruction, and 28.50% were undetermined. The mean PdetMax was 47.15 ± 0.21% (Figure 1). The compliance (association between the volume change and the pressure change, with a normal range of 64 - 124 cm H2O) was calculated for all patients and was high, low, and normal in 18%, 13%, and 69% of the patients, respectively.
In total, 50% of patients had normal, 31% had overactive, and 19% had hypoactive detrusor function. In electromyography (EMG: electric potential in the depolarized muscles of the perineum), 90.68% of patients were normal and 9.32% had detrusor-external sphincter dyssynergia (DESD).
4.2. Uroflowmetry and Voiding Phase
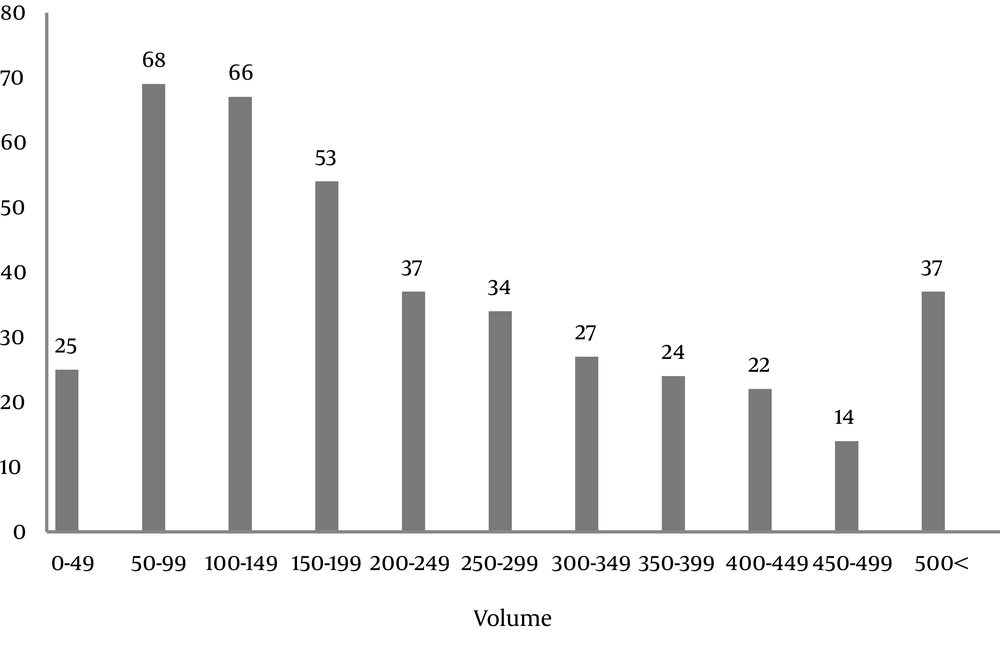
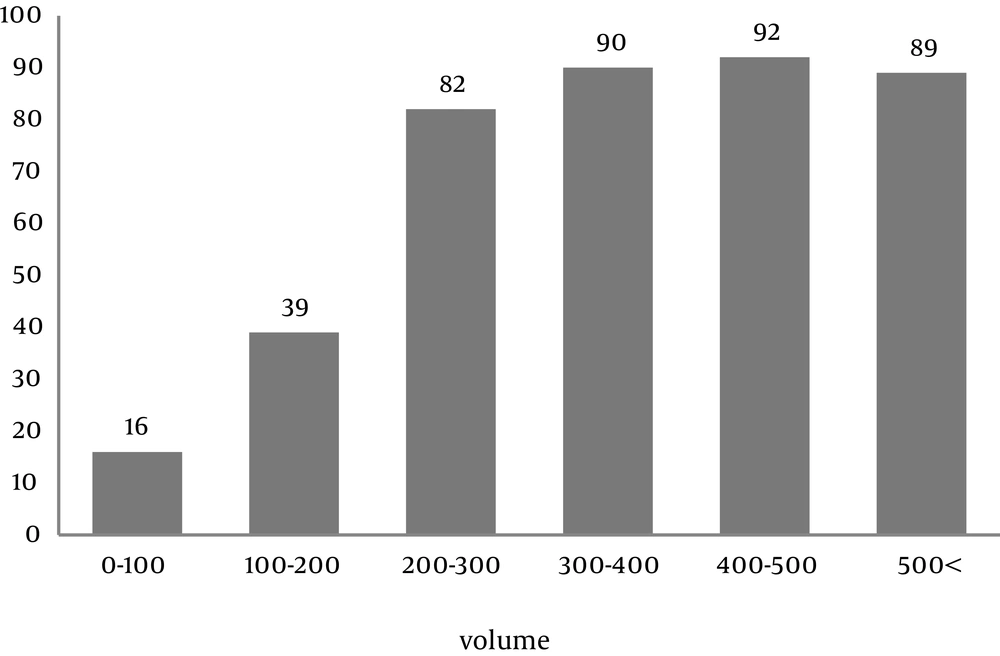
The most common pattern of voiding was bell-shaped and intermittent in 53.07% of patients, which showed that most patients had a normal voiding pattern but used abdominal pressure for evacuation, probably due to weakness of the detrusor muscle and detrusor-sphincter dyssynergia. In addition, regarding the Qmax (the maximum speed of urine flow), the normal value was 18 - 32 mL/s; 52.98% of the participants in this study were in the abnormal range, and the rest were in normal range of Qmax. The mean urine volume in patients was 187 ± 3.3 ml, which was higher than the normal range of 150 mL (Figure 2). The residual urine volume was 130 ± 2.49 mL, which was also higher than the normal range of 50 ml of the residual urine in children (Figure 3).
4.3. Association Between Symptoms and Urodynamic Findings
The most common disorders were bladder sensation disorder (SD) in 139 patients (34.06%), overactive bladder (OAB) in 95 patients (23.28%), and bladder outlet obstruction (BOO) in 52 patients (12.74%). Overall, 43 patients (10.54%) had normal findings on their urodynamic tests (Tables 1 and 2).
| Disorder | No. (%) |
|---|---|
| Sensation disorder | 139 (34.06) |
| Overactive bladder | 95 (23.28) |
| Bladder outlet obstruction | 52 (12.74) |
| Underactive detrusor | 48 (12.0) |
| Detrusor external sphincter dyssynergia | 13 (3.20) |
| Absent sensation | 10 (2.45) |
| Urethral stricture | 7 (1.73) |
| Normal | 43 (10.54) |
| Chief Complaint and Symptom | Urodynamic Disorder | No. (%) |
|---|---|---|
| Frequency | 161 (28.8) | |
| SD | 92 (12.95) | |
| OAB | 71 (10.0) | |
| BOO | 51 (7.18) | |
| UAD | 25 (3.52) | |
| Total | 239 (33.65) | |
| Enuresis | 124 (22.22) | |
| SD | 48 (6.76) | |
| OAB | 39 (5.49) | |
| BOO | 5 (0.7) | |
| Total | 92 (12.95) | |
| Incontinence | 90 (16.12) | |
| SD | 53 (7.46) | |
| OAB | 49 (6.9) | |
| BOO | 23 (3.23) | |
| Total | 125 (17.59) | |
| Incomplete emptying | 57 (10.21) | |
| SD | 30 (4.22) | |
| UAD | 16 (2.25) | |
| BOO | 19 (2.67) | |
| Total | 65 (9.14) | |
| Decreased force/caliber | 41 (7.34) | |
| UAD | 20 (2.81) | |
| BOO | 18 (2.53) | |
| OAB | 19 (1.26) | |
| Total | 57 (6.6) | |
| Dysuria | 35 (6.27) | |
| BOO | 28 (3.94) | |
| SD | 23 (9.23) | |
| OAB | 8 (1.12) | |
| Total | 59 (8.39) | |
| Retention | 18 (3.22) | |
| UAD | 25 (3.52) | |
| BOO | 10 (1.4) | |
| DSD5 | 7 (0.98) | |
| OAB | 6 (0.84) | |
| Total | 48 (6.74) | |
| Intermittency | 15 (2.68) | |
| BOO | 7 (0.98) | |
| SD | 6 (0.84) | |
| OAB | 2 (0.28) | |
| Total | 15 (2.1) | |
| Suprapubic pain | 9 (1.61) | |
| UAD | 4 (0.56) | |
| OAB | 3 (0.42) | |
| BOO | 3 (0.42) | |
| Total | 10 (1.4) | |
| Terminal dribbling | 8 (1.43) | |
| BOO | 6 (0.84) | |
| SD | 7 (0.56) | |
| Total | 13 (1.4) |
Abbreviations: SD, sensation disorder; OAB, overactive bladder; BOO, bladder outlet obstruction; UAD, underactive detrusor; DSD, detrusor-sphincter dyssynergia.
5. Discussion
In this study, the most frequent age decade was 20 - 30 years, which is consistent with research performed on young males and highlights the significance of the investigation for screening lower urinary tract disorders in this age group (15). In addition, urodynamic testing was considered a noninvasive and useful diagnostic test in this study to assess patients with chronic LUTS. On the other hand, the mean age of patients with LUTS in our study was 50.88 years old, which was similar to another report that found a mean of 56.6 years in Britain, America, and Sweden in patients from the same age decade (1).
The most common complaint of patients was urinary frequency, which was consistent with the results of Jamzadeh et al.’s study (16). Different complaints were expressed by patients in this study, which could be due to cultural diversity. This problem could distract physicians from making a proper diagnosis; thus, recognizing the effects of different cultures, providing patient guidance, and taking a complete history and physical examination are very important, as patients with OAB should undergo pelvic examination before treatment and assessment of post-void residuals (17).
Our study showed that the most common pattern on uroflowmetry test is a bell-shaped diagram + intermittency. Therefore, despite urination complaints, the test can be normal. The same results were reported in other studies (16). One of the problems with urodynamic studies is that normal flowmetry does not exclude voiding pathologies.
Yazici et al. (18) has shown that a normal Qmax value also cannot rule out voiding problems. In our study, the Qmax values were normal in more than half of the normal individuals. Therefore, a normal Qmax value is not always predictive of a normal voiding system.
The residual urinary volume was related to the Qmax In men with LUTS after benign prostatic hyperplasia (19). In the present study, the voided volume and the residual urinary volume were measured, which together determine the maximum cystometric capacity. The mean voided volume in patients was more than 150 ml for test accuracy; in addition, the residual volume was more than the normal range, which necessitates further investigation.
Investigation of bladder compliance suggested that in most patients, this parameter was appropriate at the expected filling volume. Reduction of compliance was a dangerous factor for the upper urinary tract and was seen in 13% of our patients. In previous studies, low compliance was seen in 3.9% of individuals, indicating a higher role of compliance in today’s urinary disorders (15). This discrepancy might be due to the religious beliefs of Iranian patients that could lead to urination at a lower volume of bladder filling.
Considering bladder sense disorders, the highest frequency of this disorder was early sensation, indicating that irritating symptoms are superior to other sensation disorders. In our study, EMG was also investigated. It showed that less than 10% of patients had no coordination between their detrusor and sphincter function, which suggests some degree of DESD (14). The same study showed that DESD has a high prevalence in patients with neurogenic lower urinary tract dysfunction (20).
As urinary disorders are multifactorial, physicians should consider underlying diseases to aid in making an early diagnosis. For instance, some studies suggest that the prevalence of OAB is 22.5% in patients with diabetes type II; in our study, diabetes regardless of its type was one of the underlying diseases (21).
Considering these criteria and collected data, the most common finding in this study was related to bladder SD. Similar studies suggested that in both young and old patients, the most common disorder was BOO, while this disorder was the third diagnosis in the present study (16, 22). The total frequency of bladder SD and OAB in patients with irritating symptoms was the same as the total frequency of complaints related to frequency and urinary incontinence expressed by patients, which confirms the importance of this test for diagnosis. In previous studies, urodynamic testing was proposed as the most sensitive method to diagnose detrusor over-activity, which is the base of bladder over-activity; however, in our study, OAB was the second most common disorder (23). On the other hand, this test mainly acts to distinguish over-activity to determine whether OAB is related to obstruction or neurogenic bladder. Furthermore, physicians can treat patients with either surgery or medical treatment. In addition, when patients had one complaint, urodynamic tests revealed some disorders simultaneously. Therefore, it is essential to carry out these tests prior to each surgery and intervention to reduce the chances of treatment failure that could result from the wrong diagnosis. We can also make decisions about other patients depending upon their status to determine whether urodynamic testing is necessary.
5.1. Conclusion
This study showed that if a treatment is performed based only on the patient’s symptoms, the results may not be satisfactory. Therefore, an investigation of the functions and dynamics of the urinary system is necessary to determine the main pathology, which is possible by performing urodynamic tests.