1. Background
Malnutrition is one of common problems in chronic dialysis patients (20% - 70%). Recently, protein-energy malnutrition (PEM) and systemic inflammation were found to be common in hemodialysis patients (1-4). Results of various studies show that daily intake of energy and protein in hemodialysis patients is less than the recommended dietary intake (energy: 35 kcal/kg/day and protein: 1 - 1.2 g/kg/day) (5-8). Unfortunately, 6% - 8% of hemodialysis patients suffer from severe malnutrition and 30% - 35% from moderate malnutrition. According to previous studies, in this group of patients, these factors are accompanied with reduced physical performance, increased risk of hospitalization, lower quality of life, and higher rate of mortality (9). Waste of protein during dialysis, reduction in protein intake because of anorexia or ignorance, higher metabolism during dialysis, dialysis inadequacy that leads to loss of appetite, and underlying diseases as well as economic problems are some of the major causes of malnutrition (9, 10).
Dialysis adequacy or effective dialysis dose is an important criterion in the assessment of hemodialysis patients. Measuring the dialysis adequacy is also a crucial objective for the healthcare team in a dialysis ward (11). Among the parameters for determining dialysis adequacy, urea reduction ratio (URR) and Kt/V (K: urea clearance filter; T: dialysis time; and V: urea or water distribution volume) are noteworthy. According to renal physician association (RPA) and international investigations on dialysis outcomes performed by national kidney foundation-dialysis outcomes quality initiative (NKF-DOQI), Kt/V is preferred over URR (12, 13). According to the RPA’s 1993 clinical practice guideline on adequacy, the recommended Kt/V should be at least 1.2 and the minimum URR should be greater than 65% for dialysis adequacy. NKF-DOQI also determined the same figures in 1997 and changed the target Kt/V to 1.4 in 2006, while Kt/V > 1.2 was considered as the minimum acceptable (14, 15). Dialysis adequacy is associated with appetite, nutrient intake, and nutrition rate; on the other hand, dialysis inadequacy is one of the main causes of malnutrition as well as mortality (14).
National kidney association of America recommends the periodic checking of dialysis adequacy. Studies performed in different parts of Iran showed unfavorable dialysis adequacy in hemodialysis patients; in the studies conducted in Kerman (16), Mashhad (11), Rasht (13), Hamadan, Kashan, Bojnurd, Kordestan, and Sari, the percentages of hemodialysis patients who had Kt/V < 1.2 were as follows: 91.3%, 60.4%, 23.7%, 100%, 90%, 52.5%, and 58.80%, respectively (12).
Bolasco et al. (2011) (17) stated that nutrition counseling and assessment of dialysis adequacy could be considered the first steps to improve nutritional status, after which protein-based oral nutritional supplements are recommended. In fact, special renal dietary supplements in hemodialysis patients with reduction in protein intake may lead to the improvement of nutrition status and better dialysis adequacy, which will eventually lead to a higher quality of life without the need to use phosphate-binding agents.
2. Objectives
Therefore, given the studies, high malnutrition statistics, and dialysis inadequacy, this study aims to investigate the effect of protein-based (ISO-WHEY and BCAA) oral nutritional supplements on the dialysis adequacy of hemodialysis patients.
3. Methods
The present study is a triple clinical trial that was performed in hemodialysis ward of Baqiyatallah hospital in Tehran from June to December 2014. Sample size was determined considering Altman’s nomogram, Type I error (α) as 0.05, Type II error (β) as 10%, study power as 80%, standard deviation (EZ = 2.1) from Bolasco et al. (2011) study (17), and 10% loss of sample probability. Each group (Groups A, B, and C) was assigned 22 patients, and the total number of participants was 66.
At first, eligible patients were randomly divided into three groups based on the following inclusion criteria: patients in the age group of 18 - 75 years; patients who have underwent hemodialysis at least twice a week for a minimum of 6 months; serum albumin levels less than 4 gr/dL; BMI greater than 18.5 kg/m2; no severe infection; no severe respiratory and heart failure; no chronic disease with unknown origin; no chronic liver disease, nephritic syndrome, cancer, dementia, neurologic diseases, type B hepatitis, type C hepatitis, or active infection during the previous 4 months; recent surgery during the previous 3 months or lack of follow up; and lack of parenteral nutrition as well as oral supplements.
3.1. Ethical Considerations
After receiving permission from the research committee of Baqiyatallah University of Medical Sciences and registration in the clinical trial website (IRCT201209088650N5) , in coordination with hospital administrators, the aim of the study was explained to the patients and caregivers (if necessary), and they declared their consent regarding conscious participation in the research.
3.2. Measurement Tools and Method
Personal information, including age, gender, net weight, height, marital status, education, dialysis treatment duration, and the reason for dialysis, was collected using a demographic questionnaire. For patients who needed help to complete the questionnaire (such as vision problems), the questionnaire was read and the answers were recorded without any changes or judgment. Dialysis adequacy rate was measured by determining Kt/V, which was calculated using the Daugirdas II Equation 1 and URR. Kt/V is a ratio that shows the volume of cleared plasma over urea distribution volume as follows (12, 13):


ln: natural logarithm, R: ratio of postdialysis blood urea nitrogen (BUN) to predialysis BUN (R = BUN2/BUN1); T: duration of each dialysis session, UF: ultrafiltration volume, W: weight after dialysis.
3.3. Interventions
Before intervention, in all the three groups, patients’ height was measured in centimeters and their body weight was recorded using a Seca scale (with an accuracy of 100 g). After the patients were placed in beds, about 4 mL of their blood was taken for blood urea nitrogen (BUN) and creatinine (Cr) tests before they were connected to the dialysis machine. The body mass index (BMI) was calculated by dividing the body weight (kg) by the square of height (m2). After the dialysis session, the second sampling was done for the BUN test, and the patients were weighed again. An arterial needle was used for blood sampling before dialysis, and the blood pump speed was reduced to approximately 50 - 100 mL/min for 10 - 20 s for sampling after dialysis. Then, the blood pump was stopped, and the blood sample was taken from the arterial line. The results of the tests were recorded in special forms for data collection. Before intervention, the dialysis adequacy of the patients was determined using Kt/V and URR. Moreover, training classes about nutrition and its importance in hemodialysis patients were held for nurses and patients before intervention. Then, the patients of Group A were given ISO-WHEY oral nutritional supplements and those of Group B were given BCAA oral nutritional supplements prepared by Karen Pharma and Food Supplement Co. Daily intake of supplements (as prescribed by nutrition and nephrology specialists for 2 months) was explained to the patients and caregivers. The control group (Group C) received routine diet without the use of any supplement for 2 months. Patients were reminded to take supplements and followed up through telephone calls, short messages, and in person. Nutrition counseling was done on a monthly basis, and nephrology specialist visits took place every week. The project executive was responsible to answer patients’ questions during the intervention. At the end of the first month and at the end of study, the same measurements were recorded as before intervention and URR and Kt/V were calculated in all the three groups.
3.4. Statistical Tests
IBM SPSS Statistics Base 21.0 software was used along with Chi-Square test, independent t-test, Kolmogorov-Smirnov test, one-way analysis of variance (ANOVA), and repeated measures ANOVA in order to analyze the data obtained. The minimum significance level was 0.05.
4. Results
Out of the 66 participants in the study, 61 patients completed the study period with all assessments. The most prevalent complication reported by patients was gastrointestinal problems such as nausea and bloating; as a result, nutrition and nephrology specialists recommended them to start with a lower dosage of supplements, gradually increasing it to the target prescribed dosage. Of 22 patients in the ISO-WHEY group, three patients (one female and two males) discontinued the intake of oral nutritional supplements because of gastrointestinal complications. Of the BCAA group, two patients (male) discontinued the intervention because of gastrointestinal complications and one of them underwent a transplant procedure. Thirty-three patients (54.09%) were males with an average age of 58.28 years. According to the statistical tests of Chi-Square and one-way ANOVA, the distribution of demographic variables was found to be homogenous in all the groups (Tables 1 and 2).
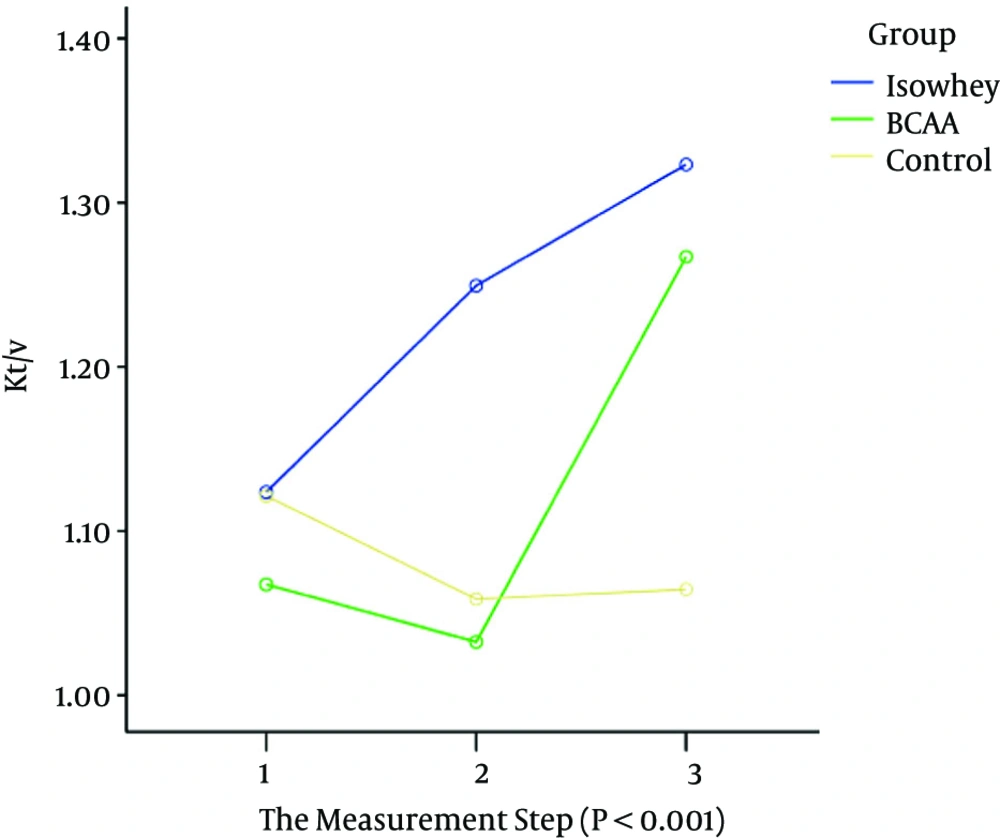
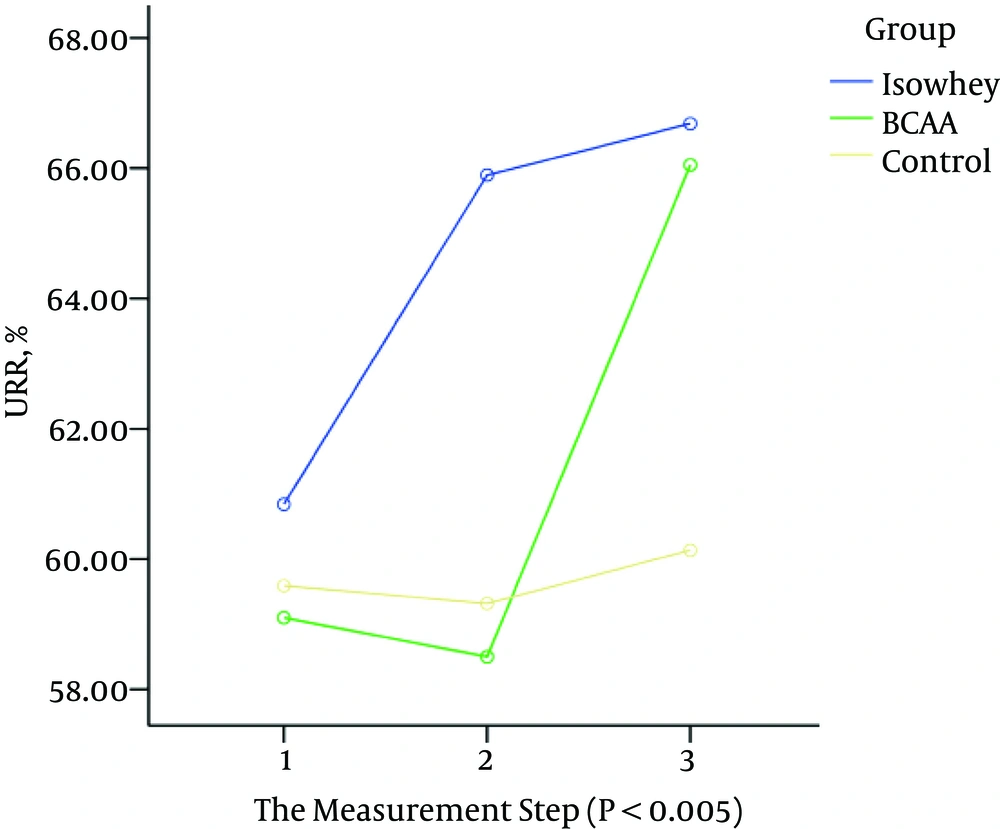
There was no significant difference between the three groups based on Kt/V and URR in the first step (before intervention) (P > 0.05). Therefore, the groups were homogenous in this step. However, there was a significant difference between the groups in the second step (1 month after intervention) and the third step (2 months after intervention) (P < 0.05) (Table 3). Moreover, repeated measures ANOVA showed a significant statistical difference in the average changes in dialysis adequacy based on Kt/V and URR among the three groups (Figures 1 and 2). The post-hoc test showed that the difference between these three groups is because of the ISO-WHEY and control groups.
| Parameter | Hemodialysis Groups | ANOVA Test | ||
|---|---|---|---|---|
| ISO-WHEY Mean (SD) | BCAA Mean (SD) | Control Mean (SD) | ||
| Age, y | 59.89 (10.75) | 53.5 (10.14) | 61.45 (14.1) | F = 2.09; P = 0.13 |
| BMI, kg/m2 | 25.67 (4.77) | 23.52 (4.07) | 26.1 (8.85) | F = 0.96; P = 0.38 |
| Hemodialysis duration, y | 4.21 (3.76) | 3.05 (5.32) | 2.84 (2.62) | F = 0.66; P = 0.51 |
| Parameter | Hemodialysis Groups | Total | Chi-Square Test | ||
|---|---|---|---|---|---|
| ISO-WHEY Frequency (%) | BCAA Frequency (%) | Control Frequency (%) | |||
| Gender | χ2 = 0.62; P = 0.73 | ||||
| Male | 9 (47.4) | 12 (60) | 12 (54.5) | 170 | |
| Female | 10 (52.6) | 8 (40) | 10 (45.5) | 130 | |
| Education | |||||
| Primary school and lower | 5 (26.3) | 6 (30) | 3 (13.6) | 112 | χ2 = 4.51; P = 0.34 |
| Diploma | 7 (36.8) | 7 (35) | 14 (63.6) | 108 | |
| University | 7 (36.8) | 7 (35) | 5 (22.7) | 80 | |
| Number of dialysis sessions per week | χ2 = 0.25; P = 0.68 | ||||
| 2 | 2 (10.53) | 1 (5) | 2 (9.09) | 20 | |
| 3 | 17 (89.47) | 19 (95.5) | 20 (90.91) | 166 | |
| Duration of a hemodialysis session | χ2 = 0.63; P = 0.49 | ||||
| < 3 h 30 min | 2 (10.53) | 3 (15) | 4 (18.18) | ||
| > 3 h 30 min | 17 (89.47) | 17 (85) | 18 (81.82) | ||
| Total | 19 (100) | 20 (100) | 22 (100) | 61 | |
| Parameter | Hemodialysis Groups | ANOVA Test | ||
|---|---|---|---|---|
| ISO-WHEY Mean (SD) | BCAA Mean (SD) | Control Mean (SD) | ||
| Before intervention | ||||
| Kt/V | 1.12 (0.14) | 1.06 (0.17) | 1.12 (0.34) | F = 0.34; P = 0.71 |
| URR | 60.84 (5.23) | 59.1 (6.19) | 59.59 (12.71) | F = 0.19; P = 0.82 |
| 1 month after intervention | ||||
| Kt/V | 1.24 (0.19) | 1.03 (0.17) | 1.05 (0.21) | F = 7.08; P = 0.002 |
| URR | 65.89 (5.16) | 58.5 (6.27) | 59.31 (7.88) | F = 7.34; P = 0.001 |
| 2 months after intervention | ||||
| Kt/V | 1.32 (0.35) | 1.26 (0.19) | 1.06 (0.26) | F = 5.04; P = 0.01 |
| URR | 66.68 (7.49) | 66.05 (6.61) | 60.13 (9.23) | F = 4.37; P = 0.01 |
| Repeated measures ANOVA | ||||
| Kt/V | F = 5.53; P < 0.001 | F = 5.53; P < 0.001 | F = 5.53; P < 0.001 | F = 5.53; P < 0.001 |
| URR | F = 3.83; P = 0.008 | F = 3.83; P = 0.008 | F = 3.83; P = 0.008 | F = 3.83; P = 0.008 |
5. Discussion
The present study aimed to investigate the effect of protein-based oral nutritional supplements on the dialysis adequacy of hemodialysis patients. Initially, ISO-WHEY, BCAA, and control groups did not show a significant difference regarding qualitative and quantitative variables as well as nutritional status; in other words, the three groups were homogenous at the first of study. Nutritional supplements are usually recommended in different studies in order to maintain nutritional status; however, it is not commonly observed (18, 19). In the case of chronic renal diseases, such as end stage renal disease (ESRD), as well as hemodialysis and peritoneal dialysis, protein absorption is incomplete, and it leads to gastrointestinal complications due to potentially toxic metabolites, such as thiol, phenol, and amines, which appear because of the fermentation of unabsorbed proteins by microbial flora in the large intestine (20, 21). To the best of our knowledge, few clinical trial studies have been performed thus far to investigate the effect of oral nutritional supplements in hemodialysis patients (22).
According to the results of this study, the dialysis adequacy of all patients studied was lower that acceptable minimum (Kt/V > 1.2) at the first of study, which reflected unfavorable dialysis adequacy in these patients (11, 12, 16). According to the studies by renal physicians association in the United States, for every 0.1 increase in Kt/V up to 1.2, the mortality rate decreases by 0.7%, and for every 5% increase in the URR up to 65%, the mortality rate decreases up to 11% (23). According to findings of the present study, protein-based oral nutritional supplements increase the dialysis adequacy based on Kt/V and URR in the ISO-WHEY and BCAA groups in comparison to the control group. Another important observation is that the average changes in dialysis adequacy based on Kt/V and URR in the ISO-WHEY and BCAA groups are higher than those of the control group. Given post-hoc test, these changes are because of the ISO-WHEY and control groups. In other words, although the intake of nutritional supplements improves the dialysis adequacy, ISO-WHEY nutritional supplements are found to have a better impact on dialysis adequacy than that of BCAA. A study performed by Bolasco et al. showed that oral amino acid supplements increase the dialysis adequacy based on Kt/V in intervention groups, although no statistically significant difference was observed (17). Findings of a study conducted by Caesar et al. (5) show no statistically significant difference based on URR in the intervention group in comparison to the control group, which may be because of the difference in sample size, daily diet in different cultures, intervention duration, and other factors influencing the dialysis adequacy (such as diet, individual’s size, training to patients, underlying diseases, filter type, dialysis duration, blood flow rate, dialysis flow rate, and urea distribution volume that in turn depend on the gender, height, and weight (24)). Given various studies and their results as well as the findings of the present study on the need to use protein-based oral nutritional supplements in dialysis patients and the prevalence of this issue, it is recommended to perform studies with larger sample size across a longer period of time. Investigating other hemodialysis outcomes such as nutritional status, quality of life, fatigue, and depression is also useful.
5.1. Conclusions
According to findings, it can be concluded that use of protein-based oral nutritional supplements will improve the dialysis adequacy in hemodialysis patients and any efforts to improve the nutritional status will be accompanied with an improvement in the dialysis adequacy, which will eventually lead to better nutritional conditions and lower mortality rates.