1. Background
Opioids are generally the preferred analgesic agents during the early postoperative period, but their use is associated with multiple adverse effects, such as nausea, vomiting, respiratory depression, and delayed recovery (1). These associations emphasize the need for an analgesic strategy that controls postoperative pain with minimal side effects (2).
Combined analgesic regimens with different mechanisms of action as a multimodal approach is becoming popular, with the aim of reducing reliance on opioids and its complications (3).
Ketamine is a centrally acting drug that exerts its main analgesic effect by antagonism of the NMDA receptors and modulates central sensory processing of pain (4). It is used alone or as an adjuvant to other analgesics in the postoperative period (5).
Paracetamol is a centrally nonopioid analgesic, and its precise mechanism of action has not yet been elucidated (6, 7). It was used in the management of postoperative pain, alone or in combination (8).
Combining paracetamol with opioids may improve analgesia, and by lowering the required doses of both medications, tolerability may be enhanced without increasing the incidence of postoperative nausea and vomiting (PONV), respiratory depression, or renal effects associated with the use of NSAIDs (9).
Tramadol is a centrally analgesic with different spectrums of activity (10). It causes the activation of both opioid and nonopioid systems, which are mainly involved in the inhibition of pain (11, 12).
2. Objectives
The aim of this randomized, double-blinded, clinical study was to evaluate the effectiveness of the combination of postoperative intravenous paracetamol plus ketamine or tramadol for early postoperative pain relief after open renal surgery. Our primary goal was to compare the analgesic effect of this combination to lowering postoperative pain scores in the early postoperative period. The secondary endpoints were to compare the following outcomes between patients who received these combinations: mean morphine consumption in the first six hours postoperatively and the presence of postoperative nausea and vomiting.
3. Patients and Methods
This randomized, double-blinded, clinical trial was conducted on 80 consecutive completely healthy patients or patients with mild systemic disease who were undergoing various types of kidney surgeries in the lithotomy position in Sina hospital in Tehran in 2014 - 2016. The study was approved by the institutional review board, and written, informed consent was obtained from all patients. Patients with a history of opium or alcohol use, history of psychological disorders, renal impairment, or definite liver disease were all excluded.
Midazolam 0.04 mg/kg and fentanyl 2 µg/kg were used as premedication for all patients. Anesthesia induction was achieved by using atracurium 0.5 mg/kg, thiopental sodium 5 mg/kg, and lidocaine 1.5 mg/kg. Fentanyl 1 µg/kg/hr and isoflurane with a minimum alveolar concentration of 1 and O2/NO 50% was maintained during the anesthesia period, and a Foley catheter was inserted for all patients. Patients were placed in a flank position during surgery.
At the end of surgery, muscular relaxation was reversed by neostigmine 50 µg/kg and atropine 20 µg/kg. After extubation, the eligible patients who had a visual analog scale (VAS) score of more than 3 were randomly assigned by using a computer random number generator to receive intravenous paracetamol (1 gr) plus tramadol (0.7 mg/kg) (P/T group) or paracetamol (1 gr) plus ketamine (0.5 mg/kg) (P/K group) within ten minutes.
The intensity of pain was measured by a 10-mm VAS, the level of consciousness and agitation were measured by RSS, and hemodynamic parameters were assessed at 5, 10, and 20 minutes after infusion, at the time of transfer from recovery to the ward, and also at one and six hours after transfer to the ward.
3.1. Ramsay Sedation Scale
1. Patient is anxious and agitated or restless, or both
2. Patient is cooperative, oriented, and tranquil
3. Patient responds to commands only
4. Patient exhibits brisk response to light glabellar tap or loud auditory stimulus
5. Patient exhibits a sluggish response to light glabellar tap or loud auditory stimulus
6. Patient exhibits no response
In the recovery room, and in any cases without proper pain control, morphine (2 mg, intravenously) was infused every five minutes, and the administrated dosages of morphine within the first six hours of drug injection were also recorded.
3.2. Statistical Analysis
Based on the results of Ali et al.’s clinical trial (10) and using 95% of the confidence level, 90% of power, and at least one mean pain score difference between the two groups, the sample size was estimated to be 39 patients in each of the two groups.
Results were presented as mean ± standard deviation (SD) for quantitative variables and were summarized by absolute frequencies and percentages for categorical variables. Categorical variables were compared using chi-square test or Fisher’s exact test when more than 20% of cells with expected count of less than five were observed. Quantitative variables were also compared with t student test or Mann-Whitney U test. For the statistical analysis, the statistical software SPSS version 16 (SPSS Inc., Chicago, IL) was used. P values of 0.05 or less were considered statistically significant.
4. Results
The 60 patients enrolled in the study were divided into PT (n = 30) or PK (n = 30) groups. There were no significant differences in the demographic data of the participants (Table 1).
| Variable | P/T Group | P/K Group | P Value |
|---|---|---|---|
| Age, y | 42.17 ± 16.06 | 46.93 ± 14.58 | 0.234 |
| Male/female | 25/15 | 29/11 | 0.222 |
| Operation time, min | 121 ± 12 | 112 ± 10 | 0.282 |
| Weight, kg | 71 ± 9 | 66.5 ± 18 | 0.11 |
aData are mean ± standard deviation.; P value < 0.05 is considered statistically significant.
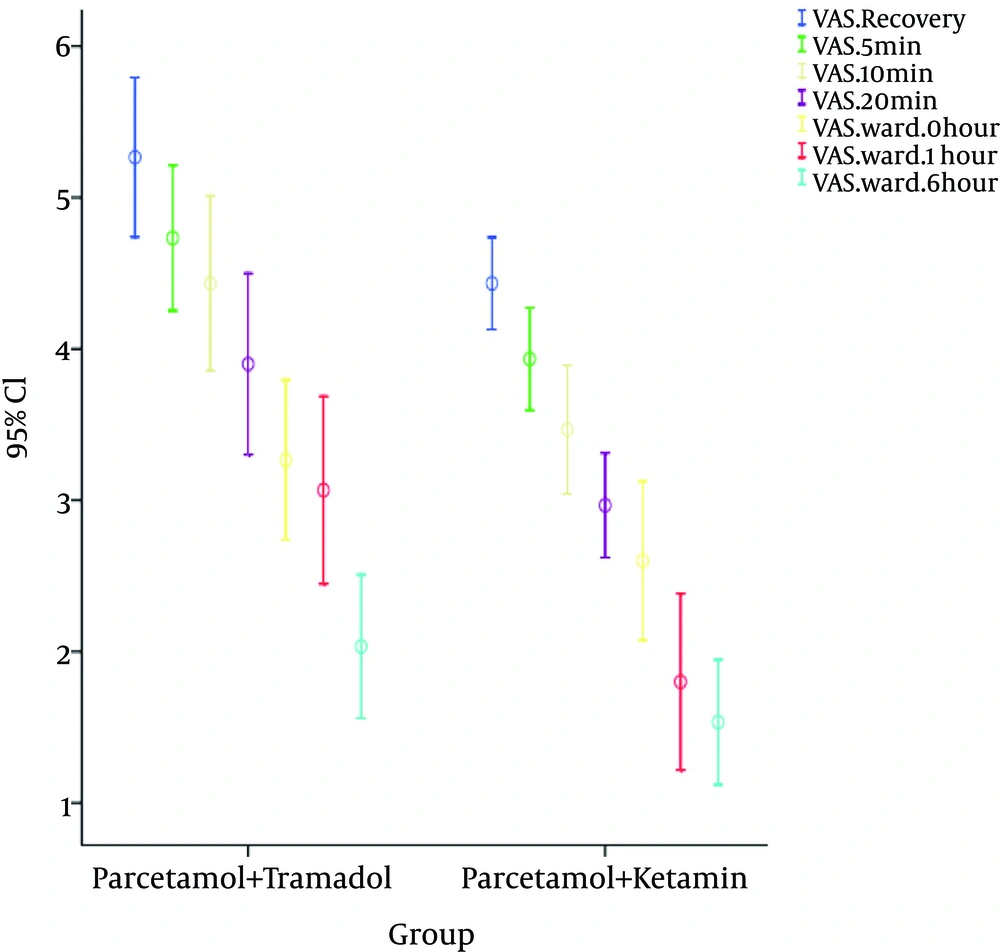
The mean pain intensity score (VAS) was lower in the PK than in the PT group during all study time points from recovery to six hours after transfer to the ward (Figure 1).
Also, the level of agitation based on the RSS score was significantly lower in the PK group than in the PT group at 10 and 20 minutes after drug infusion (Table 2).
| Group | 5 mins | 10 mins | 20 mins | Left Recovery |
|---|---|---|---|---|
| PK | 2.23 ± 0.56 | 2.83 ± 0.79 | 3.07 ± 0.64 | 2.54 ± 61 |
| PT | 2.07 ± 0.64 | 2.47 ± 0.72 | 2.52 ± 0.45 | 2.73 ± 0.83 |
| P Value | 0.29 | 0.047 | 0.031 | 0.995 |
aData are mean ± standard deviation.; P value < 0.05 is considered statistically significant.
With regard to postoperative complications, the total complication rate in the PK group was 20.0%, and in the PT group it was 53.3% that was lower in the former group (P = 0.007). In this regard, discomfort from fully catheter (i.e., catheter bladder discomfort) was more frequent in the PT group than in the PK group (43.3% versus 3.3%, P < 0.001), but there was no difference between the groups in the prevalence of PONV (13.7% versus 16.7%) or hallucination (5.7% versus 1.8%). The mean dose of morphine needed at recovery in the PK group was lower compared with the PT group (0.47 ± 0.94 mg versus 2.50 ± 1.35 mg/P = 0.001), but there was no difference in the ward (0.20 ± 0.55 mg versus 0.37 ± 0.77 mg, P = 0.337).
5. Discussion
In this clinical trial, we found that the combination of intravenous paracetamol 1 gr and intravenous ketamine 0.5 mg/kg resulted in an overall reduction in pain scores compared with intravenous paracetamol 1 gr and tramadol 0.7 mg/kg for patients undergoing renal surgery. Also, the level of agitation score during the first 20 minutes after infusion was lower in the ketamine group.
Morphine consumption during recovery was significantly reduced for patients in the ketamine group compared with the tramadol group, but was not different in the ward. Bladder catheter discomfort was more controlled with paracetamol/ketamine, but the incidence of nausea and vomiting was the same between the two groups.
Paracetamol is one of the most commonly used agents for relieving mild to moderate pain. Paracetamol is thought to inhibit or modulate mediators of pain peripherally at the site of injury, and there is increasing evidence that paracetamol acts at the level of the CNS to produce analgesia, likely by inhibiting CNS prostaglandin formation (13). The onset time of intravenous acetaminophen for 15 minutes infusion is 5 minutes, and the time to meaningful pain relief is 8 minutes, reaching maximum pain relief after 15 minutes (14). Paracetamol’s analgesic effects persist for approximately two hours (15). The primary aim of this study was to show that ketamine was more potent than tramadol in the early stages of the postoperative period. Many studies have demonstrated significant effectiveness of ketamine in controlling postoperative pain, increasing time to first analgesic request, and decreasing overall opioids required, as well as demonstrating fewer of the opioid-related side effects, such as PONV (16). In several studies, the combination of ketamine with opioids had a synergistic or additive analgesic effect that led to decreased morphine consumption during the 24-hour postoperative period (17).
Tramadol is a weak opioid with a mean potency one-tenth that of morphine. To achieve the best analgesic effect, we must increase the dosage of drugs that lead to more complications (18). In many studies, the combination of low doses of tramadol with acetaminophen at the end of surgery decreased the pain intensity during the postoperative period (19). In our study, we found that this combination markedly reduced pain intensity from the end of surgery through six hours postoperatively, although this reduction less than ketamine group.
Many studies have reported that, by combining drugs with different mechanisms of action and pharmacokinetic profiles as in the results of this study, we can enhance efficacy, even with lower doses of the individual drugs (20).
In our analysis, the secondary outcome the mean morphine consumption in recovery was significantly lower in the ketamine group, which is consistent with several previous studies demonstrating that the administration of paracetamol, ketamine, tramadol, or a combination of them reduces the quantity of analgesic administered postoperatively (17, 19, 21).
The most frequent complication in our study was catheter bladder discomfort (CBDC), which was very high in the PT group (43.3%). Catheter bladder discomfort is a common complication in recovery, with an incidence of 55 - 63% in male patients (22). Similar to our finding were the results of Agarwal et al., who previously treated CBDC with low-dose intravenous ketamine (0.25 mg/kg) in recovery (23). They also used tramadol 1.5 mg/ kg intravenously 30 minutes before extubation to decrease the incidence and severity of CRBD (24).
Shariat Moharari et al. found that preemptive administration of IV ketamine (0.5 mg/kg) can reduce the incidence and severity of CRBD in the early postoperative period (25).
These observational studies demonstrate that we can use low doses of ketamine to control CBDC, which is similar to the findings of our study.
In our study, the incidence of PONV did not differ significantly between the PK and PT groups; the incidences were 13.7% and 16.7%, respectively. Similar to our findings were the results of Rawal et al. (26), who previously reported incidences of 25% for PONV in patients treated with paracetamol plus tramadol.
Song et al. performed a randomized trial on the effects of ketamine as an adjunct to intravenous patient-controlled analgesia in 50 patients undergoing lumbar spinal surgery and at high risk of postoperative nausea and vomiting. They concluded that ketamine reduce postoperative fentanyl consumption without a reduction in the incidence of PONV (27).
In conclusion, the combination of intravenous paracetamol 1 gr and intravenous ketamine 0.5 mg/kg resulted in an overall reduction in pain scores, lower opioid consumption, and lower agitation score compared with intravenous paracetamol 1 gr and tramadol 0.7 mg/kg for patients undergoing renal surgery. Also, the paracetamol/ketamine combination is a useful strategy to control catheter bladder discomfort in the recovery period.