1. Background
Stress urinary incontinence (SUI) is the complaint of involuntary leakage on effort, exertion, sneezing, or coughing (1). A postal survey carried out across four European countries on more than 17,000 participants found that 35% of the women had experienced incontinence, with SUI being the most prevalent type of incontinence (2). It is reported that 50% of the women presenting urinary incontinence exhibit pure SUI, whereas 30% experience mixed urinary incontinence (2). In a hospital-based study on urinary incontinence in Iran, 411 females participated and out of 111 (27%) women with urinary incontinence, 77 (18.7%) had SUI, which was the most prevalent type (3). Overall, 30% of women develop SUI within five years after their first vaginal delivery (4).
SUI impairs the quality of life (QOL) in women suffering from it and is associated with significant social and financial costs and depression (4). In a survey on the QOL of women with urinary incontinence in Iran, none of the subjects with SUI could lead a comfortable life and 68.2% had low and very low QOL (5). Another survey on QOL of 105 Iranian women with urinary incontinence demonstrated that the patients had inferior mental health and QOL (6).
The staggering number of procedures to treat SUI reflects a lack of consensus on an appropriate intervention for this problem (7). Anterior colporrhaphy with the Kelly’s Plication, albeit an old method to treat SUI, is still a popular method among gynecology practitioners (8). Gynecologists employ this method to treat SUI as a common procedure in Afzalipour Hospital, where this study was conducted. The transobturator tape (TOT) procedure is a new method to treat SUI, which is universally used since its introduction by Delorme in 2001 (9).
2. Objectives
The current study aimed to compare the results between anterior colporrhaphy with the Kelly’s plication and TOT procedure to treat SUI in a one-year follow-up.
3. Patients and Methods
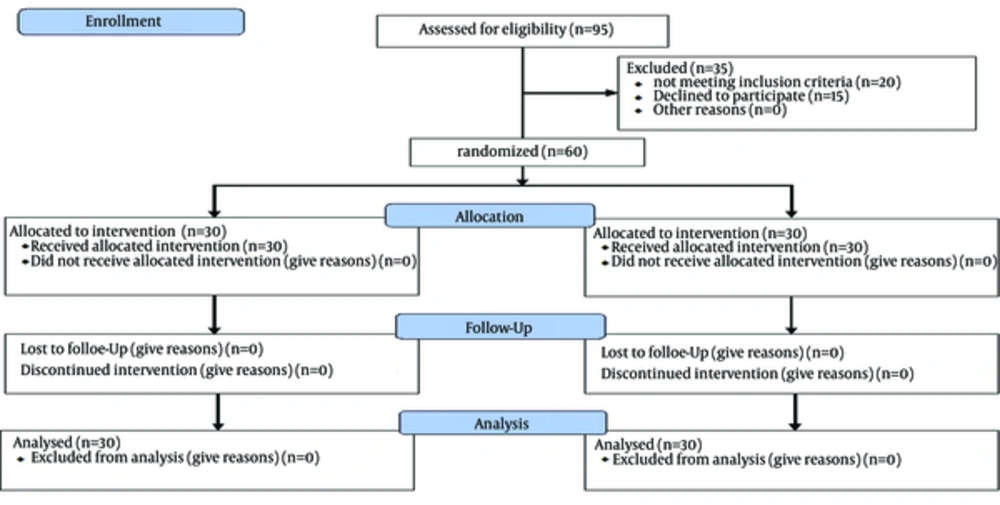
This parallel randomized clinical trial was conducted on 60 patients with SUI referred to the Gynecology Clinic of Afzalipour Hospital affiliated to Kerman University of Medical Sciences, Iran, from 2011 to 2012, after approval of the Ethics Committee of Kerman University of Medical Sciences (reference number: K/89/154) (Figure 1). All the patients signed an informed consent after receiving a detailed description of the study and its purpose.
The patients were randomly divided in to anterior colporrhaphy with the Kelly’s plication group and the TOT group using the simple random sampling method (30 patients in each group). The randomization was computerized via www.randomizer.org/form.htm.
The inclusion criteria were comprised of history of involuntary urine escape in rising intra-abdominal pressure (e.g. while laughing and sneezing and straining without pelvic pain or sense of pelvic organ prolapse (POP), lack of pathologic vaginal discharge, lack of organomegaly, positive cough-stress test and post-voiding residual volume < 50 mL. Urodynamic investigation was done on the cases suspected of having pure SUI. All the eligible cases did not respond to medical treatment.
The exclusion criteria consisted of other types of urinary system diseases or urinary incontinence; history of incontinence surgery; any disease that would affect the urinary system such as neurological diseases (e.g. Multiple Sclerosis), psychological diseases and chronic lung diseases (e.g. chronic obstructive pulmonary disease), consumption of drugs such as benzodiazepines, anticholinergics and calcium channel blockers, alcohol or opium addiction; and body mass index ≥ 30. In the TOT cases, the out-in technique was performed using Aris® tapes (Coloplast Ltd., France). All the surgeries were performed by the same surgeon.
The patients were followed up in one month, six months and one year after the surgery. Evaluation was done according to the Blaivas and Jacobs classification, viz. a) cured: absence of incontinence; b) improved: frequency of incontinence episodes less than once every two weeks; and c) failure: frequency of incontinence episodes more than once a week (10). A senior surgeon, who did not take part in the surgeries, performed the follow-up process.
The patients’ demographic data (i.e. age, parity, duration of SUI, menstruation history, occupation and delivery method), history, physical examination and follow-ups were recorded. Also, the data on the patients’ complications, including urethral erosion, bladder or vaginal perforation, abscess or hematoma in the surgical site, recurrent vaginal discharge due to the tape erosion and new urinary disorder were recorded.
The statistical analyses were performed using STATA 11 (College Station, Texas 77845 USA). The independent t-test and Chi-square test (Fisher exact test) were used to compare the results between the two groups. To compare the outcome rates, considering their ordinal nature, between the two surgery groups at each follow-up time point, the ordinal generalized estimating equation (GEE) was performed. Age was taken as a covariant in this model. A P value < 0.05 was considered statistically significant.
4. Results
Sixty patients with SUI underwent anterior colporrhaphy with the Kelly’s plication or the TOT procedure. The demographic and clinical data are provided in Table 1.
| Demographic and Clinical Data | Kelly’ Plication b | TOT | P Value c |
|---|---|---|---|
| Age, yd | 37.80 ± 8.19 | 44.13 ± 5.55 | 0.009 |
| Parity d | 3.93 ± 1.7 | 4.43 ± 2.1 | 0.307 |
| Duration of stress urinary incontinence, y d | 3.43 ± 3.7 | 2.90 ± 2.1 | 0.499 |
| Menstruation e | 0.4 | ||
| Reproductive period | 26 (86.7) | 22 (73.3) | |
| Premenopausal period | 1 (3.3) | 3 (10.0) | |
| Menopausal period | 3 (10.0) | 5 (16.7) | |
| Occupation e | 0.717 | ||
| Housewife | 27 (90.0) | 27 (90.0) | |
| No heavy-lifting job | 1 (3.3) | 2 (6.7) | |
| Heavy-lifting job | 2 (6.7) | 1 (3.3) | |
| Delivery method e | 0.278 | ||
| NVD | 27 (90.0) | 24 (80.0) | |
| NVD & Caesarean | 3 (10.0) | 6 (20.0) | |
| Cystocele stage e,f | 0.121 | ||
| I | 12 (40) | 18 (60) | |
| II | 18 (60) | 12 (40) |
aAbbreviations: NVD, normal vaginal delivery.
bKelly’s Plication: Anterior colporrhaphy with Kelly’s Plication.
cP value < 0.05 was considered significant.
d The values are presented as mean ± SD.
e The values are presented as No. (%).
f Pelvic organ prolapse-quantification (POP-Q) classification.
All the 30 patients in the anterior colporrhaphy with the Kelly plication group had general anesthesia. Among the 30 patients in the TOT group, 25 (83.3%) patients had general anesthesia, 2 (6.7%) had spinal anesthesia and 3 (10.0%) received sedation. The shortest operation timewas in sedation anesthesia (10 minutes). The mean operation time in the TOT group (22.8 ± 8.2 minutes) was significantly shorter than that of the anterior colporrhaphy with the Kelly’s Plication group (44.7 ± 6.1 minutes) (P = 0.00001).
The Foley catheter was removed the next day in the TOT group and after 48 hours in the anterior colporrhaphy with the Kelly plication group.
In the anterior colporrhaphy with the Kelly’s Plication group, one patient had urine retention after discharge from the hospital. She was readmitted to the hospital and the Foley caterer was fixed for 24 hours and then clamped (for three hours) and opened (for one hour) three times. The patient was discharged. However, she accompanied by another patient in this group still occasionally complained of incomplete emptying of urine. Sonography showed no post-voiding residue, and SUI was cured in both.
In the TOT group, 3 (10%) patients had vaginal perforation by passing a tunneler. In each of the subjects, the tunneler was removed, the procedure was repeated, and the perforation site was repaired. During the follow-ups, no complications were observed in these subjects.
De novo urge incontinence happened in two subjects of the TOT group. Before the operation, the urodynamic test proved that one of these patients had pure SUI, and the other one entered the study with a positive cough-stress test. One of the cured patients in the TOT group had no problem voiding in a European toilet, but when using the common type of toilets in Iran (i e, squat toilets), she had to put pressure on her suprapubic region or void in a semi-sitting position. Transient pain in the groin disturbed 5 (16.6%) patients in the TOT group. Except for one patient with three weeks of pain, the others had no pain in the groin after 48 hours.
Dyspareunia occurred in one TOT subject and was resolved after four months. In the anterior colporrhaphy with the Kelly Plication group, dyspareunia occurred in four subjects. Dyspareunia was resolved in one subject after four months, while it continued in the other 3 (10%).
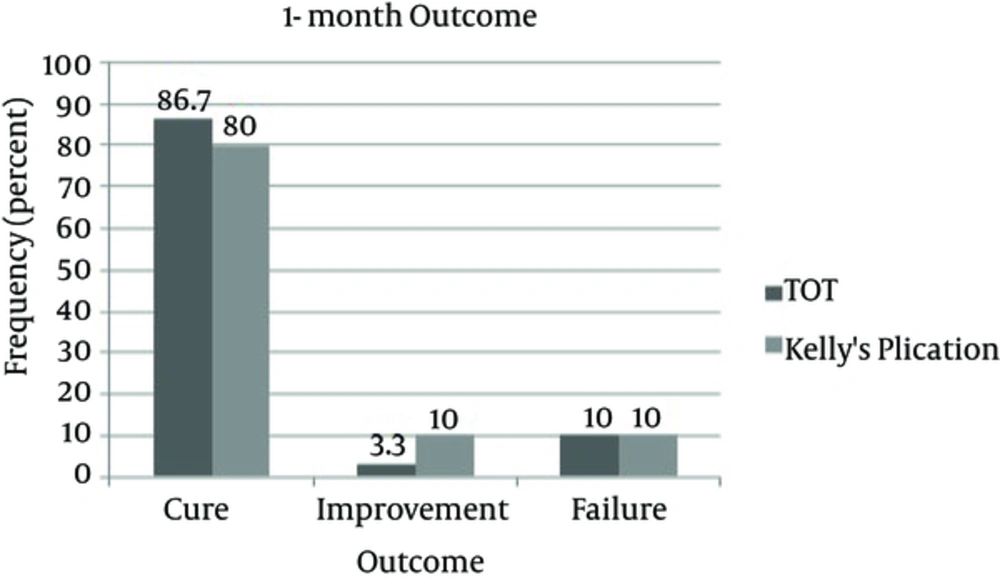
One month after surgery, no significant difference was found between the two groups (P = 0.68) (Figure 2).
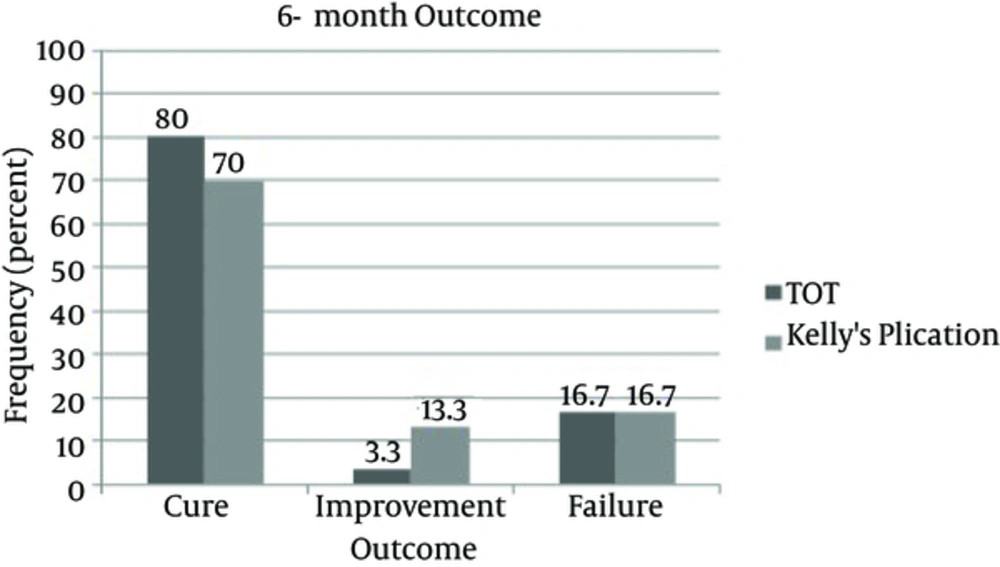
At six months’ follow-up, two patients among the cured cases had failure of treatment in each group, and one patient among the cured cases in the anterior colporrhaphy with the Kelly plication group joined the improved cases. Therefore, the failure rate increased to 5 (16.7%) cases in each group. There was no significant difference between the groups (P = 0.54) (Figure 3).
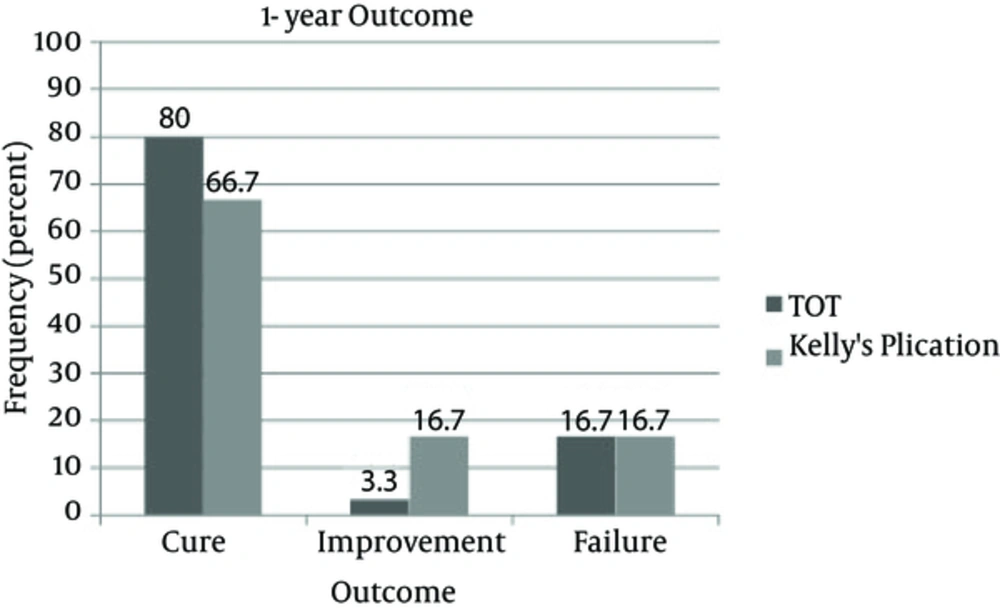
After a year of follow-up, there were no changes in the TOT group’s results. However, one cured patient in the anterior colporrhaphy with the Kelly’s Plication group was categorized as an improved case. No significant difference was found between the two groups after a one-year follow-up (P = 0.22) (Figure 4).
The results of the ordinal GEE analysis indicated no significant differences in the cure rates between the two surgery groups on follow-ups (Odds Ratio [OR]: 0.56, 95% Confidence Interval [CI]: 0.18 - 1.74; P = 0.32).
Despite the significant difference in the mean age between the two groups (Table 1), this variable had no significant effect on the surgery outcomes in the ordinal GEE analysis (OR: 1.01, 95%CI: 0.94 - 1.08; P = 0.74).
5. Discussion
The outcome of SUI treatment is perfect if the patient achieves the best urine control, at least for morbidity and improvement in the QOL. Since Delorme used the TOT procedure in 2001 to treat SUI (9), it is universally performed as a low-invasive method in medical centers. On the other hand, anterior vaginal colporrhaphy with the Kelly’s Plication, despite several reports on its low long-term success rate, is used by gynecologists in numerous centers, including Afzalipour Hospital, to treat SUI.
Evidence supporting the value of combination surgery is still limited in females with POP and SUI and two reviews underscored the need for further research (11). In the current study, patients were included with a pure SUI complaint, without pelvic pain or sense of POP and cystocele grades of I or II according to the pelvic organ prolapse-quantification (POP-Q) classification. Accordingly, no additional vaginal prolapse surgery was performed in the TOT group or the TOT procedure in the anterior colporrhaphy with the Kelly plication group.
In the current study, there was no significant difference after a one-year follow-up between the two procedures. The obtained results showed that a short operation time and a short Foley fixation duration were the benefits of the TOT procedure, compared with anterior colporrhaphy with the Kelly plication.
Regarding the operative complications, there were no urethral or bladder injuries in the two groups. Vaginal erosion and dyspareunia were reported in several studies on the TOT procedure, but there were no such complications in the TOT subjects (12) of the current study. However, in the anterior colporrhaphy with the Kelly’s plication group, dyspareunia continued in 10% of the cases. There was no de novo urgency in the anterior colporrhaphy with the Kelly’s Plication group, whereas 6.6% of the 30 cases in the TOT group had de novo urgency. In a study on the TOT, among 604 subjects, the de novo urgency rate was 1.5% in 131 cases after a one-year follow-up (13). A study on the TOT and laparoscopic Burch procedures and another study on the TOT procedure found de novo urgency in 5.2% of 16 TOT cases and 3.7% of 54 TOT cases, respectively (14, 15). The complications of the TOT procedure in a study on 81 subjects were 4.9% vaginal erosion, 4.9% de novo urgency, 1.2% unrecognized vesicovaginal fistula and 3.7% urinary retention plus postoperative residue (16). One of the reasons for such differences between the results is probably the dissimilarity of sample size.
In all available sources, there is no clinical trial to compare anterior colporrhaphy with the Kelly plication and the TOT procedure, but these two modalities are assessed separately and compared with other methods.
In the TOT group, the cure rates at one month, six months and one year follow-ups were 86.7%, 80% and 80%, respectively. Different studies from 2003 to 2008 reported cure rates in the TOT groups from 80.5% to 96% at four months to 40 months follow-ups. In contrast, Mellier et al. had 100% pure SUI cases with a 95% cure rate in the TOT group (12). In another study with 17 ± 4.7 months of follow-up, the objective cure rate in the TOT group was 89.9% (17). In a randomized clinical trial on 40 subjects with SUI, there was no significant difference between the laparoscopic Burch and TOT procedures after a six-months follow-up, and the cure rate in the TOT group was 84.2% (14). A clinical trial on the treatment of 35 SUI patients, who underwent the TOT procedure, showed a 91.4% cure rate, 8.6% improvement rate and no failure after an average follow-up period of 14 months, which is, albeit better than the current study results, of no significance (10). Another research on the TOT efficacy to manage SUI after a one-year follow-up reported a subjective cure rate of 90.7% among 54 patients, while anterior and posterior colporrhaphy was done in 81.5% of the patients and vaginal hysterectomy in 9.25% (15). A comparison between the TOT and Transobturator Adjustable tape (TOA) procedures with six months of follow-up reported that 72.3% of the 47 patients were cured in the TOT group, which is a relatively lower rate than that of the current study (18).
Two other clinical trials on the TOT to treat SUI with a sample size almost similar to that of the current study were previously conducted. In the study on the tension-free vaginal tape method versus the TOT procedure, there was a 91.4% cure rate in the TOT group after a mean follow-up period of 30 months. In the other study on the TOT versus laparoscopic Burch procedures, the cure rate in the TOT group was 90.3% after a mean follow-up period of 22 months. In both studies, there were no significant differences between the two procedures after the follow-ups (19, 20).
In the current study, 80%, 70% and 66.7% of the patients were cured one, six and twelve months after anterior colporrhaphy with the Kelly’s plication, respectively. There are success rate reports of about 37% - 84% in a five-year follow-up (8). In a study, the comparison between the Burch colposuspension and anterior colporrhaphy with the Kelly’s plication showed a 75% success rate in the latter modality after six months and there was no significant difference between the two procedures (21). A long-term study on anterior colporrhaphy with the Kelly plication to treat SUI found no failure after a one-year follow-up, but 46.8% of the cases had failure after a five-year follow-up (8). Elsewhere, a study on the long-term advantages of the Kelly plication to treat SUI reported the 50% recurrence rate of SUI after two years (22). In six studies between 1995 and 2005, which compared anterior colporrhaphy with the Kelly plication and the other methods of SUI treatment, the cure rates in anterior colporrhaphy with the Kelly plication groups were 55% - 71% (23).
The foremost among the limitations of the current study were the small sample size, short-term follow-up and lack of a QOL questionnaire. Further studies with greater sample sizes, use of QOL questionnaires, and long-term follow-ups are required to confirm the results of the current study.
The current study concluded no significant difference between the TOT procedure and anterior colporrhaphy with the Kelly plication to treat SUI at short-term follow-ups. Nevertheless, the TOT cure rate was higher than that of anterior colporrhaphy with the Kelly plication during the follow-ups. According to the aforementioned studies and referenced literature, the success rate in anterior colporrhaphy with the Kelly’s plication may decrease in the long term, while there are limited long-term follow-up studies on the TOT procedure. Since the outcome rates of each follow-up in the current study were quite close between the two groups, it was supposed that increasing the sample size would not have made a significant difference to the results. Nonetheless, it is likely that in a long-term follow-up, the results change.