1. Background
Infertility is a major clinical concern affecting 15% of couples and in almost half of these cases, male infertility is the sole or a contributing factor (1). The most common cause of male infertility is varicocele which can be detected in 15% of the general male population and 35 to 40% of infertile men and is generally correctable or at least treatable (2-4). The most common indication for the treatment of varicocele is still male subfertility.
Several mechanisms are suggested regarding the infertility in men with varicocele. These include hypoxia, stasis, testicular venous hypertension, elevated testicular temperature, increase in spermatic vein catecholamine, and increased oxidative stress (5).
Oxidative stress (OS) is considered as a major cause that leads to infertility (6). OS results from an imbalance between the production of reactive oxygen species (ROS) and their efficient removal by available antioxidant systems which can lead to an increased rate of cellular damage. It is recommended that elevated ROS levels in the semen may be an etiologic factor for male infertility (7, 8). Even though, small amounts of ROS are necessary for sperm activation, these agents can cause damage to the sperm in higher concentrations (9, 10). Thus, recent studies have investigated the different antioxidant agents to prevent this damage on sperm metabolism and fertilizing capacity.
Crocus sativusL., commonly known as saffron, is a perennial herb of the Iridaceae family with antioxidative properties (11, 12). Its dried red stigma has been extensively used as a spice and food colorant. Saffron is used in folk medicine as an anti-spasmodic, eupeptic, pain killer, anti-catarrhal, carminative, diaphoretic, expectorant, stimulant, stomachic, aphrodisiac, and emmenagogue. Recent studies have demonstrated that saffron and its constituents have antioxidant, anti-microbial, anti-convulsant, anti-depressant, anticancer, and anti-inflammatory effects and also reduce withdrawal syndrome and improve male erectile dysfunction (11-15).
Several studies on animal models and on men have suggested the role of saffron on sperm parameter improvement (16-20). Due to the possible role of saffron on sperm parameter improvement, we aimed to evaluate the effect of saffron on semen analysis in infertile men with clinical varicocele after varicocelectomy.
2. Methods
In this randomized clinical trial, patients with infertility and clinical varicocele who referred for varicocelectomy to urology clinics of Tabriz University of Medical Sciences were recruited. All married men between 20 to 35 years old with the duration of infertility more than one year with varicocele willing to participate were included. Partners of study participants were below 35 years of age with normal hormonal profiles, regular menstrual cycles, and no signs of female infertility in their medical records. Those with any systemic or urogenital disease or any history of childhood disease, use of approved drugs or illegal ones such as opioid, stimulants, hallucinogens and inhalants, or any history of testis trauma that might affect the spermatogenesis were excluded. Also, patients with acute infections, previous history of varicocelectomy, unilateral testicular atrophy, or with Azoospermia were excluded.
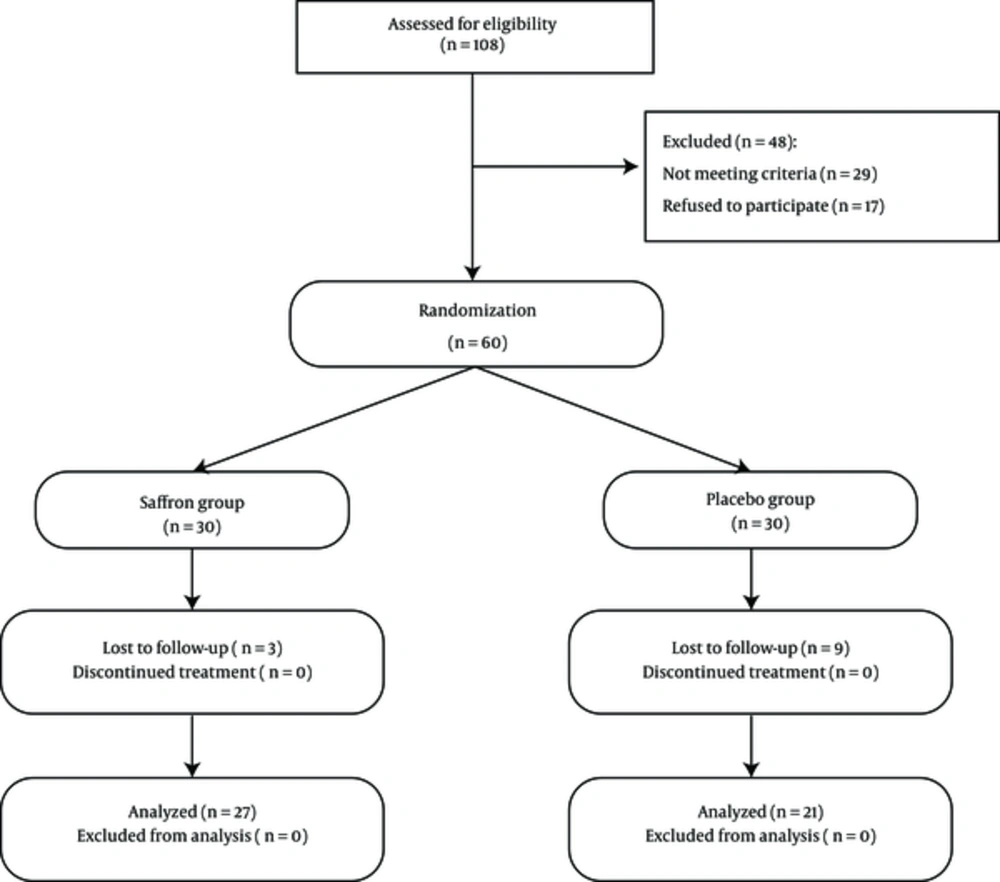
The trial is powered to detect an effect size of d ≥ 0.70 as statistically significant in a two-tailed test with α = 0.05 and power of 0.80 with N = 26 per condition. As there was the possibility that some patients do not complete the study, we included 30 patients in saffron and placebo groups. Using RANDLIST 1.2 software, random numbers were produced and according to the sample size, patients were enrolled into the study. During the study period, three patients from saffron group and 9 patients from placebo group refused to complete the study for personal issues and the study was conducted with 27 patients in the saffron group and 21 patients in the placebo group (Figure 1).
All patients underwent a standard, diagnostic infertility evaluation. A detailed history and complete physical examination was performed by the same physician. Testicular ultrasonography was performed on all patients. Testis volume was assessed by physical examination and testicular ultrasonography. A varicocele identified at scrotal examination, performed with the patient in the standing position and during Valsalva’s maneuver was classified as grade I (palpable only during Valsalva’s maneuver), grade II (palpable without Valsalva maneuver), and grade III (visible without need for palpation) (21).
A specific brand of the available saffron in the area was obtained for all the patients. Using the maceration method, saffron capsules containing sixty milligrams of the concentrated powder were prepared (22). The capsules were manufactured by pharmacology labs of our university. Starch powder was used with the same weight inside identical capsules for the placebo group. Study subjects received saffron capsules or placebo every other day for six months. The first dose was given 3 days after varicocelectomy. No other treatment options were considered during the study period.
Before initiating the treatment with saffron and at the end of the study period, semen analysis was performed. Samples were obtained 48 to 72 hours after the patients’ last sexual contact. Analyses were performed by the aid of the Computer-Assisted Sperm Analysis in less than 1 hour after sample collection. Semen specimens were evaluated according to WHO criteria (23).
2.1. Statistical Analysis
All statistical tests were performed using SPSS for windows Version 17 (Chicago, IL, USA). Quantitative data were presented as mean ± standard deviation (SD), while qualitative data were demonstrated as frequency and percent (%). Independent t test or Mann-Whitney U test for quantitative date and chi-square test or Fisher’s exact tests, as appropriate, were used to compare data between the two groups. Paired samples t test was used to compare findings before and after treatment in each group. A P value of < 0.05 was considered statistically significant.
3. Results
In this study, 27 patients received saffron and 21 patients received placebo for six months. Table 1 demonstrates the baseline findings of the groups which had no significant difference.
| Variables | Intervention Group | Control Group | P Value |
|---|---|---|---|
| Age, y | 29.63 ± 5.03 | 28.10 ± 4.16 | 0.27 |
| Infertility period, y | 3.62 ± 0.70 | 3.79 ± 0.78 | 0.88 |
| Testis size | |||
| Right | 19.56 ± 0.70 | 19.44 ± 0.70 | 0.61 |
| Left | 19.33 ± 1.14 | 19.11 ± 0.90 | 0.49 |
| Varicocele grade, No. (%) | |||
| Grade I | 11 (40.7) | 7 (33.3) | 0.47 |
| Grade II | 2 (7.4) | 4 (19) | |
| Grade III | 14 (51.9) | 10 (47.6) | |
| FSH | 4.91 ± 2.68 | 3.73 ± 1.72 | 0.36 |
Sperm analyses before and after treatment are demonstrated in Table 2. There was no significant difference between groups regarding values before treatment as well as in semen volume, morphology, and sperm count post-treatment, but motility was significantly higher in the saffron group. The findings before and after treatment were also compared in each group. There were no significant differences in placebo group, but in saffron group motility was significantly increased after treatment (P < 0.001).
| Variables | Intervention Group | Control Group | P Value |
|---|---|---|---|
| Pre-treatment | |||
| Volume | 2.77 ± 1.10 | 3.17 ± 1.63 | 0.07 |
| Morphology | 23.48 ± 3.48 | 29.90 ± 5.40 | 0.3 |
| Count | 43.93 ± 26.16 | 46.38 ± 40.68 | 0.8 |
| Motility (M1 + M2) | 18.11 ± 10.05 | 19.61 ± 12.57 | 0.64 |
| Post-treatment | |||
| Volume | 3.30 ± 1.84 | 4.00 ± 2.13 | 0.08 |
| Morphology | 25.59 ± 3.96 | 34.14 ± 5.59 | 0.20 |
| Count | 46.29 ± 5.77 | 65.62 ± 12.62 | 0.14 |
| Motility (M1 + M2) | 30.00 ± 14.46 | 21.71 ± 11.45 | 0.03a |
aP is two-sided significant.
There was one (3.7%) complication (irritative urinary syndrome) in saffron group.
4. Discussion
Previous studies have reported ROS increase in the sperm of infertile men with varicocele (24-26). So, therapies with antioxidant properties are recommended in these patients to prevent ROS damage to metabolism, sperm motility, and morphology and to increase the fertility capacity. Many antioxidants have been studied and their role in decreasing infertility through sperm motility improvement is demonstrated (27).
In this randomized clinical trial, we evaluated the effect of saffron, a herb with anti-oxidant properties, on sperm parameters in patients with clinical varicocele undergoing varicocelectomy and found that six month treatment with saffron significantly improved sperm motility but had no effect on other parameters.
There are only three studies on animal models and two studies on male infertile subjects evaluating the effect of saffron on sperm parameters (16-20). Although animal studies were indicative of the potential role of saffron in improving all semen parameters (16-18), studies on humans could not confirm these results. Heidary et al. (19) observed that saffron is effective on sperm morphology and motility in nonsmoker infertile men with oligospermia, but it does not increase sperm count. However, Safarinejad et al. (20) in their research on saffron showed no statistically significant improvements in any of the studied semen parameters in infertile males with idiopathic oligoasthenoteratozoospermia compared with placebo group. In this study, we only found significant improvement in sperm motility. The dissimilarity between animal and human studies may be caused by inherent differences between rats and humans and also it could be due to administrating different doses and the treatment period.
Previous studies have recommended that saffron improves sperm parameters by its antioxidant properties to prevent oxidative stress (15, 28).
Oxidative stress is induced by ROS or free radicals. ROS are needed for capacitation, the acrosome reaction, and ultimately fertilization; however, excessive levels of ROS may damage a variety of biomolecules such as lipids, amino acids, carbohydrates, protein, and DNA and negatively impact sperm quality (8, 9). It is shown that increased levels of ROS are correlated with decreased sperm motility (29), increased sperm DNA damage (30), sperm cellular membrane lipid peroxidation (31), and decreased efficacy of oocyte–sperm fusion (32). These free radicals induce sperm cell injury through several pathways and can significantly impact both sperm quality and function (32, 33).
Recent systemic reviews of the oral antioxidants on male infertility reported improvement in either sperm quality after antioxidant therapy due to their role in protecting semen from ROS (27, 34). However, Safarinejad et al. (20) observed that saffron does not significantly improve total seminal plasma antioxidant capacity. It is possible that saffron does not have proper effects on male infertility, but further studies are necessary in this regard.
Our study has some limitations. The low sample size is an important limitation of our study which could have affected the results. We did not evaluate the ROS levels, neither total seminal plasma antioxidant capacity nor their change during the treatment with saffron and could not conclude about the saffron effects in these regards. Most studies on human have evaluated the saffron effects compared to placebo and did not compare their efficacy with other antioxidants. Further studies are necessary to clarify the exact role of saffron on sperm parameters.
4.1. Conclusion
Our results showed that except improving sperm motility, saffron has no effect on other semen parameters in infertile male with clinical varicocele after varicocelectomy. However, further studies are necessary to evaluate the effective suitable dose, prescription fashion, and prescription intervals.