1. Introduction
The shortage of cadaveric organ donors has led to look after new strategies for transplantation. Live donation, non-heart beating donors and extended-criteria are well-established options in renal transplantation; however, experience in kidney transplantation with congenital anomalies is sparse and limited to small reports of isolated cases, without an established agreement regarding what should be the attitude towards these potential grafts currently undervalued. In this article, a review of available literature, specially focused on surgical approach and evaluation of allografts, and a presentation of our experience is reported.
Horseshoe kidney is the most common anatomical renal variation with an incidence that ranges from 600 to 800 adults (0 - 25% of the population), being more common in males (2:1). VA Politano transplanted the first case of a horseshoe kidney in 1963, implanting half of a horseshoe kidney into a monozygotic twin of the donor; however, it was not until 1975 when Nelson published the first case (1). It consists of two renal masses vertically separated on each side of the midline, usually joined at the lower pole by a parenchymal or fibrous isthmus that traverses the median plane. Familiar aggregation with a low penetrance gene pattern is possible. There is an association between horseshoe kidneys and genetic abnormalities such as chromosome 18 trisomy and Turner syndrome. They may be associated with cardiovascular malformations, central nervous system, and skeletal deformities. Genital anomalies are found in 4% of males (hypospadias and cryptorchidism) and in 7% of females (bicorn uterus and vagina). Anomalies of the urinary system are, also, more frequent: vesicoureteral reflux up to 50%, ureteral duplication 10%, and obstruction of the ureteral junction by 20%. Although the majority of these kidneys are asymptomatic, they present a higher incidence of recurrent infections and lithiasis (30 - 50%). This higher incidence of lithiasis seems to be caused by metabolic disorders in 50% (hypercalciuria, hyperoxaluria, hypocitraturia and hypouricosuria) more than to drainage defects because of anatomic anomalies. The most common symptom is abdominal pain that can irradiate to the lower lumbar region. 30% of patients have urinary tract infections. Abdominal mass palpation leads to diagnosis in only 10% of cases. One-third of the horseshoe kidneys may have hydronephrosis as a result of an obstruction of the ureteral junction, either by the high insertion of the ureter in the pelvis, its situation in front of the isthmus, or its aberrant vascularization. An increased incidence of squamous and transitional cell tumours has been documented which may be due to increased frequency of lithiasis, obstruction, and chronic infection.
In normal development, kidneys rotate medially and ascend gradually over the posterior abdominal wall. The horseshoe kidney is a result of an accidental fusion of the ureteral buds between the sixth and fourth week of gestation (2). Although most horseshoe kidneys are fused in the lower pole, less than 5% are through the upper pole. There are two types of fusion, medial and lateral. In lateral fusion, the calyceal system can drain a portion of the kidney that extends across the midline. Migration is usually incomplete and the kidneys are located lower in the abdomen than usual. The isthmus usually crosses the sacral promontory at the level of L3-L4 immediately below the birth of the inferior mesenteric artery in the aorta, and usually contains functioning parenchyma, being only a fibrous band in 15% of cases. Vascularization is highly variable both in number and origin. Only 30% have a single artery for each side of the horseshoe kidney. The isthmus may receive branches from the renal arteries, the aorta, inferior mesenteric, iliac or sacral arteries.
Vascular anatomy is determinant in transplantation technique. In 1969, Graves (3) tried to establish a classification based on the arterial vascularization of horseshoe kidneys dividing them into 3 types. Kidney can be divided into five segments without collateral circulation, receiving independent arterial supply. Apical and posterior segments receive supply from the other three segments. Depending on arterial supply to upper, midline, and lower segment, three types are stablished. In Type I, a single lateral artery directly from the aorta irrigates all segments of both sides. Type II consists in upper and middle segments supplied by one lateral aortic branch to each side and the lower pole has an independent supply. In type III, the upper, middle, and lower segments have independent supply, being the lower pole supplied by aortic branches or from iliac arteries (4).
The number of calyces is normal, but its orientation is atypical. Because the kidney does not rotate, the calyces are directed backwards and the axis of each pelvis remains in the lateral plane oblique or vertical on an imaginary line that goes from the inferior pole to the superior pole. The lower calyces extend downward or towards the midline and drain into the isthmus and may extend into the spine. The ureter can be inserted higher into the pelvis and arranged outwards; with its bladder insertion being normal. It should be taken into account when using these kidneys that the length of the ureter is usually shorter.
2. Case Presentation
2.1. Case 1
After 18 hours of cold ischemia, horseshoe kidney was trasplantated to a 55-year-old female recipient with end-stage renal failure of unknown origin on hemodialysis. Pretransplant creatinine level was 477.37 mmol/L. En bloc transplantation was performed into right iliac fossa. Kidney showed three arteries, two veins in a inferior vena cava patch, and two separated ureters. One artery came from the isthmus and an end-to-end anastomosis to internal iliac artery was done. The other two arteries were anastomosed separately to external iliac by end-to-side anastomosis. Extra vesical ureteroneocistostomy of each ureter was independently done and intubed with double J catheter to avoid fistula formation. Warm ischemia time was 60 minutes. First serum creatinine decline was at the second postoperative day and 67.19 mol/L at discharge. Hemodialysis was not necessary immediately on postransplant. Persistent lymphocele required to maintain drainage for 20 days after surgery as unique complication. After nineteen months of follow-up, renal function remained at 69.84 mmol/L.
2.2. Case 2
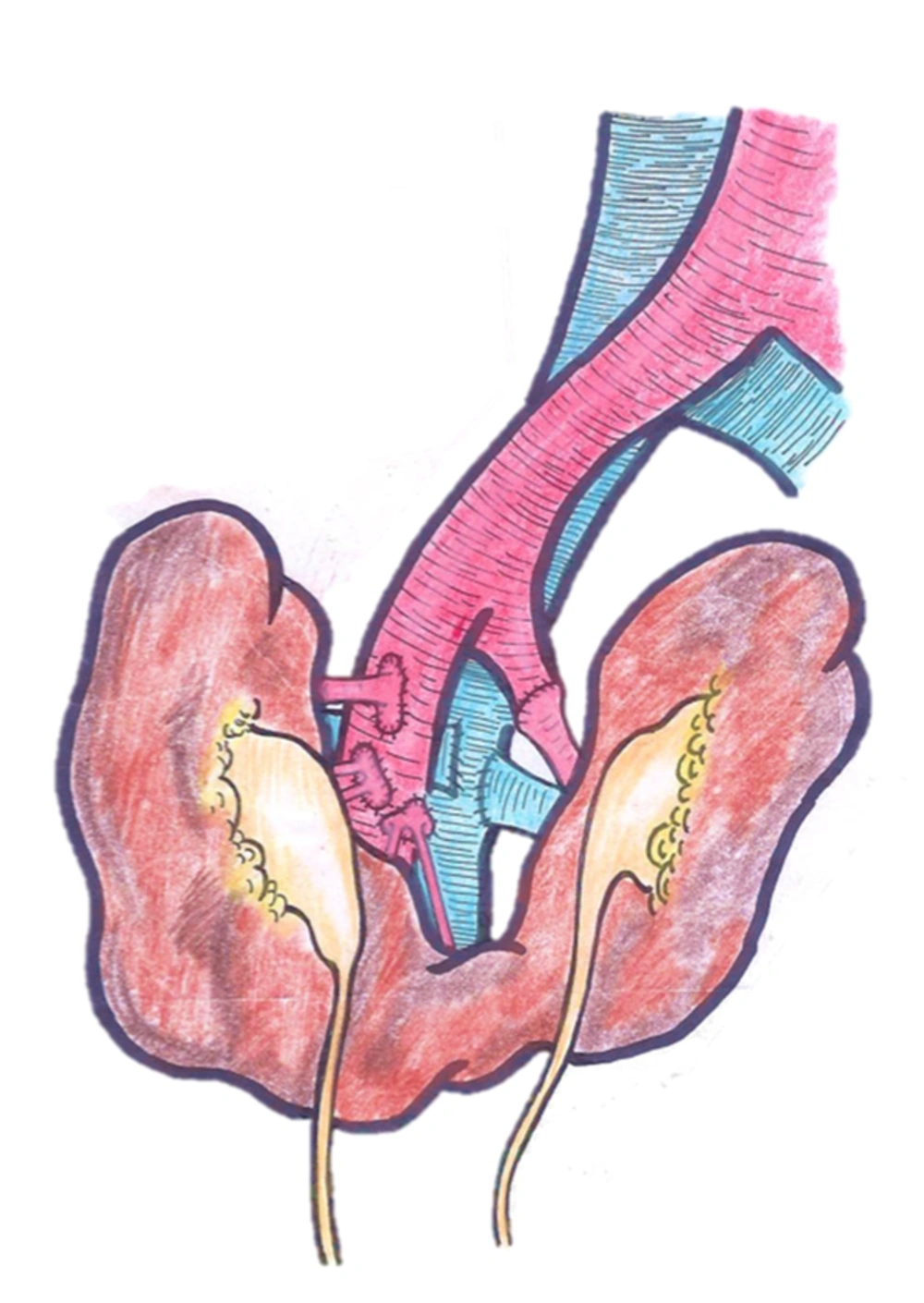
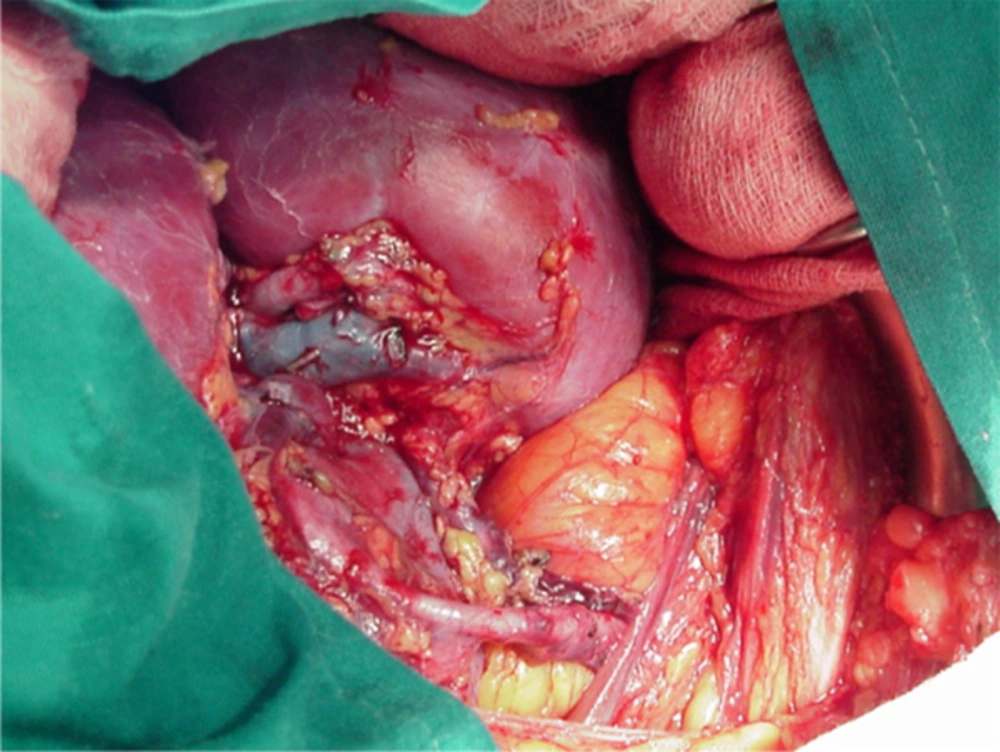
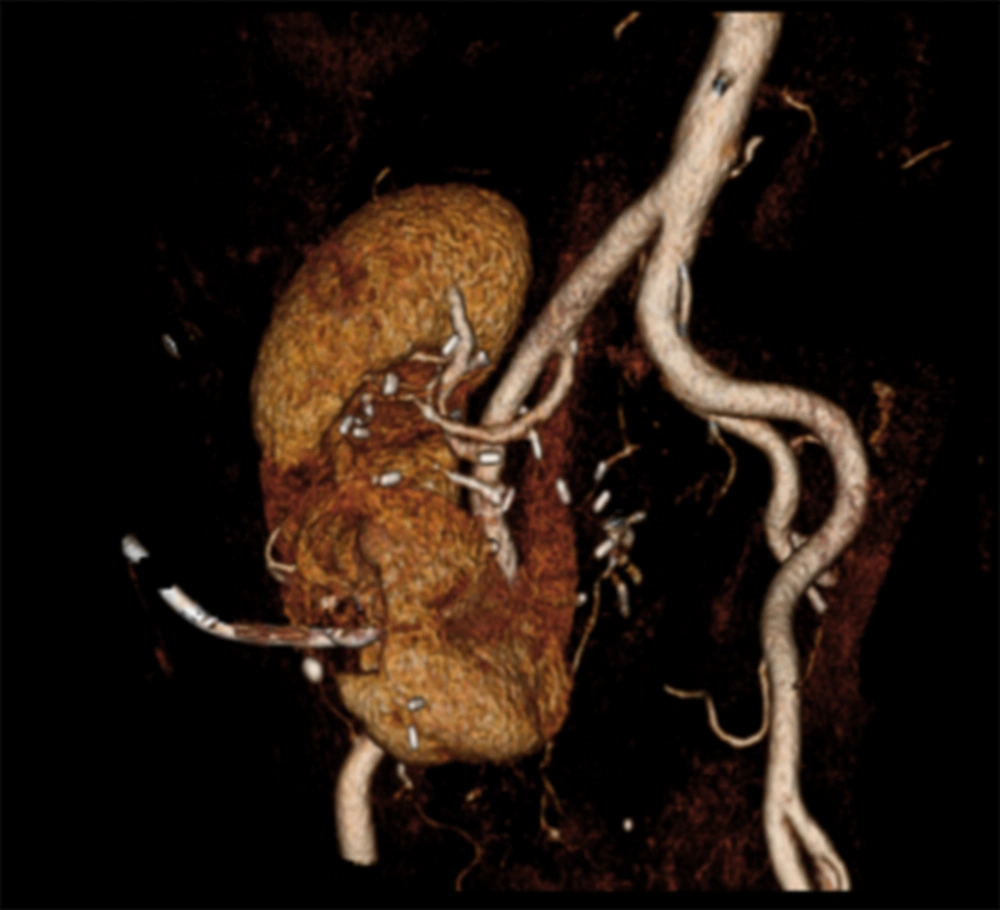
Recipient was a 53-year-old man who had been on haemodialysis for the past two years because of tubulointerstitial chronic kidney disease. After injection of methylene blue, a parenchimatous isthmus was confirmed so transplantation was done in bloc (Figure 1). Vascular anatomy complexity made necessary multiple anastomosis. Right side showed five arteries: one to upper pole, two arteries on a patch to the mid pole, and other two arteries to the lower pole and the isthmus on another patch. Three termino-lateral anastomosis to the external iliac were done. Left half with an unique artery was anastomosed end to end to hypogastric artery (Figures 2 and 3). Ureteroneocistoctomy of the two independent ureters was done separately and intubed with doble J catheter. After ten days of delayed graft function, creatinine levels started to decline and discharge serum creatinine was 159.12 mmol/L.
Readmission was done Three months after transplantation, asymptomatic patient was readmitted because of rising creatinine levels of 212.16 mmol/L. Doppler ultrasound did not show any findings and a computed tomography (CT) with vascular reconstruction was done, showing a critical stenosis of one of the right side arteries. Percutaneous balloon angioplasty was done and stenosis was satisfactorily resolved, returning creatinine levels to basal 159.12 mmol/L. After stenosis resolution, creatinine levels continued to decrease to 79.56 mmol/L and remained stable until sixteen years of follow-up.
A slight ascent of creatinine of 123.76 mmol/L at the sixteenth year after transplantation with no other symptoms, required further studies with CT that found a 8 mm radiotransparent lithiasis that caused obstruction of the left moiety (Figure 4). A percutaneous nephrostomy was placed and two lithotripsy sessions were performed without resolution of the lithiasis. After failed percutaneous lithotripsy, a combined retrograde and anterograde ureterorrenoscopy was done without complete fragmentation, and alkalinizing oral treatment with bicarbonate with a double J stent on the allograft was maintained for 3 months. After control CT showed dissapearance of the lithiasis and double J was removed. Bicarbonate was maintained for three months. Renal function at seventeen years of follow-up remained at 74.26 mmol/L.
3. Discussion
Multiple factors must be considered when accepting these organs for transplantation. Most of donors with congenital anomalies are asymptomatic patients (5). History of urinary tract infections, lithiasis or hematuria should be evaluated (6). If confirmed, radiological evaluation with CT with vascular and urinary reconstruction is mandatory. Special consideration should be given to the number and disposition of renal vessels, as well as the higher incidence of collecting system defects such as duplicity, ureterocele, anomalies of the uretero pelvic junction, vesicoureteral obstruction, and reflux. Fusion anomalies can cause the collector system to communicate in the midline. Splitting into the isthmus can result in damaged calyces, fistula formation, and indentation of sectioned edges. It is important, therefore, to have a meticulous bench surgery and identification of structures with repair of those damages that can take place when splitting the two halves. The presence of a crossover of the collecting system should be inspected, either by retrograde injection of radiological contrast or methylene blue. If the isthmus is sectioned, parenchymal defect should be repaired to avoid the appearance of fistulas and haemorrhages. Suture can be performed either with resorbable material or GIA-type stapler. If the isthmus is broad with abundant parenchyma and multiple vessels, it is better to perform in bloc transplant. Because of the lower position of these kidneys in the abdomen, the smaller length of the ureter should be taken into account during the organ extraction, obtaining as much ureter longitude as possible near its orthotopic insertion into the bladder. Arterial cannulation should be placed distally in the common or external iliac artery to ensure good perfusion of the organs and avoid vascular lesions. Kidneys should be removed in bloc with a long segment of aorta, cava and iliac vessels for bench surgery. Extensions of cava and aorta and terminolateral anastomosis can be made to the iliac vessels to give greater length to the donor vessels. Sometimes transplantation to the aorta and the cava is an option (7). Multiple vascular anastomosis are often necessary because of anomalous vasculature. If possible, transplantation into ipsilateral iliac fossa is advisable because veins are usually shorter. The most frequent complications of these transplants are urinary fistula and haemorrhage (6.4%) in the isthmus at the level of the parenchyma section. Primary non-function occurs around 5 to 18% and mostly due to vessels thrombosis (6%). The position of the allograft into the recipient can also variate, and orientation must be checked to avoid kinking or vascular stretching. Decision about en bloc transplantation or separating the two renal moieties and transplanting into two recipients must consider both allograft and recipient variables, such as vascular anatomy, technical feasibility to separate the two kidneys, graft size, and donors anatomy (2, 8).
According to registers, 60% of all horseshoe kidneys are suitable for transplantation.
Stroosma et al. in 2001(9) carried out a retrospective worldwide register from 1975 to 2000, finding 80 horseshoe kidneys transplanted into 97 recipients, including two living donation allografts. 23 kidneys were transplanted en bloc and 57 were divided. After division, 17 halves were rejected for transplantation. Median follow-up was 14 months in the en bloc group and 24 months in the split group. When dividing the isthmus, 77% was crossed by renal parenchyma, according to previous data reported in the literature. Vascular distribution was variable, from 1 to 8 arteries and from 1 to 6 veins. Those kidneys with greater vascular complexity were those transplanted en bloc. Cold ischemia ranged from 24 hours in the en block group (9 - 48) to 22 hours in the divided (2 - 61). Complication rate in en bloc transplant was 13% (2 ureteral necrosis and one lithiasis) and 11.3% in the divided group (2 sepsis, 2 urinary fistulas, 2 ureteral strictures, and one adult respiratory distress syndrome). Primary non function occurred in 4.3% in the en bloc and 13.4% in the divided and was not associated with complex vascular anatomy; being arterial thrombosis the most frequent cause. Median creatinine levels were 90 and 150 mmol /L in the en bloc and split group at the longest- term follow up. Results were similar to conventional transplants, although this data may be biased by the lack of notification of those transplants with poor results.
In a previous publication by the same authors (10), data of 34 patients (included in the global analysis) were disaggregated, and results were evaluated separately in the divided kidneys compared to those transplanted en block and in a control group. The frequency of primary non-function, immunological failure, and surgical complications (11.3% divided, 13% block), did not show statistically significant differences. Five-year graft survival was 83.3%, 76.4%, and 75.1 % for the en bloc, split, and control group, respectively.
3.1. Conclusion
Although experience with horseshoe kidney transplantation is scarce, the use of these organs with fusion anomalies has to be considered given the short and long-term results reported. However, surgical technique and selection of donors must be carried out carefully. Past medical history of the donor should be investigated based on discarding pathology of the urinary system. In addition, kidneys must be extracted en bloc to allow a through exploration of the collecting system and the vascular tree. Despite a possible bias in the communication of cases of horseshoe kidney transplantation, there is an underutilization of these with the loss of potential organs that it entails. Results are comparable to those of conventional kidneys, despite greater surgical complexity of the procedure, with graft and patient survival comparable to conventional transplantation. Management of complications during the follow-up is similar to normal kidneys, but anatomical considerations must be kept in mind to avoid graft damages. Endourological and endovascular procedures are feasible but must be done by experienced transplantation teams.