1. Introduction
Primary Hyperparathyroidism (PHPT) is a disease that may be asymptomatic and discovered after a routine chemistry profile or may cause symptoms of hypercalcemia and be associated with symptoms of renal stone and bone disease (1). Nephrolithiasis occurs in 7% to 40% of patients with PHPT (2, 3). Approximately 5% of patients with nephrolithiasis will have hyperparathyroidism (4). Although Primary Hyperparathyroidism (PHPT) is asymptomatic in most patients, its main clinical manifestation is nephrolithiasis (5).
Finding of long-lasting cases of PHPT with progressive renal damage is infrequent. In this report, a case of hypercalcemia secondary to long lasting PHPT, is presented, which eventually led to renal failure.
2. Case Presentation
This report presents a 55-year-old male with nausea and weakness from 3 days prior to referral. He was a smoker and had a history of chronic kidney disease and multiple kidney stones from 6 years ago that had undergone multiple intervention by extracorporeal shock wave lithotripsy (ESWL) and transurethral lithotripsy (TUL) and insertion of double j stent (DJ) due to right obstructive renal stone 2 weeks ago.
Spiral abdominopelvice CT scan showed renal stone in the left kidney and DJ stent in the right kidney without evidence of hydronephrosis (Figure 1). The results of lab exams included:
Blood Urea Nitrogen (BUN): 48 mg/dL, creatinine: 2.83 mg/dL with base-line serum creatinine of 1.7 mg/dL, urinalysis showing hematuria, calcium: 15.8 mg/dL, 25-hydroxy vitamin D: 25 mg/dL, phosphorus: 4.4, serum albumin: 4 mg/dL, intact parathyroid hormone (iPTH) = 1046 pg/mL. Lateral skull X-ray showed salt and pepper appearance (Figure 2).
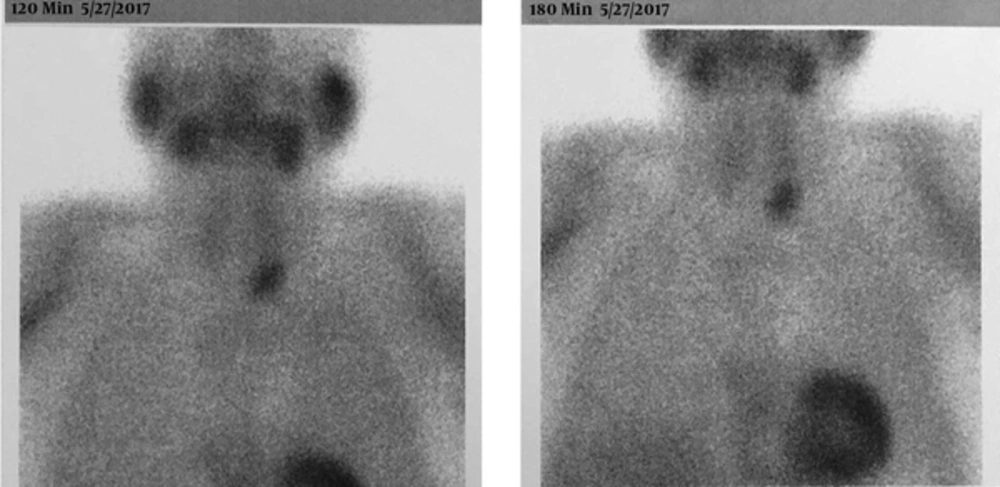
He was treated with hydration by Sodium Chloride (0.9%) solution followed by furosemide, dexamethasone, Pamidronate, and calcitonin. His creatinine dropped to 1.95 and calcium decreased to 10.2 mg/dL. Due to presence of hypercalcemia and high iPTH and normal phosphorus in spite of renal failure, PHPT was suspected. He underwent parathyroid scan using sestamibi (T99scan MIBI, nuclear scan). The T99 scan MIBI, nuclear showed parathyroid adenoma in the inferior pole of the right thyroid (Figure 3). Having primary hyperparathyroidism with standard indications for surgery, the abnormal gland was removed by surgery. Three days after surgery, calcium level returned to the normal range.
3. Discussion
Primary Hyperparathyroidism (PHPT) is a common condition affecting up to 4 per 1000 individuals, and the majority of cases are due to adenoma or hyperplasia of the gland (6).
Although primary Hyperparathyroidism (PHPT) is asymptomatic in most patients, its main clinical manifestation is nephrolithiasis (5).
In a reported case series about nephrolithiasis, incidence of PHPT was 2% to 8% (7). More than 50% of cases with hyperparathyroidism had renal manifestations, such as nephrolithiasis and nephrocalcinosis (8).
One of the clinical manifestations in symptomatic patients, who had no previous history of renal disorder, was nephrolithiasis. Other involvements were in cardiovascular, neuromuscular, and gastrointestinal systems, with different symptoms (9). The classic manifestations of hyperparathyroid bone disease are osteitis fibrosa and brown tumors (1).
In symptomatic pHPT, proximal muscles weakness can occur, which is accompanied by progressive fatigue and malaise (10).
The most important renal manifestation of PHPT is nephrolithiasis, chronic renal insufficiency, and a variety of abnormalities in renal tubular function, particularly decreased concentrating ability (1). About 20% of patients with PHPT have nephrolithiasis caused by chronic hypercalcemia (11). Nephrolithiasis is considered as a risk factor for chronic kidney disease; patients with kidney stone that develop chronic kidney disease correspond from 0.8% to 17.5%. Renal failure in patients with nephrolithiasis results from various factors, including obstructive uropathy, recurrent urinary tract infection, frequent surgeries, and coexistent medical diseases (12).
Besides urological procedures themselves, especially surgery, can damage the renal parenchyma, especially if interventions are repeated (13). Deposition of crystals in the tubules and interstitium of the kidneys is another mechanism for renal injury, mainly observed in patients with genetically transmitted metabolic disorders (13).
Solitary parathyroid adenoma accounts for 85% of cases of PHPT (14). The diagnosis of the disease is based on high normal calcium or hypercalcemia with lower normal limit phosphorous and high alkaline phosphatase and finally high PTH values (1).
The guidelines for treatment of asymptomatic PHPT is surgical intervention in patients, who have serum calcium level > 1 mg/dL above the upper limit of normal, renal stone, and a glomerular filtration rate (GFR) less than 60 mL/minute (15).
In the current case, the patient had renal insufficiency, urolithiasis, increased serum calcium level and parathyroid adenoma, thus underwent parathyroid gland resection.
The diagnosis could be delayed due to nonspecific involvements in several systems, including the urinary, neuralgic, gastrointestinal, and musculoskeletal system. In the present case, the patient had neglected to evaluate the etiologies of recurrent nephrolithiasis and metabolic investigation for 6 years, and the renal outcome was due to late diagnosis.
3.1. Conclusion
More attention must be paid to patients with recurrent nephrolithiasis, and such patients must be evaluated for PHPT before progressing to CKD. Also, routine serum calcium measurement are recommended to determine the cases of this disease in its earlier stages before the start of complications.