1. Introduction
About 97% of vesicovaginal fistulae (VVF) are because of obstetric trauma in underdeveloped countries and gynecologic surgery in developed countries. Some important causes of VVF are tissue sloughing, pressure necrosis and edema. In contrast to the developing countries, in the developed countries obstetrics have a low rate of VVF (1). Less commonly, VVFs may be between the cervix and bladder, ureters and vagina, or between the urethra and vagina. Also, ureteral injuries are common in 10 - 15% of VVFs. Consequently, the incidence of VVF may change owing to surgical management changes in the developed and underdeveloped countries (2).
The incidence rate of VVF after total abdominal hysterectomy (TAH) is 0.5 - 2%, while other studies suggested only a 0.05% incidence rate of injury to the bladder or ureter in these cases. VVF may occur as a result of bladder and ureter injuries in 1% of gynecologic procedures, and about 75% of VVF cases are associated with hysterectomy, and if about 500,000 hysterectomies are performed each year, 5000 patients will experience an injury. VVF attributable to a vaginal foreign body is a rare complaint in girls younger than 13 years old referring to gynecology clinics. Blood-tinged and foul smelling vaginal discharge are the main complaints in patients with vaginal foreign body. A variety of foreign bodies such as lock pin, head clamp, pencil, jumbo glass, and toys have been extruded from the vagina of young girls, but the most common foreign body found in 80% of cases is toilet paper (3).
Hereby, we report a rare case who presented with VVF due to a vaginal foreign body (marbles) leading to stone formation in the vagina. In this case, probably the foreign body existed in the vagina for a long time, and the formation of a VVF caused vaginal stone formation due to continuous leakage of urine.
2. Case Presentation
A 16-year-old girl was referred to pelvic floor disorders clinic with the chief complaint of urinary incontinence as continuous leakage of urine since eight years ago, which was aggravated by the maneuver of valsalva.
The patient mentioned a history of urinary problems like urinary incontinence and nocturia since the age of eight. Cystoscopy by an urologist was performed and urinary reflux was detected. The patient underwent an anti-reflux surgery, but her complaints did not disappear after this operation. Also, the patient had a history of oxybutynyl consumption for urinary incontinence, which was not effective in the improvement of the symptoms.
An ultrasound examination was performed. In trans-abdominal sonography, a 60-mm mass-like image with regular and distinct borders was observed in the posterior vaginal wall. A computed tomography (CT) scan without contrast was carried out to better localize the position of the mass-like lesion and determine its precise diameter. A hyposignal mass with the diameter of 40 × 22 mm was detected in the upper third of the vaginal area without any connection to the vaginal wall or cervix. This mass could be due to calcification, hematoma, or materials used in previous surgery.
Other CT findings showed a hypoplastic kidney and a 5-mm fistula between bladder trigone and 2/3 distal segment of the vagina, and a little amount of urine was detected in the vagina.
Cystoscopy and vaginoscopy were attempted in operation room by a pelvic floor disorders specialists, after general anesthesia, and in lithotomy position. Methylene blue was injected into the bladder wall and the tract to the uterine cavity was seen. There was a fistula in the bladder below the urethra. A stony mass with a diameter of 7 cm was seen in the distal segment of vaginal cavity. The stone was quite rigid and could not be removed from the vagina.
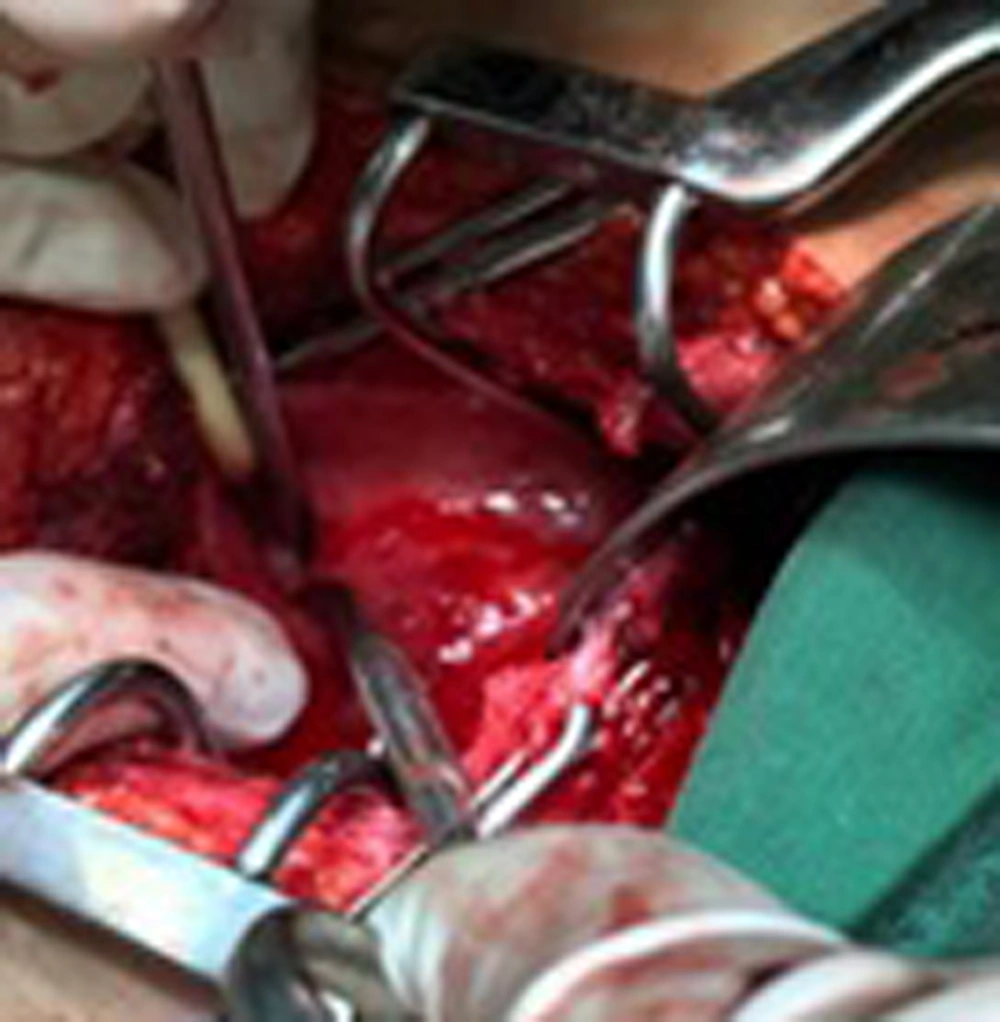
Finally, we planned open surgery technique. The patient underwent laparotomy by an expert urologist. The lower segment of the bladder (vesical neck) was dissected and removed from the anterior region of the vagina. The anterior region of the vagina was dissected. The 7-cm stone was hardly crushed and removed by washing. After opening the anterior wall of bladder, a 1-cm fistula was observed.
After excision of the fistula and mobilization of the contiguous area of the bladder and vaginal wall, a three-layer closure was performed. Superapobic catheter was inserted for 14 days and transurethral was inserted for 21 days after surgery.
Systemic antibiotics like cefazolin and metronidazole were administered after surgery. On the fifth postoperative day, the patient became febrile and cefazolin was changed to imipenem and vancomycin. The ultrasound was performed again and the result was a 73 × 41-mm collection suggesting a possible hematoma, which was evacuated by an expert sonographer, and after four days, fever was discontinued.
In the macroscopic view of the foreign body extracted from the vagina, a stony mass was seen that, after crushing inside it, a marble was seen. In the pathology study, some stones with a total diameter of 9 × 7 × 3 cm were observed.
3. Discussion
The etiology of VVF may be congenital or acquired. VVF has many causes like radiation, malignancy, obstetric disorders, and surgical procedure. The most common cause of VVF is obstructed labor (4). Foreign body is the least common cause of VVF, which is reported in less than 10% of girls with genitourinary disorders.
In most countries, more than 90% of fistulae are of obstetric etiology caused by impacted fetal head. Generally, fistulae occur between the seventh and twelfth days after gynecologic surgery (5). Foreign bodies can enter the vagina in various forms like accidently inserted by traumatic injury or without injury. Vaginal foreign bodies are usually small in size like batteries, small clamps, pins and staples (6). Foreign body can cause ulceration and perforation in the vaginal wall, thus, cause VVF and vaginal stenosis because of scarring and adhesion. It can cause peritonitis after perforation or even complete obstruction of the vagina (7). VVF diagnostic procedures include hysterosalpingography, cystoscopy, cystography, magnetic resonance imaging (MRI) and CT scan (8). Also, high level of creatinine in vaginal discharge can confirm urinary leakage. One of the main urinary symptoms in VVF is urinary incontinence (9), the other common symptoms are urinary tract infections and vaginal leakage of urine (10). Treatment options of VVF are VARIED depending on the case. Surgery is the main method of treating VVF. The most common approaches for vaginal surgery are transperitoneal, transvesical and laparoscopic procedures. Disappearance of vaginal leakage is the sign of effective and successful treatment.
In summary, gynecological complaints in most girls and adolescents with vaginal foreign body are foul smelling and blood-tinged vaginal discharge. According to our case, foreign body in the long-term causes tissue necrosis and formation of fistula that cause urinary incontinence. In this patient, the continuous leakage of urine from the fistula caused the formation of a large stone in the vagina.