1. Background
Ureteropelvic junction obstruction (UPJO) is a common congenital anomaly in children. The incidence of UPJO is reported about 5 per 100000 infants annually. In some cases, patients with congenital UPJO do not require surgery. However, in some cases, they may need surgical interventions. The clinical manifestation of UPJO depends on the patient’s age at the time of diagnosis. Recent advances and skill improvements in fetal ultrasound studies (US) led to early diagnosis of this disease prenatally. Nevertheless, the definitive diagnosis could be made after birth by further imaging and isotope scans (1).
Newborns with UPJO may be asymptomatic, however most frequent symptoms of UPJO among newborns are vomiting and pain. Hematuria and urinary tract infections (UTI) are also likely to be observed in patients with UPJO. Indications for surgical intervention in patients with UPJO include obstruction-related symptoms, impaired renal function, progressive deterioration of ipsilateral renal function, developing renal stones, infections, and hypertension (2, 3).
Treatment of UPJO focuses on relieving symptoms and maintaining the function of kidneys within normal limits. In most cases, pyeloplasty is the method of choice to treat patients with UPJO applied by Treudelem in 1886 for the first time. Although, different methods are proposed to treat UPJO, dismembered pyeloplasty remains the most popular surgical technique for years (4). Surgical pyeloplasty technique is improved during recent decades especially in the era of minimally invasive approach. Surgical pyeloplasty may be performed in open, laparoscopic-assisted, laparoscopic, or robotic-assisted surgeries.
Conventional open pyeloplasty is conducted with a flank incision, while the endoscopic approach could be performed via transperitoneal or retroperitoneal approach the same as robotic-assisted pyeloplasty (5). Endoscopic pyeloplasty is considered as a complex minimally invasive surgery (MIS) that needs advanced laparoscopic skills and fine instruments. Although endoscopic pyeloplasty gains worldwide popularity recently, it is not applicable in many centers yet due to equipment and skill limitations. Laparoscopic-assisted pyeloplasty could be the first step towards MIS approach to UPJO applicable with limited endoscopic skills and instruments.
The current study aimed at comparing the results of laparoscopic-assisted extracorporeal and open pyeloplasty in infants with UPJO.
2. Methods
The current non-randomized, controlled, clinical trial (NRCT) was conducted on a population of neonates and infants with UPJO referred to the Department of Pediatric Surgery and Urology of Dr. Sheikh Children’s Hospital with an indication for surgical intervention. Sixty infants diagnosed with UPJO were enrolled in the current study. The known advantages and disadvantages of each method were explained to parents and they were also given consultation considering the age and anatomy, and severity of symptoms.
All the children enrolled in the current study were younger than six years old. The exclusion criteria were dyspepsia, gastroesophageal reflux disease (GERD), any history of ipsilateral UPJO surgery, anatomical abnormalities such as ectopic or duplicated ureter, or any other urinary tract anomalies, general contraindications for MIS such as underlying diseases such as coagulopathy, any history of previous abdominal surgery, abdominal diseases, and interventions.
The current study was designed to evaluate 30 patients with UPJO in each group treated with either laparoscopic-assisted extracorporeal pyeloplasty or open pyeloplasty. They were non-randomly located in each of the two groups regarding the parents’ preference and considering the exclusion criteria.
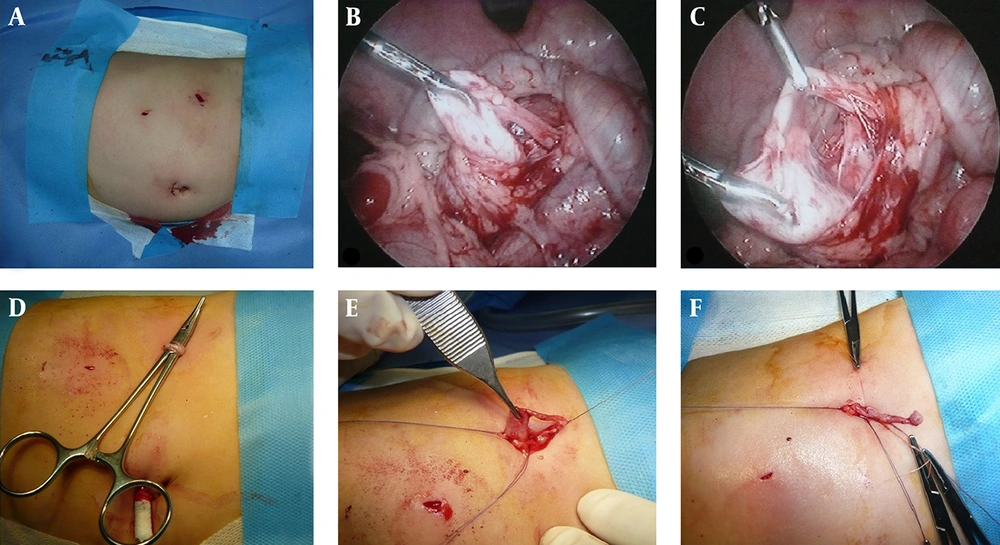
Open pyeloplasty was performed under general anesthesia via a flank incision. The surgery was performed by an expert surgeon following the standard discipline of open pyeloplasty. In laparoscopic transperitoneal approach, the patient was placed in 30 degree angle tilted to the right or left according to the involved kidney. A 5 mm port was introduced through the umbilicus for camera and gas insufflation. Two 3 mm stab wounds were created in the upper and lower parts of the right upper quadrant to insert the instruments in a port-less fashion. The exact place of these incisions were created based on the location of the UPJ. The pressure of the insufflated CO2 should be maintained at approximately 7 to 10 mmHg. The left pelvis was usually visualized and mobilized through the colon mesentery, while it might be required to mobilize the right colon before accessing the right pelvis. The urine inside the dilated pelvis was aspirated for better mobilization. Then, by the dilation of one of the stab wounds, which was closer to the ureteropelvic junction and deflation of the CO2 from the abdominal cavity, the ureteropelvic junction was pulled out of the abdominal cavity and pyeloplast was performed simply over a JJ stent extracoporeally. Due to the thin abdominal wall and high elasticity of the body organs in children, this procedure was performed without any difficulty in all cases (Figure 1).
After anastomosis, the renal pelvis was pushed back into normal anatomic position, gas insufflation was resumed and the intra-abdominal space was thoroughly observed in order to reconfirm the anatomic arrangement of UPJ and also to detect any possible problems such as bleeding. Finally, the laparoscopic instruments were removed under direct vision and the abdominal cavity was deflated; fascia was closed in port sites, and the operation was completed. Ureteral JJ stent was used in both groups of laparoscopic-assisted extracorporeal pyeloplasty and open pyeloplasty.
On the first day after surgery, plain abdominal radiography was conducted in order to demonstrate the correct position of the JJ stent. Foley catheter, which was inserted before the operation in both groups, was removed one day before discharge. Furthermore, the JJ catheter was removed within the 3rd or 4th week after the operation. The patients were followed up for at least six months and intra- and post-operative findings in clinical visits and imaging were recorded, evaluated, and compared between the two groups.
3. Results
Sixty children with UPJO underwent surgery through two major surgical methods of laparoscopic-assisted extracorporeal and conventional open pyeloplasty. The study was conducted with 30 patients in each group. Two patients in the laparoscopic-assisted group were converted to open surgery due to bleeding that excluded. Two patients in open group missed the follow-up and did not show up for a post-operative scan; 73.2% of the children were male and 26.8% were female. The comparison of gender distribution in the two groups revealed no significant difference (Table 1).
| Laparoscopic-Assisted Extracorporal Pyeloplasty | Open Pyeloplasty | P Value | |
|---|---|---|---|
| Gender (M/F) | 21/7 | 20/8 | 0.745 |
| Age | 1.16 ± 0.34 | 3.27 ± 0.41 | 0.098 |
| Pre-operative Anteroposterior pelvic diameter (mm) | 25.21 ± 4.76 | 25.79 ± 6.11 | 0.521 |
| Post-operative Anteroposterior pelvic diameter (mm) | 12.89 ± 7.38 | 10.71 ± 5.43 | 0.318 |
| Duration of surgery (min) | 78.17 ± 2.96 | 70.88 ± 1.46 | 0.321 |
| Hospitalization (d) | 2.93 ± 0.12 | 4.1 ± 0.23 | < 0.05 |
| Time to oral diet (h) | 6.6 ± 0.102 | 6.96 ± 0.21 | 0.425 |
| Normal excretion in isotope scan (%) | 92.8 | 96.4 | 0.408 |
The mean age of the patients was 2.18 ± 0.23 years. Mean operation and hospitalization time among all patients were 79.84 ± 2.75 minutes and 3.41 ± 0.4 days, respectively. Mean time to oral diet tolerance after surgery was 6.78 ± 0.107 hours and comparing the age of patients in the two study group did not show significant differences. Mean hospitalization time was significantly longer in the cases undergoing open surgery, while operation time and time to oral diet were almost the same in both groups.
Among all the patients undergoing surgery for UPJO, 10 (17.86%) had a history of another surgery as well where inguinal hernia repair was the most common operation reported in three (5.35%) patients. In addition, UPJO was operated on both sides in two (3.57%) patients that both underwent laparoscopic-assisted extracorporeal pyeloplasty.
All patients were evaluated by ultrasound study before surgical intervention and also one month after surgery and before JJ catheter removal.
Mean anteroposterior pelvic diameter before and after the operation among all cases were 25.5 ± 1.34 mm and 12.3 ± 5.97 mm, respectively. Comparison of the pelvic anteroposterior diameter before and after the operation indicated a significant reduction after the operation (P = 0.002). Comparison in both groups separately also revealed significant pelvic AP diameter reduction (P < 0.05).
Kidneys function was also evaluated by a diuretic scan after JJ catheter removal that was a reflection of surgical outcome of surgical interventions. Based on the current study findings in isotope scan, no significant differences were observed regarding the patients’ response to surgery between the two groups and just two cases in laparoscopic-assisted and one case in open pyeloplasty group showed signs of obstruction in isotope scan (P = 0.636). Common postoperative complications of UPJO surgical repair such as urinary tract infection, urinoma, and gross hematuria were not observed in any of the patients during the six-month follow-up. Only one patient in the laparoscopic-assisted group and two in the open pyeloplasty group experienced pain in the flank area. The comparison of the postoperative complications of UPJO revealed no significant differences between the two groups (P = 0.408).
4. Discussion
MIS approach for UPJO repair was first introduced in adults. The first pediatric laparoscopic pyeloplasty was performed in 1995, but did not gain much popularity worldwide especially in younger children. It may be due to technical complexities, small working space, and a need for ultra-fine instruments (6). The introduction of robotic-assisted and robotic surgery with state of art, fine articulating instruments with ergonomic working, and magnification opened a new window in minimally invasive reconstructive surgery, recently (6).
Although these recent technological improvements made the procedures easier and safer, they are not accessible in all centers yet. The current study proposed a minimally invasive thinking about pediatric UPJO repair considering the anatomic specification in pediatrics.
The current study compared the method of laparoscopic-assisted pyeloplasty technique with conventional open pyeloplasty.
No significant differences were observed in the duration of surgery between the two groups; however, the hospitalization length in the patients undergoing open pyeloplasty was longer than those of the ones undergoing laparoscopic-assisted extracorporeal pyeloplasty.
Further results of the current study demonstrated that pelvic anteroposterior diameter significantly decreased after the operation. Finally, the surgical outcome of both types of the surgery indicated that therapeutic response was acceptable and almost the same among the two groups of open surgery and laparoscopic-assisted pyeloplasty. Lower AP diameter in open surgery group may be due to more extensive partial resection of renal pelvic in the cases with huge pelvic volume.
Several studies attempted to compare laparoscopic and open pyeloplasty as the treatment of choice for patients with UPJO. Umari et al. reported longer mean operative time among patients treated with laparoscopic pyeloplasty compared with open surgery (5). Several other studies also approved the significantly longer operative time of laparoscopic pyeloplasty compared with open surgery (7-10). In the current study, the mean operative time did not differ significantly between open surgery and laparoscopic-assisted approaches.
This can be explained by extracorporeal ureteropelvic anastomosis that saves the time and also facilitates the operation technique as the most challenging and time-consuming part of MIS approach is the anastomosis that requires long learning curve.
Excluding this step makes the MIS approach easier, safer, and more applicable. Decreasing the operation time will cause less gas insuflation and it's related complications such as hypothermia and hypercarbia specially in small children.
Hospital stay duration was longer in the open surgery group compared with the patients with laparoscopic-assisted pyeloplasty in the current study, while both were shorter than the findings in most reports in previous literature (5, 6), although some other articles also reported almost the same hospital stay for their patients (7-11).
In the current study, the hospital stay was longer among patients that underwent open pyeloplasty. This may be justified with more aggressive and painful intervention, which needs more sedative and narcotics. Moreover, the duration of sedation and dose of sedatives were higher in the patients of open surgery compared with the patients undergoing laparoscopy according to the study by Bonnard et al. (7).
The rate of postoperative complications in the current study was lower than that of Umari report on MIS approach that may be due to safe and easy extracorporeal anastomosis (5).
Some other authors such as Tong and Caione et al. also approved the advantages of laparoscopic pyeloplasty for UPJO repair over conventional open approach (10, 12).
In terms of the complication rate and other findings, Wu et al. recommended open surgery as the standard treatment of UPJO, which was inconsistent with the findings of our study (8). Our results revealed that none of the applied methods were preferred to the other in terms of result and complications. However, inconsistently, pain and hospitalization length were lower in patients with open pyeloplasty than those of the ones undergoing laparoscopic pyeloplasty in the study by Ravish et al. (13).
4.1. Conclusion
Several advantages of laparoscopic UPJO repair are proved in literature such as better cosmetic results, and less pain and hospital stay; but the complexity of laparoscopic ureteropelvic anastomosis that demanded advanced surgical skills and fine instruments made it time-consuming and less applicable widely. Laparoscopic-assisted pyeloplasty as an MIS is easier and more applicable and showed acceptable results in the current study. The current study suggested this approach as the first step toward MIS for patients with UPJO.