1. Background
Protein-energy malnutrition (PEM) is linked to increased the morbidity and mortality, which is common in patients with end-stage renal disease (ESRD) on maintenance hemodialysis (HD) therapy (1, 2). PEM leads to reduction in quality of life and increases the hospital cost following the prolonged hospitalization due to infection, delayed wound healing, respiratory muscle mass losses and excessive loss of nutrients through the feces (3, 4). There are several factors which can contribute to malnutrition, including inadequate food intake, anorexia, altered taste sensation, emotional distress, poor diet, comorbid disease and increased metabolism rate owing to inflammation (5). Furthermore, atherosclerosis together with inflammation and also malnutrition affect hemodialysis patients (6, 7). Some predictors of malnutrition have been identified, the ones such as age > 65, male sex, time on dialysis and duration of dialysis (8). Low body mass index (BMI), the marker of malnutrition, is another predictor of poor survival in hemodialysis patients (9). Although the malnutrition is common among HD patients, it is ignored in many specially for some specific simple methods for nutritional evaluation that have a favorable effect on patient situation (5). Nutritional support via care team can improve nutritional status especially in severely malnourished patients (10). In this way, the malnutrition can be estimated by employing a quantitative scoring method and also a subjective global evaluation-dialysis, which is practical and reliable in this section and is the only screening tool suggested by the (ASPEN) American Society for Parenteral and Enteral Nutrition (11).
Thus, the evaluation of nutritional state is an important aspect of the HD patient treatment control. Correspondingly, the evaluation process determination of demographic and socioeconomic main parameters may contribute in distinguishing the high risk rate of patients in order to deliver appropriate care.
2. Objectives
In this study, we tried to evaluated the nutritional status of hemodialysis patients in Razi hospital in Rasht, Iran and determine the demographic and socio-economic risk factors of malnutrition.
3. Methods
This cross-sectional study was carried out on 312 patients, aged 18 or older, and admitted for hemodialysis in Razi hospital in Rasht, Iran. We used convenience sampling method to recruit participants. The following inclusion criteria were considered: (1) history of hemodialysis for at least 6 months, at least up to 3 times/week, (2) no hospitalization, (3) no history of parenteral or enteral nutrition.
The main variable was nutritional status, assessed with modified subjective global assessment (SGA) scores (12). Relatively, the altered subjective global assessment (SGA) marks, identified by medical history on seven main topics and also the clinical qualification for four other categories was the remarkably quantitative scoring system including seven elements with a total score ranging from 7 to 35 (7 - 13: normal), (14 - 23: mild to moderately malnourished) and (24 - 35: severely malnourished). The history section of this questionnaire includes five parts: weight/weight modification; dietary intake; main gastrointestinal symptoms; functional capacity; and disease situation morbidities as a related issue to nutritional status. Relative to weight/weight alteration, the patient’s weight loss was recorded along with the current weight from the preceding six months. Additionally, information regarding weight assessment for the SGA was obtained from the patient’s medical history. Other main information was required for the SGA which was gained from the patient’s clinical record. The second part was the physical examination. The physical examination comprises an assessment of the patient focusing on muscle wasting as well as the edema. We did not consider edema or ascites in this section. Other main areas including the eye, and around the triceps and biceps muscles were investigated in order to identify the subcutaneous fat loss. Muscle wasting was evaluated by considering the temporalis muscle, prominence of the clavicles, the contour of the shoulders and also the visibility of the scapula, interosseous muscle between the thumb and forefinger, and the gastrocnemius muscle. Fat loss or muscle wasting are expressed as severe (score: 5), average (score: 3) and unchanged (score: 1). The comorbidities related to malnutrition were evaluated by Charlson comorbidity index (13, 14). The body mass index (BMI) was obtained by using a DS200, scale with an accuracy of 0.5 kg. The researcher was educated on how to measure the HDP with the 7-point SGA as well as using the body fat calipers. Results are presented as mean ± SD and frequency (percentile). P value < 0.05 was determined to be significant. Notably, the logistic regression model was used for assessing probable predicting factors. Variables with a P value less than 0.2 were chosen as a possible factor. Enter method of logistic regression was used for analysis. In this study SPSS version 22 (SPSS, Inc., Chicago, USA) was used for analysis of data.
3.1. Ethical Considerations
This study was reviewed and approved by the Ethical Committee of Guilan University of Medical Sciences (number EP. 3.132.3091). Written informed consents were obtained from all the patients.
4. Results
A total of 312 patients (130 female and 182 male), aged 27 - 86 years (mean age 50.64 ± 13), completed this study. Most of them were married (82.7%); low-income (63.1%); literate (63.8%) and employed (52.2%). Demographic characteristics of the samples are summarized in Table 1.
| Socio-Demographics | N = 312 | Well Nourished (N = 62) a | Mildly to Moderately Malnourished (N = 203)a | Severely Malnourished (N = 47) a | P Value |
|---|---|---|---|---|---|
| Gender | 0.24 | ||||
| Female | 130 | 20 (15.4) | 89 (68.5) | 21 (16.2) | |
| Male | 182 | 42 (23.1) | 114 (62.6) | 26 (14.3) | |
| Age, y | 0.00 | ||||
| < 50 | 172 | 44 (25.6) | 117 (68) | 11 (6.4) | |
| ≥ 50 | 140 | 18 (12.9) | 86 (61.4) | 36 (25.7) | |
| Marital status | 0.00 | ||||
| Single | 13 | 6 (46.2) | 7 (53.8) | 0 (0) | |
| Married | 258 | 53 (20.5) | 172 (66.7) | 33 (12.8) | |
| Divorced | 41 | 3 (7.3) | 24 (58.5) | 14 (34.1) | |
| Education | 0.00 | ||||
| Illiterate | 113 | 10 (8.8) | 74 (65.5) | 29 (25.7) | |
| Below diploma | 108 | 18 (16.7) | 78 (72.2) | 12 (11.1) | |
| Diploma and upper | 91 | 34 (37.4) | 51 (56) | 6 (6.6) | |
| Economic situation | 0.35 | ||||
| Low income | 197 | 37 (18.8) | 132 (67) | 28 (14.2) | |
| Average income and high income | 115 | 25 (21.7) | 71 (61.7) | 19 (16.5) | |
| Employment status | 0.001 | ||||
| Employee | 7 | 5 (71.4) | 2 (28.6) | 0 ( 0 ) | |
| Retired | 114 | 26 (22.8) | 74 (64.9) | 14 (12.3) | |
| Worker | 87 | 17 (19.5) | 56 (64.4) | 14 (16.1) | |
| Unemployed | 104 | 14 (13.5) | 71 (68.3) | 19 (18.3) | |
| Number of family members | 0.00 | ||||
| < 3 | 127 | 31 (24.4) | 83 (65.4) | 13 (10.2) | |
| 3 - 5 | 160 | 29 (18.1) | 109 (68.1) | 22 (13.8) | |
| > 5 | 25 | 2 (8) | 11 (44) | 12 (48) | |
| Habitation | 0.07 | ||||
| Urban | 207 | 48 (23.2) | 132 (63.8) | 27 (13) | |
| Rural | 105 | 14 (13.3) | 71 (67.6) | 20 (19) | |
| Housing conditions | 0.02 | ||||
| Leased | 89 | 25 (28.1) | 56 (62.9) | 8 (9) | |
| Private | 223 | 37 (16.6) | 147 (65.9) | 39 (17.5) | |
| Living conditions | 0.000 | ||||
| Alone | 18 | 5 (27.8) | 11 (61.1) | 2 (11.1) | |
| With spouse | 73 | 18 (24.7) | 48 (65.8) | 7 (9.6) | |
| With his wife and children | 221 | 39 (17.6) | 144 (65.2) | 38 (17.2) | |
| Spouse Education | 0.03 | ||||
| Illiterate | 120 | 19 (15.8) | 80 (66.7) | 21 (17.5) | |
| Below diploma | 116 | 22 (19) | 82 (70.7) | 12 (10.3) | |
| Diploma and upper | 48 | 16 (33.3) | 30 (62.5) | 2 (4.2) | |
| Spouse’s employment status | 0.93 | ||||
| Employed | 3 | 1 (33.3) | 2 (66.7) | 0 ( 0 ) | |
| Retired | 93 | 16 (17.2) | 66 (71) | 11 (11.8) | |
| Worker | 36 | 5 (13.9) | 26 (72.2) | 5 (13.9) | |
| Unemployed | 152 | 35 (23) | 98 (64.5) | 19 (12.5) | |
| Membership in the community | 0.18 | ||||
| Yes | 249 | 47 (18.9) | 168 (67.5) | 34 (13.7) | |
| No | 63 | 15 (23.8) | 35 (55.6) | 13 (20.6) | |
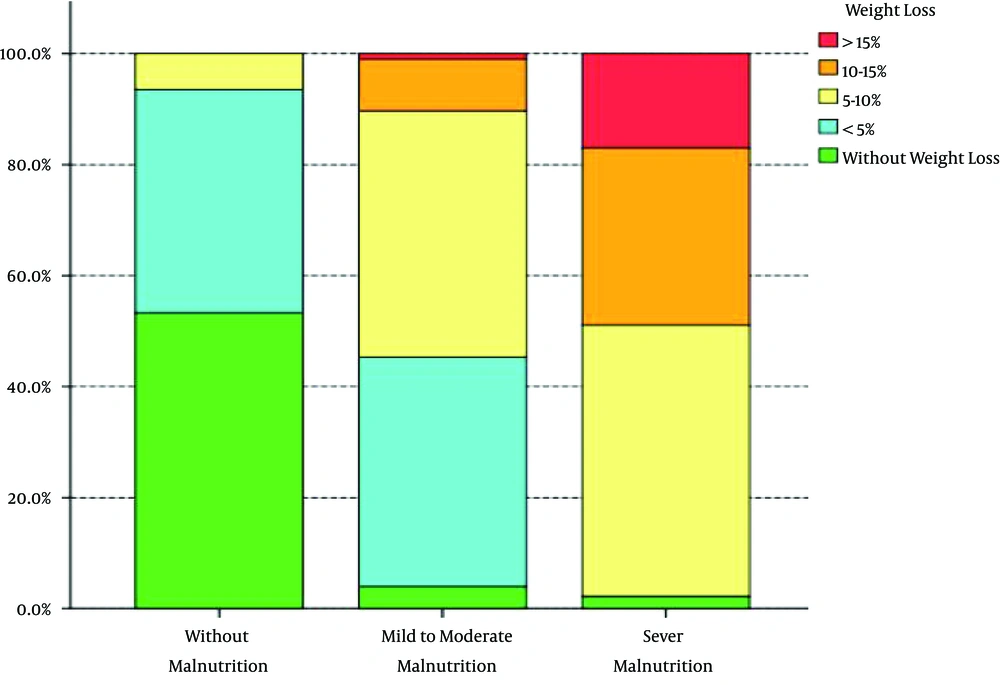
| Weight loss, % | 0.000 | ||||
| No | 42 | 33 (78.6) | 8 (19) | 1 (2.4) | |
| < 5 | 109 | 25 (22.9) | 84 (77.1) | 0 (0) | |
| 5 - 10 | 117 | 4 (3.4) | 90 (76.9) | 23 (19.7) | |
| 10 - 15 | 34 | 0 (0) | 19 (55.9) | 15 (44.1) | |
| > 15 | 10 | 0 (0) | 2 (20) | 8 (80) | |
| History of transplantation | 0.45 | ||||
| Yes | 32 | 9 (28.1) | 19 (59.4) | 4 (12.5) | |
| No | 280 | 53 (18.9) | 184 (65.7) | 43 (15.4) | |
| Dialysis/week | 0.07 | ||||
| 2 | 37 | 8 (21.6) | 19 (51.4) | 10 (27) | |
| 3 | 275 | 54 (19.6) | 184 (66.9) | 37 (13.5) | |
| Duration of disease, y | 0.34 | ||||
| < 1 year | 24 | 7 (29.2) | 16 (66.7) | 1 (4.2) | |
| > 1 year | 288 | 55 (19.1) | 187 (64.9) | 46 (16) | |
| Duration of dialysis, y | 0.44 | ||||
| < 5 | 188 | 36 (19.1) | 123 (65.4) | 29 (15.4) | |
| 5 - 10 | 96 | 22 (22.9) | 63 (65.6) | 11 (11.5) | |
| > 10 | 28 | 4 (14.3) | 17 (60.7) | 7 (25) |
a Values are presented as No. (%).
The rates of mild to moderate and severe malnutrition were 65.1% and 15% respectively. The rest (19.9%) had normal nutritional status. There is a significant correlation between weight change and nutritional status (P value = 0.000). As shown in Figure 1, the severe weight loss was associated with severe malnutrition.
After control of confounding factors, illiterate patients had a significantly higher risk of malnutrition. Low educational level can also increase the risk of malnutrition (Table 2).
| Variables, Education | Nutritional Status | COR (95%CI) | P Value | ||
|---|---|---|---|---|---|
| Normal | Malnutrition | Total, No. | |||
| Diploma and above | 34 (37.4) | 57 (62.6) | 91 | 1 | |
| Under diploma | 18 (16.7) | 90 (83.3) | 108 | 3.07 (1.10 - 8.52) | 0.031 |
| Illiterate | 10 (8.8) | 103 (91.2) | 113 | 8.14 (1.8 - 36.89) | 0.006 |
aValues are expressed as No. (%) unless otherwise indicated.
5. Discussion
Hemodialysis patients are always at risk of protein-energy malnutrition (15). In this study, the majority of patients had some degree of malnutrition, even though in some studies, the incidence of malnutrition is underreported (16).
We found that malnutrition is correlated with some demographic characteristics and socio-economic status. Women, the elderly, the unemployed, the widowed, the divorced, the illiterate and those living in large families are more susceptible to malnutrition similar to the previous studies (17, 18). This is perhaps partly because of the more psychological and economical tensions and less supportive initiatives in these patients (19, 20). Contrary to our study, it has been shown that the male sex and the younger age were the predictive factors of malnutrition (21). Duration and frequency of dialysis did not have impact on the nutritional status significantly; however, the results of other studies are inconsistent (22). Nevertheless, high-quality regular dialysis can improve the nutritional status of patients (23). We found that illiteracy can increase the risk of malnutrition, particularly severe malnutrition. Reversed relationship has been found between the level of education and malnutrition, the higher the education, the greater the risk of malnutrition (24), but it seems that higher education can improve the social and economic status and access to health services to reduce the risk of malnutrition. Higher education creates a greater ability to deal with physical and mental problems that can lead to the improvement of nutritional status. Despite the fact that none of the patients in this study was the member of the association of kidney patient support, it seems that community support by providing training and financial assistance for patients can help to improve nutritional status (25). Educated spouses with good economic situation can be a protective factor in the prevention of malnutrition as well (26).
In this study, the weightiest change was seen in malnourishment. The inflammation may often induce weight loss or a condition of malnutrition (27). As previous studies have shown, there is a remarkably significant negative correlation between altered Subjective Global Assessment-Dialysis Malnutrition Score and also the anthropometric evaluation such as triceps skin fold thickness, mid arm circumference, and mid arm muscle circumferences (28). It is well worth noting that decreased fat mass is correlated with cardio-vascular diseases CVD and other markers of malnutrition (22).
5.1. Conclusions
In summary, more attention must be paid to high risk patients with regard to demographic and socio-economic status in treatment programs.