1. Introduction
Arthrogryposis-renal dysfunction-cholestasis (ARC) syndrome is a rare disorder that affects several organs and is fatal. The ARC is caused by an autosomal recessive mutation in the VPS33B gene in the chromosome 15q26.1 (1). Several clinical manifestations include cognitive impairment, ichthyosis, hypothyroidism, congenital heart disease, cerebrovascular disorder, neonatal deafness, diarrhea, and frequent fever (2-4).
In this case report, our patient was a 45-day-old infant who had tachypnea, direct hyperbilirubinemia (cholestasis), and severe dehydration, with pelvic joint deformity (DDH), bilateral club foot, and renal tubular acidosis who was treated with ARC syndrome diagnosis.
2. Case Presentation
A 45-days-old infant who referred to our hospital with jaundice and tachypnea complaints. According to his mother’s claims, he had jaundice from the second week, which was exacerbated from a week ago. Shortly after birth, he developed jaundice, diarrhea, and failure to thrive. He was ill and had poor feeding. Owing to lethargy and severe dehydration, he was admitted in the ICU.
This male infant was born at term by Cesarean section. Mother’s pregnancy was normal. His birth weight was 3,190 g. According to the mother’s explanations, she had tachypnea from a few days after birth and he was admitted and examined for sepsis recurrently. He was dehydrated and the oral mucosa was very dry. Her fontanel was depressed. He had a mild murmur in the heart examination. During the lung examination, he had respiratory distress and its respiratory rate was 74 and the lung was clear.
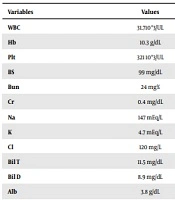
Also, he had multiple joint contractures and had a bilateral dislocation in the lower extremity examination of the hip and bilateral talipes calcaneovalgus. His skin was icteric and wrinkled, and the skin turgor had increased and on the whole, the skin was spreading (ichthyosis) and he had muscle atrophy. At the neurological examination of reflexes (moro, grasp, sucking) was decreased. The infant was admitted to the ICU and laboratory tests were done (Table 1).
| Variables | Values |
|---|---|
| WBC | 31.710*3/UL |
| Hb | 10.3 g/dL |
| Plt | 321 10*3/UL |
| BS | 99 mg/dL |
| Bun | 24 mg% |
| Cr | 0.4 mg/dL |
| Na | 147 mEq/L |
| K | 4.7 mEq/L |
| Cl | 120 mg/L |
| Bil T | 11.5 mg/dL |
| Bil D | 8.9 mg/dL |
| Alb | 3.8 g/dL |
| T pr | 5.9 g/dL |
| TSH | 14.5 mic IU/L |
| FT4 | 20.6 pmol/L |
| AFP | 12 ng/mL |
| Gamma GT | 38 IU/L |
| Lactate | 8 mg/dL |
| B/C | Neg |
| BT | 4.2 min |
| CPK | 61 U/L |
| Ca | 8.5 mg/L |
| P | 4.2 mg/L |
| Mg | 2.1 mg/L |
| Ast | 37 IU/L |
| Alt | 33 IU/L |
| TG | 180 mg/dL |
| Chol | 120 mg/dL |
| PT | 13 s |
| PTT | 37 s |
| INR | 1 |
| ESR | 11 mm |
| Vbg | pH: 7.13 → 7.44 |
| PCO2 | 39 → 36 mmHg |
| HCO3 | 12.5 → 22 mmol/L |
| U/A | pr 3+ |
| Glc | 2+ |
| SG | 1030 |
| LDH | 452 IU/L |
| CRP | Neg |
In the lab data, he had direct hyperbilirubinemia. Thyroid function test was abnormal and he had hypothyroidism. He had hyperchloremic metabolic acidosis and glycosuria with normal urea and creatinine. Liver function test was normal.
In ultrasound, the kidneys had a normal size, but their echoes had increased. The liver had normal size and echo, but the gall bladder was not seen. In the brain sonography, he had mild ventriculomegaly and corpus callosum was not seen. Sonography of hip joint show bilateral DDH grade 3. In cardiac echocardiography had mild LVH and mild PH.
The patient was treated with DW5% and Normal Saline to compensate for dehydration. Owing to acidosis, he was treated with intravenous bicarbonate. Fat-soluble vitamins were prescribed to him and treated with zinc sulfate syrup, ursobil capsule, MCT oil, and an ampoule of pantoprazole. Signs of dehydration have improved and the patient got a good weight gain. Because of the impossibility of genetic testing in our country, but based on the patient's set of symptoms, including arthrogryposes, acidosis, and cholestasis, as well as the normal gamma-GT (GGT) level; in contrast, the presence of cholestasis, and also the agenesis of corpus callosum, hypothyroidism, and ichthyosis he was treated with the diagnosis of ARC syndrome. He received supportive treatment, including Shohl's solution or bicitra for treating acidosis and fat-soluble vitamins (A, D, E, K), multivitamins, and MCT oil.
3. Discussion
From 1973, when the first report of ARC syndrome was given by Lutz-Richner and Landolt (5), this fatal disease was reported elsewhere in the world. It seems that Arthrogryposis is caused by neurogenic muscular atrophy and has different manifestations, including talipes equinovarus, talipes calcaneovalgus, radial deviation of the wrists, limb contraction, limb clubfeet, and buttock displacement (6). Renal tubular function disorder occurs in the first few days of life and sometimes two to three months later. It can also be diagnosed as renal tubular acidosis and symptoms of Fanconi syndrome, including glycosuria, proteinuria, aminoaciduria, phosphaturia, and bicarbonate wasting. Renal ultrasound is sometimes shown by nephrocalcinosis (3, 7, 8).
Direct hyperbilirubinemia with normal or elevated levels of transaminases is a feature of the ARC syndrome. On the other hand, in contrast to high bilirubin and alkaline phosphatase (ALP), they have normal levels of GGT enzyme (9, 10). Neurological symptoms, including growth retardation and hypotension, have been reported in all cases. Other manifestations were comprised of neural deafness and non-formation or hypoplasia of corpus callosum in some cases (4, 8). Most patients with ARC syndrome do not grow up well despite enough calorie intake, which is usually due to increased calorie intake as a result of frequent dehydration, sepsis or chronic diarrhea, which can be secondary to fat malabsorption. In many cases of ARC syndrome, hypernatremia, dehydration, and polyuria have been reported (8, 11).
Mild to severe ichthyosis has also been reported in many patients with ARC syndrome (7, 8, 10). In patients who were considered to be immunodeficient, this workup was normal (7). Various features related to the ARC syndrome consist of prominent occiput, posteriorly angulated, and low set ears, flattened nasal bridge, upslanting palpebral fissures, simian crease, high arched palate, beaked nose, small anterior fontanel, lax skin, low implantation of the thumb, and cryptorchidism (3, 7, 8). Abnormal platelets are found in some patients. Other symptoms of this syndrome include fractures of the femur and ribs in some patients (3, 7). In some patient with ARC syndrome hypothyroidism was also reported (3).
Congenital heart defects such as ventricular septum defects (VSD) and atrial septum defects (ASD) are sometimes seen (4, 8, 11). Most patients die in the first year of life, but some survive up to the age of three, and usually their death is due to sepsis, severe anemia, acidosis, and dehydration (8). Genetic testing was not available for the diagnosis in our country but totally, according to the patient symptoms, including arthrogryposis, cholestasis, and renal tubular acidosis, as well as other symptoms such as failure to thrive, hypothyroidism, ichthyosis, and congenital cardiac defect (small ASD). The patient was treated with the diagnosis of ARC syndrome.
3.1. Conclusions
More attention must be paid to patients with arthrogryposis-renal dysfunction-cholestasis (ARC). Also, routine serum measurements are recommended to determine the cases of this disease in its earlier stages before the start of complications.