1. Background
Primary hypertension is usually considered as a disease of adulthood, with a prevalence of 30% (1, 2). Despite the low incidence of HTN in children, its prevalence has been increasing recently. Hypertension in childhood serves as a strong predictor of hypertension in adulthood (3, 4). The diagnosis of hypertension predicts potential damage to the vasculature, heart, and other organs (5); therefore, early diagnosis of HTN is correlated with a reduced mortality rate.
Hypertension may occur as a result of vitamin D deficiency, which regulates blood pressure by balancing arterial constriction and dilation. Low vitamin D levels impair this regulation system leading to HTN and its’ resultant complications (6).
Therefore, vitamin D levels demonstrate an inverse relationship with blood pressure, which seems to play an essential role in both the development and persistence of HTN. Despite that the link between vitamin D levels and hypertension has been well documented in animal studies; however, it has not yet been fully established in numerous clinical trials (7).
Primary hypertension occurs when the balance between vasoconstriction and vasodilatation is disturbed. According to a study by Chen and colleagues, it was found that administering vitamin D to patients with primary hypertension exerted antihypertensive qualities (8).
2. Objectives
Previous research has demonstrated that low vitamin D levels lead to hypertension in some individuals, accordingly, this study aims to evaluate blood pressure levels in children suffering from vitamin D deficiency.
3. Methods
This descriptive study was conducted on 65 children under the age of 11 with vitamin D deficiency at Amirkabir Hospital, Arak, Iran. Demographic characteristics including age, sex, and height of children were documented in order to interpret blood pressure levels.
The blood pressure of children was measured by the digital blood pressure monitor citizen (REFCH-311B) after obtaining informed consent, according to the standards of blood pressure assessment in children.
A digital blood pressure monitor and a checklist for data documentation were employed to collect information. The 25-hydroxyvitamin D levels were measured as a suitable indicator of vitamin D levels in the blood.
Blood pressure percentiles were determined by age, gender and height. Blood pressure less than the 90th percentile is considered normal, blood pressure levels between the 90 - 95th percentile indicate pre-HTN, blood pressure between 95 - 99th percentile plus 5 mmHg indicates stage I HTN, and blood pressure greater than the 99th percentile plus 5 mmHg is considered as stage II HTN (9).
The inclusion criteria included all individuals under the age of 11 with 25-hydroxyvitamin D levels less than 20 ng/dL. Children suffering from underlying illnesses and consumers of hypertensive drugs were excluded.
Eventually, collected data was statistically analyzed via the SPSS-23 software, independent sample t-test, chi-square, one way ANOVA, and Pearson correlation tests.
4. Results
In this study, 65 children were enrolled consisting of 32 boys and 33 girls. The mean age of these children was 6.01 ± 2.32 years old. More detailed information on their age, height, weight, and BMI are summarized in Table 1. In the study, the systolic and diastolic blood pressure in 62 children (95.4% of all) were in normal range (Table 1).
| Variable | Status |
|---|---|
| Gender | |
| Male | 32 (49.2) |
| Female | 33 (50.8) |
| Age | 6.01 ± 2.32 |
| Height | 114.66 ± 16.82 |
| Weight | 21.17 ± 7.30 |
| BMI | 16 ± 2.84 |
| Systolic blood pressure | |
| Normal | 62 (95.4) |
| Pre-HTN | 2 (3.1) |
| HTN grade I | 1 (1.5) |
| Diastolic blood pressure | |
| Normal | 62 (95.4) |
| Pre-HTN | 3 (4.6) |
General Characteristics of the Childrena
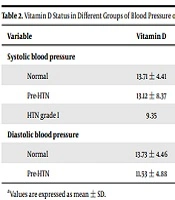
Statistical analysis demonstrated no significant correlation between vitamin D levels and systolic blood pressure, diastolic blood pressure, height, weight, and BMI in children; a level of 0.05 was considered significant. More detailed information in this area is summarized in Tables 2 and 3.
| Variable | Vitamin D | P Value |
|---|---|---|
| Systolic blood pressure | 0.624 | |
| Normal | 13.71 ± 4.41 | |
| Pre-HTN | 13.12 ± 8.37 | |
| HTN grade I | 9.35 | |
| Diastolic blood pressure | 0.409 | |
| Normal | 13.73 ± 4.46 | |
| Pre-HTN | 11.53 ± 4.88 |
Vitamin D Status in Different Groups of Blood Pressure of the Childrena
| Variable | P Value | Pearson Correlation |
|---|---|---|
| Height | 0.416 | -0.103 |
| Weight | 0.425 | -0.106 |
| BMI | 0.474 | -0.095 |
Relationship Between Vitamin D Status and Height, Weight and BMI of the Children
5. Discussion
This recent study was conducted to determine the blood pressure status in children with vitamin D deficiency in Amir Kabir Hospital, Arak, Iran. A total of 65 children under the age of 11, with vitamin D deficiency, were enrolled and their blood pressure was measured according to standards of BP assessment. The results obtained demonstrated no significant difference between vitamin D and blood pressure levels despite the diversity of vitamin D levels in various systolic and diastolic BP conditions.
Arora and colleagues, found vitamin D supplements not effective in reducing blood pressure in patients with vitamin D deficiency and stage I HTN (10), which was broadly compatible with the results of this recent study; in both studies, no significant correlation was observed between vitamin D and blood pressure levels.
Kunutsor and colleagues reported a significant reverse relationship between 25-hydroxyvitamin D and the risk of HTN in patients, which was not in line with the results of our study. They also found a 12% decrease in the risk of HTN with 10 ng/mL increase in the levels of 25-hydroxyvitamin D (11).
In another study conducted by Witham and colleagues, a 6-month trial of oral vitamin D supplementation was not found effective in reducing blood pressure levels in patients suffering from resistant HTN and decreased cardiac mass (12).
Vimaleswaran et al. found that an increase in 25 (OH) vitamin D concentration was associated with a decrease in systolic blood pressure and reduced the risk of hypertension. Generally, it was concluded that increased plasma concentrations of 25 (OH) vitamin D, decreased the risk of HTN (13).
Another study by Loloei and colleagues concluded that the prevalence of vitamin D deficiency was very high in individuals suffering from hypertension. In addition, the treatment of vitamin D deficiency, due to its effects on hypertension, were recommended (14).
Unfortunately, various studies have demonstrated diverse results regarding vitamin D levels and blood pressure status indicating that there is still considerable uncertainty; therefore, further work needs to be done in order to establish more conclusive results regarding this topic.
This study had some limitations; the most important lies in the small sample volume. We propose that further research should be undertaken on a wider level to compare vitamin D levels with different blood pressure levels.
5.1. Conclusions
In regards to the results of this study, it seems that vitamin D levels in children is not related to the incidence of hypertension. In addition, the analysis did not reveal any significant correlation between vitamin D levels and BMI. However, the conclusions of this study cannot be conclusive in this regard.