1. Background
Nephrotic syndrome is one of the most important chronic kidney diseases in children. Steroids are the drugs of choice for the treatment of nephrotic syndrome in children. In some cases, due to the chronicity of the disease and recurrent episodes, they are used for a long time, causing complications such as severe growth disorder, obesity, cataract, osteoporosis, bone aseptic necrosis, immune system weakness, hypersensitivity, psyche, and peptic ulcer, among other complications (1, 2).
Nephrotic syndrome can be seen in children in three forms of congenital, secondary, and idiopathic based on origin (3, 4). Diseases that initially affect the kidneys and interrupt the structure, glomerular function, or both in the absence of a systemic condition may lead to the early or idiopathic nephrotic syndrome in children. Childhood nephrotic syndrome is unexplained in more than 90% of the cases while 25% of nephrotic syndrome cases are unexplained in adults (5).
On the other hand, mild to moderate micronutrient deficiency is very common in developing countries, especially in nations with high growth rates. High levels of infection in developing countries increase the importance of zinc deficiency. Zinc supplementation can reduce morbidity and mortality due to diarrhea and pneumonia and accelerate population growth in developing countries (6). The plasma level is usually normal in mild deficiency while it is less than 60 μg/dL in moderate to severe cases. Based on the evidence, the zinc level can reduce many clinical disorders, such as cirrhosis, nephrotic syndrome, and renal failure (5, 7).
2. Objectives
Therefore, due to the important of serum zinc levels in prognosis of nephrotic syndrome, the current study aimed to investigate the serum zinc levels in children with nephrotic syndrome.
3. Methods
3.1. Study Setting
A descriptive-analytical study was conducted on patients with nephrotic syndrome at the Pediatrics Clinic of Amir-Kabir hospital in Arak city, Iran.
3.2. Study Population
The study population included children with nephrotic syndrome aged 1 to 14 years from both genders who referred to Amir Kabir Hospital in Arak. A sample of 102 children with nephrotic syndrome was recruited.
3.3. Measurement
Nephrotic syndrome in children was determined based on their medical history as diagnosed by pediatric nephrology specialists. The nephrotic syndrome severity was classified into the mild, moderate, and severe categories based on diagnostic criteria and response to treatment. The serum zinc levels were also evaluated in these patients to compare with the severity of nephrotic syndrome.
3.4. Tools
A checklist was used to record the demographic and clinical characteristics including age, sex, serum zinc level, and the severity of nephrotic syndrome. The levels of zinc were determined in 2.5 cc of peripheral blood samples. As soon as possible after sampling, serum or plasma samples were centrifuged for up to 2 h in trace element-free tubes containing anticoagulant such as EDTA, until the measurement of zinc. The serum zinc concentrations were measured based on the 5-Br-PAPS method using a diagnostic kit (Biochemistry, Tehran, Iran) and expressed as mg/dL.
3.5. Ethical Considerations
Before entering the study, all children and their parents were explained about the study and they gave their informed consent and in the case with the age of under 12 years of age, the patients are enrolled in the study. The study followed the statements of the Helsinki Declaration and it was approved by the Ethics Committee of the Research Council of the Arak University of Medical Sciences (ethical code 21-171-93).
3.6. Statistical Analysis
Data were analyzed by SPSS software. Descriptive statistics were used to express the frequency of variables. Fisher’s exact test was used to evaluate the correlation between the severity of nephrotic syndrome and the serum zinc level. The P values of < 0.05 were considered significant.
4. Results
The mean age of the children was 2.6 ± 2.3 years. Moreover, 58 out of 102 (56.86%) children were male and 56 (43.14%) were female (Table 1). Based on severity, the nephrotic syndrome was severe in 23 (22.54%) children, moderate in 36 (36.23%) children, and mild in 43 (42.15%) children (Table 2).
| Variables | Values |
|---|---|
| Age, mean ± SD | 6.2 ± 3.2 |
| Gender | |
| Male | 58 (56.8) |
| Female | 44 (43.1) |
Frequency Distribution of Age and Gender Among Patients
| Nephrotic Syndrome | Frequency (%) |
|---|---|
| Severe | 23 (22.5) |
| Moderate | 36 (35.3) |
| Mild | 43 (42.2) |
Frequency Distribution of Nephrotic Syndrome Severity
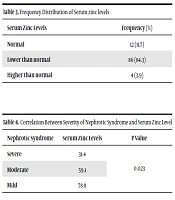
The serum zinc level was normal in 12 (11.76%) patients, lower than normal in 86 (84.3%) patients, and higher than normal in 4 (2.94%) patients (Table 3). The mean serum zinc level was 64.82 mg/dL. The serum zinc level was significantly lower in the group with severe nephrotic syndrome (48.8 ± 6.8) than in the groups with moderate (59.12 ± 5.4) and mild (78.22 ± 4.1) nephrotic syndrome (P < 0.001) (Table 4).
| Serum Zinc Levels | Frequency (%) |
|---|---|
| Normal | 12 (11.7) |
| Lower than normal | 86 (84.3) |
| Higher than normal | 4 (3.9) |
Frequency Distribution of Serum zinc levels
| Nephrotic Syndrome | Serum Zinc Levels | P Value |
|---|---|---|
| Severe | 31.4 | 0.023 |
| Moderate | 59.1 | |
| Mild | 78.8 |
Correlation Between Severity of Nephrotic Syndrome and Serum Zinc Level
5. Discussion
In the present study, although the prevalence of nephrotic syndrome was more in male children rather than in female the difference was not significant. Most patients with nephrotic syndrome had low serum zinc levels. It was also found that the serum zinc level was significantly lower in patients with severe nephrotic syndrome than in patients with mild to moderate nephrotic syndrome. Serum zinc levels had a statistically significant association with the severity of nephrotic syndrome. However, different results have been observed in previous studies, which are further addressed.
A study by McBean et al. found that the serum zinc level was significantly lower in patients with nephrotic syndrome than in a control group (P < 0.001) (8), which is consistent with the results of our survey and indicates the important role of zinc level in patients with nephrotic syndrome. Moreover, a case-report study by Yang et al. in 2011 evaluated a newborn with transient short-term nephrotic syndrome. In this study, the serum zinc level was lower than normal while it was normal in the mother. Moreover, the serum level of zinc was very low in breast milking children (9). The results obtained from the mentioned study are different from our study results possibly due to differences in the methodology of the two studies. In another study, Abrams found that more urea excretion in healthy kidneys than unhealthy kidneys, could be a sign of decreased renal reabsorption. Zinc levels in the urine may also affect kidney damage and kidney stones. Therefore, the therapeutic use of zinc may have beneficial effects on kidney stone disease (10). In addition, a study by Gurgoze and Sari concluded that chronic hemodialysis may lead to abnormal serum levels of trace elements in children with chronic renal failure. The low levels of these trace elements, especially zinc, may be associated with prognosis and symptoms in children undergoing chronic hemodialysis (11). These results are consistent with the results of the current study. Based on the results of the current study and other studies in this area, it is crucial to pay attention to the serum zinc level in patients with nephrotic syndrome.
5.1. Conclusions
The mean serum zinc level was significantly lower in patients with severe rather than in those with mild to moderate nephrotic syndrome. The correlation between the zinc level and the nephrotic syndrome severity was significant, which may have implications for improving the prognosis of patients with nephrotic syndrome.