1. Introduction
Toxoplasmosis is a very common human infection. Latent toxoplasmosis has involved approximately one-third of the entire world’s population. Latent infection reactivation can cause the development of the central nervous system (CNS) toxoplasmosis. It is often associated with the symptoms of impaired consciousness, fever, local neurological deficits, and/or headache. The treatment of immune system diseases. Long-term use of immunosuppression, and acquired human immunodeficiency (e.g. AIDS) can be challenging in the presence of neurotoxoplasmosis. Since neurotoxoplasmosis can mimic other CNS disorders, the diagnosis and management of its clinical representations become challenging, thereby necessitating regular empiric therapy (1-5). The present case was an unusual neurotoxoplasmosis in a patient with glomerulonephritis.
2. Case Presentation
The patient was a man, aged 23 years old, admitted to the hospital because of having drowsiness, fever, nausea, vomiting, and acute progressive headache in the past 24 hours.
The patient suffered from a progressive blurred vision in the right eye for 3 weeks prior to admission. He had also experienced an episode of seizure.
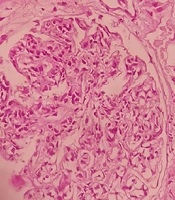
He underwent a renal biopsy for proteinuria and hematuria five months ago and received four weekly infusions of rituximab (375 mg/m2) for four doses, followed by off-label prednisolon 1 mg/kg two months before for DPG (Figure 1). Physical examination revealed the symptoms of stupors pale conjunctivae and bilateral papilledema.
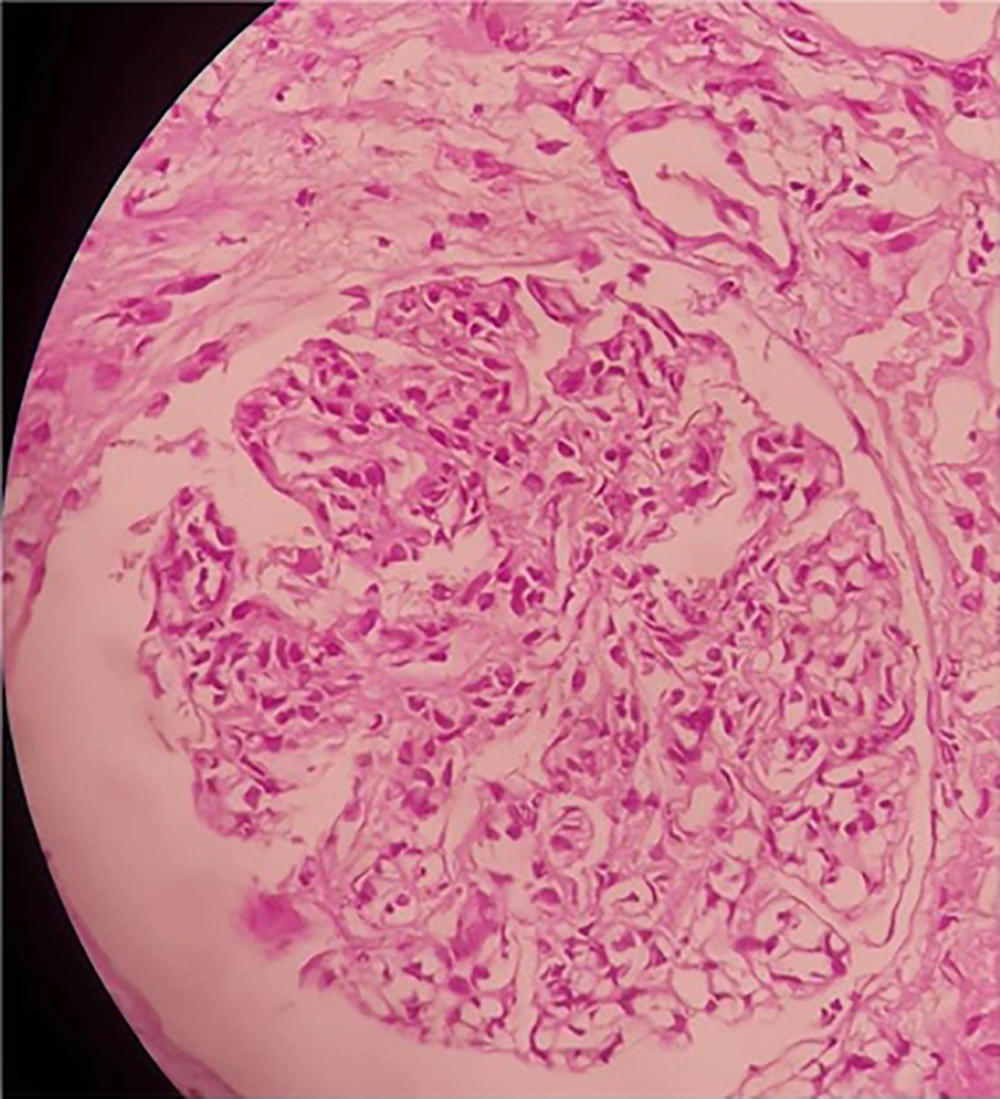
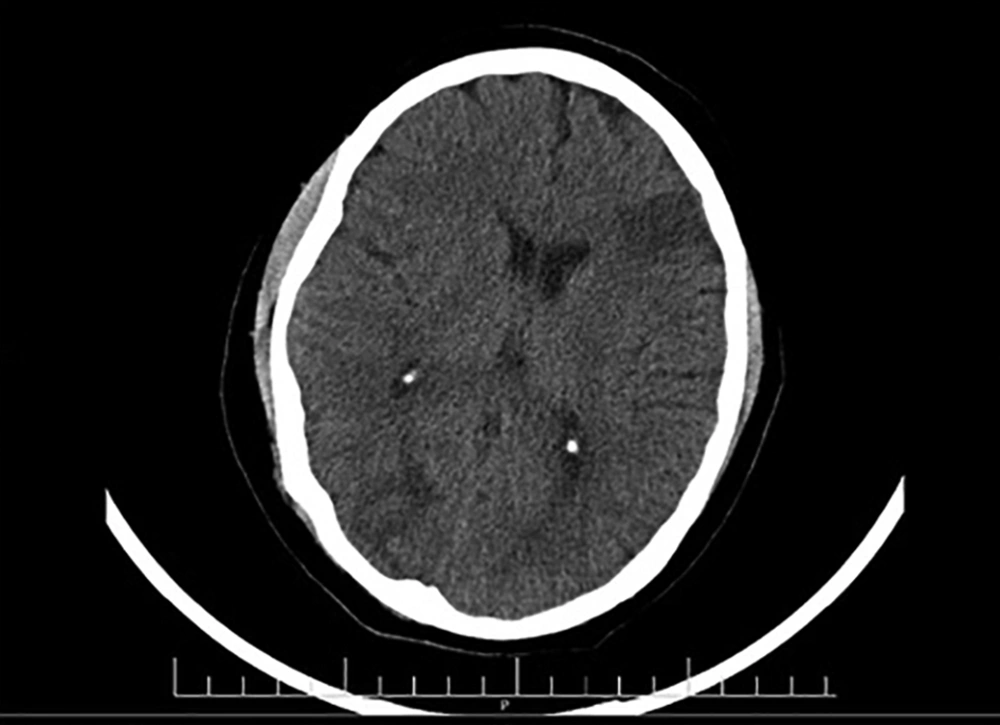
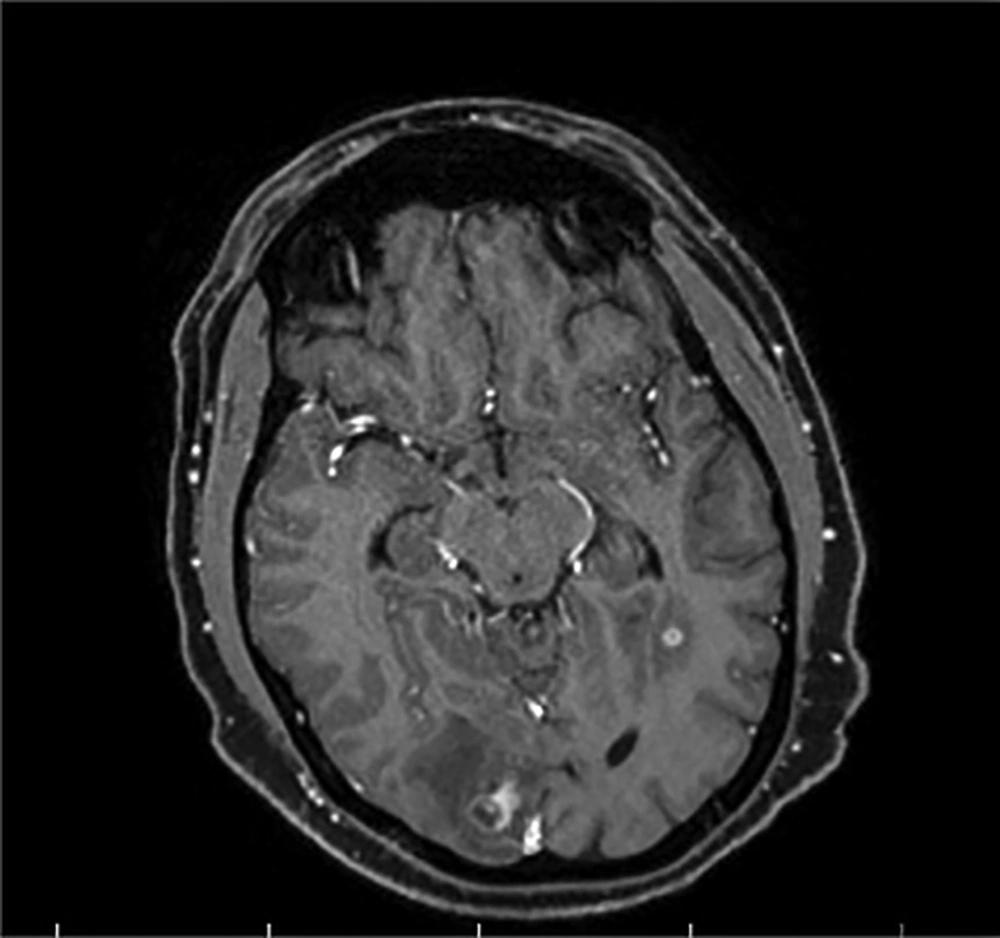
He was examined by an ophthalmologist for blurred vision and subretinal mass, optic disk swelling with hemorrhage and hypopyon, and creamy yellow exudate, as a complication of the retinal abscess, were detected. He was given an antibiotic therapy based on the CT and MRI results and the diagnosis of multiple brain abscesses (Figures 2 and 3). Due to the possibility of toxoplasma following brain and retinal abscesses, the patient received vancomycin, ceftriaxone, metronidazole, and cotrimoxazole, and the improvement of symptoms and normal state of consciousness were observed.
Brain MRI (navigation protocol; with and without GD): MRI shows multifocal vasogenic edema of the bilateral, parietal, right occipital, right temporal, left frontal lobes, and subcortical white matter lesions in both cerebellar hemispheres, indicating a multifocal abscess. No evidence of thrombosis, aneurysm, or AVM was detected in brain MRV and MRA scans.
3. Discussion
Toxoplasma gondii infection is a common disease worldwide. Acute infections usually remain asymptomatic in patients with immunocompetency. Diffuse encephalopathy with or without seizure, singular/large progressive mass lesions, and meningoencephalitis are major pathologic patterns associated with cerebral toxoplasmosis in an immunocompetent host. The demonstration of toxoplasmosis-specific antibodies in the patient's serum can be a definitive diagnosis. The brain biopsy is occasionally recommended in some cases susceptible to toxoplasmosis (1-5).
A definitive diagnosis of immunocompromised patients with CNS lesions involves the detection of a set of clinical signs (e.g., headache, neurologic symptoms, fever), one or more mass lesions by brain imaging, and toxoplasma DNA in the cerebrospinal fluid or T. gondii organisms in a biopsy specimen. In some cases, empiric treatment is administered based on a presumptive diagnosis made on the basis of the constellation of physical signs or symptoms. In such patients, response to therapy usually produces powerful support of diagnostic hypotheses (6).
With the growing prescription of rituximab for glomerulonephritis treatment, clinicians must be aware of the risk of Toxoplasma gondii encephalitis. Recent travel to highly endemic regions, contact with cats, and using undercooked meat make people susceptible to acute toxoplasmosis (7).
Before pharmacological therapy, the susceptible patients should be screened for toxoplasmosis and receive regular clinical examinations. Due to the severity of neurotoxoplasmosis and its potentially lethal mutation, empiric therapy should be started in case of neurological symptoms of unexplained origin, while other symptoms should be checked at the same time (8). The seropositive status of the patients can also be helpful helps in close monitoring and starting early treatment.
3.1. Conclusion
Cerebral toxoplasmosis should be considered as a differential diagnosis for patients with neurological symptoms after rituximab therapy .Due to the severity of neurotoxoplasmosis and its potentially lethal condition, empiric therapy should be started in case of neurological symptoms of unexplained origin. The differential diagnosis of patients with neurological symptoms after rituximab therapy should consider the risk of cerebral toxoplasmosis. Due to the severity of neurotoxoplasmosis and its potentially lethal mutation, empiric therapy should be started in case of neurological symptoms of unexplained origin.