1. Context
Most pancreatic tumors are epithelial cancers. Adenocarcinoma is the most common malignancy in this organ. Stromal pancreatic tumors are usually GIST or neurogenic cancers. Primary sarcoma of pancreas (PS) are very rare and most be differentiated from gastrointestinal and retroperitoneal sarcoma with extension to pancreas (1). Among 15,000 patients who were referred to our center for treatment over a 10-year period (2003 - 2013), 95 cases had sarcoma. Among those who had sarcoma, only one case had pancreas sarcoma. Most pancreatic sarcomas (PS) are diagnosed in autopsy (1). Presenting symptoms are nonspecific and are abdominal pain, mass, epigastric tenderness or even may present as acute pancreatitis (1, 2). In order to elucidate the clinical course and behavior and responses to treatment, we searched PubMed for information regarding primary pancreatic sarcoma.
2. Evidence Acquisition
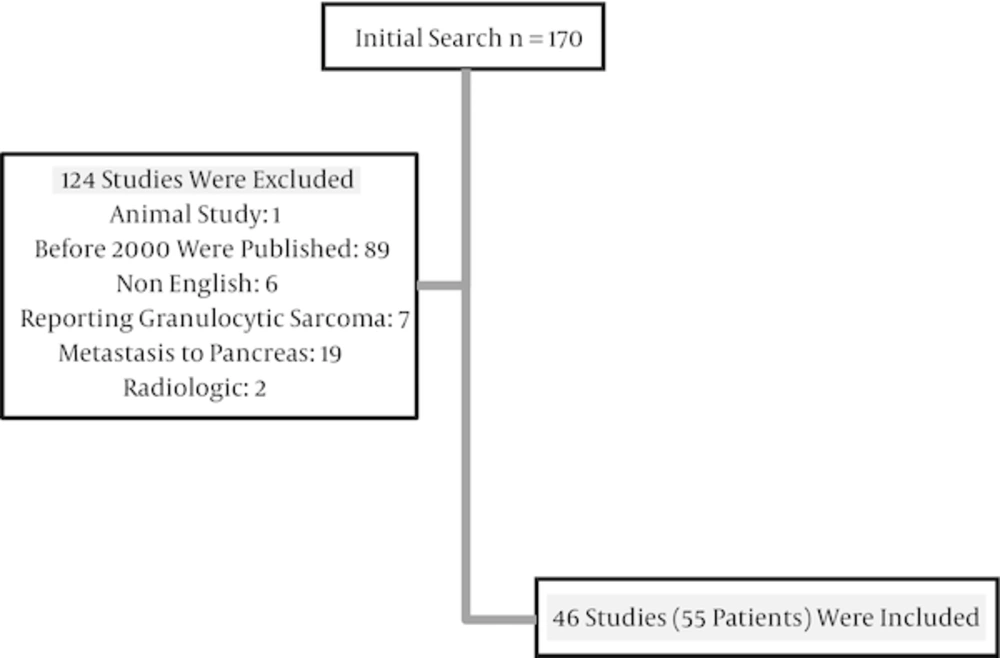
We searched PubMed for primary pancreatic sarcomas. Only studies that reported clinical data were included in the study. Review articles (without reporting a new case), animal studies and genetic or radiologic studies were excluded. Keywords in the title were: “sarcoma” or “leiomyosarcoma” or “liposarcoma” or “rhabdomyosarcoma” or “mesenchymal” or “malignant fibrous histiocytomas” AND “pancreas” or “pancreatic”. Articles that had no information about a new patient or were published before the year 2000 were excluded. Metastasis to pancreas (non-primary pancreatic tumors) and non-English reports were also exclusion criteria.
All clinical data, including age, sex, and disease presentation, type of sarcoma, and completeness of resection, treatment, site of metastasis and survival were collected. Some studies reported a case and then reported a review. Only the data of reported case(s) were collected.
3. Results
We found 170 articles in PubMed. Eighty-nine articles were published before 2000 and six articles were in a non-English language. Nineteen articles reported metastasis to pancreas. Seven articles reported granulocytic sarcoma, which is a presentation of acute myeloid leukemia (3). One report was about a cat. Two reports were on a radiologic description and contained no other clinical information (Figure 1).
We found 46 reports and 55 patients. One article reported on nine cases of pancreatic leiomyosarcoma (4). Others included reports on one or two cases in each study. Mean age was 57.1 ± 16.7 years (median: 59; range: 23 - 83 years), 27 patients were male and 28 patients were female. Median survival was 14 months. One, 3 and 5 years overall survivals were 78.4, 48.5 and 48.5 percent, respectively.
Two studies had no information about presenting symptoms. The most common presenting symptom was pain. Eighteen patients had abdominal pain. Pain was the sole presentation (in nine cases), or in combination with other symptoms. Nine patients had mass sensation or had palpable mass. Four patients had jaundice and sarcoma was found in eight cases incidentally. Other less common symptoms were fever, deep vein thrombosis (DVT), anemia and gastrointestinal bleeding. Mean survival among those whose diseases were detected incidentally was 17.3 (4 - 48) months.
In our review, 10 patients had not been operated on. Their survival was from 3 to 27 months and mean survival was 9.5 (3 - 27) months. In this group only two patients were alive at the presentation for 3 and 12 months. Survival among 41 patients who had undergone operations was 30.2 (0.5 - 240) months. In five patients, type of surgery or survival were not obvious. There may be other patients who were not operated and were not reported.
Type and details of adjuvant therapy was not reported in five articles. In 31 cases, no adjuvant treatment was prescribed. Others received different chemotherapy agents. The most common agent was gemcitabine in three reports and doxorubicin in two cases. Other agents were capecitabine, myocet, ifosfamid and cisplatin. Transcatheter arterial chemoembolization (TACE) was done for a patient with clear cell sarcoma, but this patient died from liver metastasis after 10 months. One patient received radiotherapy alone and another patient received chemotherapy and radiotherapy. A 76 year old man with pancreatic liposarcoma received adjuvant radiotherapy and was alive for 26 months.
In eight studies, tumor size was not mentioned. In others, mean tumor size was 9.0 ± 6.8 cm (1 - 27 cm). The most common type was leiomyosarcoma (16 patients). Nine patients had carcinosarcoma and six cases had MFH. Four patients had liposarcoma. Angiosarcoma, Ewing’s and fusocellular sarcoma were seen in two cases. One case had rhabdomyosarcoma and subtype was not determined in three cases.
Thirty patients had no metastasis at the time of report and metastatic state was not disclosed in seven cases. Fourteen patients had liver metastasis and four patients had metastasis beyond liver. The most common site of metastases were lung, bone, ovary, and peritoneum.
In our review, four cases had a more than 5-year survival. Mean age in this group was 52 (40 - 64) years. Among them, three were alive at the time of presentation. Three patients had leiomyosarcoma and one case had inflammatory myofibroblastic tumor. All had undergone complete tumor removal and none received adjuvant treatment (4-6).
Among reported cases, 10 patients had 6 months or less overall survival. In these patients, mean survival was three (0.5 - 6) months. In five cases, tumors were completely resected. Four cases were unresectable and in one case, information was not complete. One case had angiosarcoma, two patients had MFH, two cases had leiomyosarcoma, and four cases had carcinosarcoma. One report mentioned sarcoma. Data were not large enough for statistical analysis (2, 4, 7-14).
Thirty patients were alive at the time of report and 22 patients had died. Information about three patients was unclear. Medial follow up for surviving patients was 20 months. Median survival for all patients was 14 months. Five-year and 10-year overall survival rate were 48.5% and 32.3%, respectively. Age (P = 0.076), sex (P = 0.701), and tumor size (P = 0.907) were not prognostic factors for overall survival. Among these patients, the number of patients was not sufficient for analysis for the effect on survival.
4. Conclusions
Sarcomas are rare human malignancies and pancreatic sarcomas (PS) are even rarer (13). Most malignancies in the pancreas are epithelial originated adenocarcinoma. Gastro-intestinal stromal tumors (GIST) and neurogenic tumors are the most common non epithelial pancreatic tumors (1). Before histological evaluation, differentiating from epithelial carcinoma is not possible (2). Tumor markers, other laboratory tests, and physical examination radiologic studies are not helpful to differentiate sarcoma from epithelial tumors (2).
In our review, the most common presenting symptom was abdominal pain. Only four patients had jaundice at presentation, but it is a usual presenting symptom in pancreas adenocarcinoma. History of alcohol consumption was not a known effect on pancreatic sarcoma (13).
The main stay of treatment for PS is surgery (1). In our review, 10 patients had not been operated on. Of course reporting a rare case with a good survival is more attractive for an author. We guess that some cases with an advanced disease and poor outcome were not reported.
Although lymph node (LN) dissection is not necessary for pancreas sarcoma, LN metastasis is reported in some studies (15-18). Reilly reported LN metastasis in a 23 years old man with Ewing's sarcoma of pancreas (19). Zhu reported LN metastasis in a case of carcinosarcoma (20). It seems that type of sarcoma is important to decide about LN dissection.
The role of chemotherapy and radiotherapy in pancreatic sarcoma are not well studied. In our review, only two patients received radiotherapy. One patient received radiotherapy for liposarcoma and another patient received chemotherapy and radiotherapy for rhabdomyosarcoma. The first patient was alive and disease free for 26 months. The other female patient with rhabdomyosarcoma died from local recurrence and then widespread metastasis after 26 months (21, 22).
Some authors believe that chemotherapy is not very effective in survival prolongation (16). Moletta reported a 54-year-old woman who had a pancreatic leiomyosarcoma with liver metastasis at presentation. She received chemotherapy (myocet and ifosfamide) after distal pancreatectomy. She had lung and then ovary metastasis and was operated for both nine months after panreatectomy. She was alive for 37 months (23). Choosing chemotherapy agents is not easy. Some authors have used drugs that are known to be effective in epithelial pancreas tumor (13). Although there is no clear evidence, for PS we suggest chemotherapy agents that are effective in sarcoma.
Thirty-one patients had no recurrence at the time of report and six patients had no clear information about metastasis, and three patients had local recurrence. Liver was the most common site for metastasis and 14 patients had liver metastasis. Lung and peritoneum, bone and ovary were other sites for recurrence.
Pancreatic sarcoma may have an indolent and slowly progressive course. Vanderpuye reported a case of pancreatic leiomyosarcoma who presented with liver metastasis. The liver lesion was not operated and the patient received capecitabine with no response. Then he received adriamicin with a partial response. Although his disease was progressing and lung and bone metastasis happened, the patient was alive two years after presentation (24). We found other reports about pancreatic sarcoma with metastasis and a relatively prolonged survival. Hur et al. reported (1) a 70-year-old woman with pancreatic leiomyosarcoma. Their patient was operated on and her tumor was resected completely. After six months she had developed liver metastasis and she refused chemotherapy. Attractively, she survived for 16 months. Muhammad (9) reported an old man with metastasis at presentation. He died three months after operation. On the other hand some authors have reported an aggressive behavior for this disease.
As mentioned above, in our review, four cases had a more than 5-year survival. All had undergone complete tumor removal and none received adjuvant treatment (4-6). On the other hand, PS may have an aggressive and fatal course (2, 4, 7-14).
In conclusion, larger reports should include more complete information on clinical course, DFS and OS. Currently, it is difficult to draw any obvious treatment schedule.