1. Background
CNS tumors have an average annual age-adjusted incidence of 28.57 per 100000 population (1). Gliomas are the most common primary brain tumours.
The combination of surgery (to confirm diagnosis and to achieve macroscopic excision), post-operative radiotherapy, and chemotherapy represents the standard approach to the treatment of high grade gliomas. Three-dimensional conformal therapy (3DCRT) is increasingly used in the treatment of primary brain tumours. The use of intensity-modulated radiotherapy (IMRT) yields conformal dose distributions and better avoidance of organs at risk (2).
Memory impairment is a well-documented side effect of cranial irradiation. One possible hypothesis focuses on a neurogenic stem cell compartment in the hippocampus, which is highly sensitive to radiation and potentially central to radiation-induced memory impairment. Damage to neural progenitor cells located in the subgranular zone of the hippocampus results in radiation-induced neurocognitive decline, specifically in terms of short-term memory formation and recall (2).
Hippocampus belongs to the limbic system and plays an important role in the consolidation of information from short-term memory to long-term memory and spatial navigation. The hippocampal formation includes the dentate gyrus, hippocampus, subiculum, and entorhinal cortex.
In high grade gliomas, post-operative radiation therapy can be delivered while sparing hippocampus without compromising the outcome. This has been evaluated in many studies (3).
In this study we evaluated the possibility of sparing the hippocampi in post-operative radiation therapy for high grade glioma (3DCRT/IMRT technique) and its impact on preservation of memory function.
2. Methods
2.1. Eligibility Criteria
The study protocol and consent procedure were approved by the Medical ethics committee. Patients aged between 18 - 70 years with a Karnofsky performance score (KPS) of more than or equal to 70, with histologically confirmed high grade glioma, and no prior history of chemotherapy and cranial radiotherapy, were eligible.
After obtaining informed consent, patients were randomly assigned to post-operative partial brain irradiation via the 3DCRT (3DCRT arm) or IMRT technique (IMRT arm), combined with concurrent and adjuvant temozolomide (TMZ) in both arms.
2.2. Radiation Therapy (RT)
2.2.1. Target Volumes
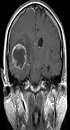
Gross tumor volume (GTV) was defined as the resection cavity with any residual contrast-enhancing tissue on T1-weighted magnetic resonance imaging. The clinical target volume (CTV) was defined as the GTV with a 2 cm expansion to include any potential subclinical disease, with attempts made to respect the natural anatomic boundaries and organs at risk (OAR). An initial planning target volume (PTV) was generated by adding a 5mm expansion to the CTV to account for setup uncertainties and a dose of 50 Gy in 25 fractions was prescribed to this volume. Sequential boost dose of 10 Gy in 5 fractions was delivered to the boost PTV, which was generated by adding a 5 mm margin to the GTV.
2.2.2. Hippocampal Sparing
Bilateral hippocampi were contoured according to RTOG 0933 contouring atlas (4). Hippocampal avoidance regions were created using a 5 mm volumetric expansion around the hippocampus to spare the subgranular zone of the hippocampus.
2.3. Chemotherapy
2.3.1. Concurrent Phase
An oral tablet of Temozolomide, 75 mg/m2, 5 days a week, was given to patients in both arms, half an hour before radiation therapy, under fasting condition.
2.3.2. Adjuvant Phase
Oral tablet of Temozolomide, 150 - 200 mg/m2, under fasting condition for 5 consecutive days once in 28 days for 6 months starting after a gap of 28 days from the day of completion of concurrent chemoradiation.
All patients received steroids during the 1st week of radiation therapy.
2.3.3. Memory Function Test
Patient’s memory function was assessed using the P.G.I. Memory scale (5) before, during, and at 3 time points after completion of radiotherapy (immediately, at 3 months, and at 6 months).
2.3.4. Follow up
Patients were on follow-up till 6 months post chemoradiation.
3. Results
3.1. Statistical Methods
Descriptive and inferential statistical analysis was carried out. Results on continuous measurements are presented as mean ± SD (min - max) and results on categorical measurements are presented as number (percent). Significance is assessed at 5% level of significance.
Student t-test (2 tailed, independent) has been used to find the significance of study parameters on a continuous scale between the 2 groups (inter group analysis) on metric parameters. Student t-test (2 tailed, dependent) has been used to find the significance of study parameters on continuous scale with in each group.
Chi-square/ Fisher Exact test has been used to find the significance of study parameters on categorical scale between 2 or more groups.
The statistical software’s, namely SAS 9.2, SPSS 15.0, Stata 10.1, MedCalc 9.0.1, Systat 12.0, and R environment ver.2.11.1 were used for the analysis.
| Variables | 3DCRT | IMRT | P Value |
|---|---|---|---|
| Total | 10 (100) | 10 (100) | |
| Age, y | 0.488 | ||
| 21 - 30 | 2 (20) | 1 (10) | |
| 31 - 40 | 2 (20) | 3 (30) | |
| 41 - 50 | 5 (50) | 3 (30) | |
| 51 - 60 | 1 (10) | 3 (30) | |
| Gender | 0.35 | ||
| Male | 8 (80) | 5 (50) | |
| Female | 2 (200 | 5 (50) | |
| KPS | 0.382 | ||
| 70 | 1 (10) | 3 (30) | |
| 80 | 5 (50) | 4 (40) | |
| 90 | 4 (40) | 3 (30) | |
| Neurological deficit | 1 | ||
| Yes | 2 (20) | 1 (10) | |
| No | 8 (80) | 9 (90) | |
| Laterality | 0.65 | ||
| Left side | 5 (50) | 7 (70) | |
| Right side | 5 (50) | 3 (30) | |
| Histology | 0.65 | ||
| Anaplastic oligodendroglioma | 5 (50) | 6 (60) | |
| Glioblastoma | 5 (50) | 4 (40) |
Patient and Tumor Characteristicsa
| Sub Test and Maximum Score | 3DCRT | IMRT | P Value |
|---|---|---|---|
| 1- Remote memory (max score = 6) | |||
| Before RT | 4.40 ± 0.52 | 4.20 ± 0.63 | 0.449 |
| During RT | 4.30 ± 0.95 | 4.50 ± 0.53 | 0.567 |
| After RT | 4.30 ± 0.95 | 4.40 ± 0.52 | 0.773 |
| 3 months Post-RT | 3.40 ± 1.35 | 4.10 ± 0.57 | 0.148 |
| 6 months Post-RT | 3.20 ± 1.32 | 3.60 ± 0.70 | 0.407 |
| 2- Recent memory (max score = 5) | |||
| Before RT | 4.30 ± 0.48 | 4.30 ± 0.48 | 1 |
| During RT | 4.20 ± 0.79 | 4.30 ± 0.67 | 0.764 |
| After RT | 4.40 ± 0.70 | 4.40 ± 0.70 | 1 |
| 3 months Post-RT | 3.70 ± 1.42 | 4.20 ± 0.63 | 0.322 |
| 6 months Post-RT | 3.40 ± 1.35 | 4.10 ± 0.32 | 0.128 |
| 3- Mental balance (max score = 9) | |||
| Before RT | 6.70 ± 0.95 | 6.50 ± 1.08 | 0.665 |
| During RT | 6.70 ± 0.95 | 6.10 ± 1.10 | 0.208 |
| After RT | 6.40 ± 1.26 | 6.30 ± 1.06 | 0.85 |
| 3 months Post-RT | 5.90 ± 2.33 | 6.00 ± 1.15 | 0.905 |
| 6 months Post-RT | 5.30 ± 2.11 | 5.90 ± 1.20 | 0.444 |
| 4- Attention and concentration (max score = 16) | |||
| Before RT | 12.00 ± 0.82 | 12.20 ± 0.79 | 0.584 |
| During RT | 11.50 ± 0.53 | 12.40 ± 1.07 | 0.029a |
| After RT | 11.70 ± 1.06 | 12.40 ± 0.84 | 0.119 |
| 3 months Post-RT | 10.60 ± 3.84 | 12.20 ± 1.23 | 0.225 |
| 6 months Post-RT | 9.90 ± 3.63 | 11.50 ± 1.43 | 0.212 |
| 5- Delayed recall (max score = 10) | |||
| Before RT | 6.30 ± 1.16 | 6.30 ± 1.06 | 1 |
| During RT | 6.10 ± 1.52 | 6.40 ± 0.97 | 0.605 |
| After RT | 5.70 ± 1.42 | 6.40 ± 1.17 | 0.245 |
| 3 months Post-RT | 4.80 ± 2.10 | 6.10 ± 1.10 | 0.1 |
| 6 months Post-RT | 4.30 ± 1.89 | 5.40 ± 1.07 | 0.127 |
| 6- Immediate recall (max score = 12) | |||
| Before RT | 8.40 ± 0.97 | 9.50 ± 1.08 | 0.027a |
| During RT | 8.20 ± 0.79 | 9.50 ± 1.18 | 0.010b |
| After RT | 7.80 ± 1.23 | 9.60 ± 1.35 | 0.006b |
| 3 months Post-RT | 6.80 ± 2.57 | 9.30 ± 1.16 | 0.012a |
| 6 months Post-RT | 6.40 ± 2.32 | 8.90 ± 1.20 | 0.007b |
| 7- Verbal retention for similar pairs (max score = 5) | |||
| Before RT | 4.30 ± 1.34 | 3.80 ± 0.42 | 0.274 |
| During RT | 4.30 ± 1.42 | 4.10 ± 0.74 | 0.697 |
| After RT | 3.80 ± 1.32 | 3.90 ± 0.57 | 0.828 |
| 3 months Post-RT | 3.40 ± 1.51 | 3.70 ± 0.67 | 0.572 |
| 6 months Post-RT | 3.00 ± 1.41 | 3.10 ± 0.57 | 0.838 |
| 8- Verbal retention for dissimilar pairs (max score = 15) | |||
| Before RT | 10.90 ± 1.45 | 9.70 ± 1.16 | 0.056c |
| During RT | 10.70 ± 2.16 | 9.50 ± 1.18 | 0.141 |
| After RT | 10.30 ± 1.83 | 9.50 ± 1.51 | 0.3 |
| 3 months Post-RT | 9.30 ± 3.53 | 9.00 ± 1.63 | 0.81 |
| 6 months Post-RT | 8.50 ± 3.17 | 8.50 ± 1.72 | 1 |
| 9- Visual retention (max score = 13) | |||
| Before RT | 9.70 ± 1.89 | 9.00 ± 1.25 | 0.341 |
| During RT | 9.40 ± 2.17 | 8.90 ± 1.29 | 0.539 |
| After RT | 9.00 ± 1.83 | 8.90 ± 1.20 | 0.886 |
| 3 months Post-RT | 8.00 ± 3.37 | 8.40 ± 1.17 | 0.727 |
| 6 months Post-RT | 7.30 ± 3.13 | 8.20 ± 1.14 | 0.404 |
| 10- Recognition (max score = 10) | |||
| Before RT | 6.80 ± 0.92 | 7.00 ± 0.94 | 0.637 |
| During RT | 6.70 ± 1.06 | 6.90 ± 0.74 | 0.63 |
| After RT | 6.50 ± 1.27 | 7.00 ± 0.47 | 0.258 |
| 3 months Post-RT | 5.60 ± 2.17 | 6.60 ± 0.84 | 0.191 |
| 6 months Post-RT | 4.90 ± 1.97 | 6.00 ± 0.82 | 0.12 |
Assessment of Memory Function
4. Discussion
Standard management for high grade glioma is surgery followed by post-operative radiotherapy with concurrent and adjuvant temozolomide. Radiotherapy technique has evolved from whole brain radiotherapy (WBRT) using 2D cobalt to the present standard of care of delivering focal high dose radiation therapy using 3DCRT/IMRT technique. This has led to improved tumor control and survival.
Quality of life is increasingly relevant as patients’ survival improves. Hence, stress is being laid on maintaining a good quality of life of patients after treatment by reducing toxicity of radiation. Toxicities following cranial irradiation can be classified as acute and late.
Acute radiation morbidities include fatigue, erythema, alopecia, headache and rarely, nausea with or without vomiting; these are generally not severe and are usually self-limiting (6).
Late effects of radiation, especially cognitive impairment, are more worrisome and may become manifest many years later. In the era of 2D-WBRT, post radiotherapy neurological toxicities in the form of memory loss were very common.
Memory is the ability to retain and reproduce impression once perceived intentionally (5). Short-term memory, also known as working memory, allows recall for a period of several seconds to a minute without rehearsal. Long-term memory can store much larger quantities of information for potentially unlimited duration (sometimes a whole life span).
The hippocampus is essential for consolidation of information from short-term to long-term memory. Hippocampus, which is a part of limbic system, is important for memory, executive functioning, and emotional responses. It is known to be sensitive to radiotherapy (7).
Though memory impairment is a well-documented side-effect of cranial irradiation, the underlying cause is ill-defined. One possible hypothesis focuses on a neurogenic stem cell compartment in the hippocampus that is highly sensitive to radiation and potentially central to radiation-induced memory impairment. The neurocognitive effects of cranial radiotherapy in patients with gliomas are well-recognized and may be related to the dose delivered to the hippocampi (3). Preclinical models have shown that hippocampal irradiation can impair spatial learning and memory, however, currently clinical data are lacking.
Hippocampal-sparing is defined as a mean dose to at least 1 hippocampus of less than 30 Gy (3). This correlates with a dose constraint of 17 Gy in 10 fractions to the hippocampus used in the RTOG 0933 protocol.
After reviewing the literature on neurocognitive effects of cranial irradiation Vinai Gondi et al., (4) discussed clinical and preclinical data associating damage to neural progenitor cells located in subgranular zone of the hippocampus with radiation-induced neurocognitive decline, specifically in terms of short-term memory formation and recall, the feasibility and risks of sparing the subgranular zone of the hippocampus during whole-brain radiotherapy for brain metastases, and provided a detailed and comprehensive discussion of the rationale for using modern IMRT techniques to spare the subgranular zone of the hippocampus during cranial irradiation.
In a feasibility study, Marsh et al., (8) concluded that it is possible to spare contralateral limbic circuit, neural stem cell compartment, and hippocampus during partial brain radiotherapy for both high- and low-grade gliomas using IMRT. This approach may reduce late cognitive squeal of cranial radiotherapy.
Pinkham et al., (3) retrospectively reviewed consecutive patients with WHO grade II and III gliomas treated with IMRT at their institution between January 2009 and August 2012. A total of 18 patients were identified and hippocampal-sparing was achieved in 14 (78%). They concluded that Hippocampal-sparing radiotherapy is feasible in patients with WHO grade II and III gliomas and that IMRT can be used to selectively spare the hippocampi without compromising the dose delivered to the tumour.
As noted in above studies, in our study also, we could achieve bilateral hippocampal sparing in all patients in IMRT arm (21 Gy in contralateral and 29 Gy in ipsilateral Hippocampus). Whereas, in 3DCRT arm, ipsilateral hippocampus could be spared in 60% of patients (24 Gy in contralateral hippocampus and 34 Gy in ipsilateral hippocampus), favoring the IMRT technique for hippocampal sparing post-operative radiation therapy without compromise in delivery of prescribed dose to PTV.
Further, analysis of serial memory function scores showed that in 6 subtests of P.G.I. memory scale (mental balance, delayed recall, verbal retention for similar and dissimilar pairs, visual retention, and recognition), the patients in IMRT arm had maintenance of the score for a period 3 months post radiotherapy while patients in 3DCRT arm showed a decline immediately after radiotherapy. Thus, a trend towards benefit of IMRT is observed allowing for longer preservation of memory function when compared to 3DCRT. This co-relates with bilateral hippocampal sparing, which was achieved in the IMRT arm.
4.1. Conclusion
Bilateral hippocampal sparing, with preservation of memory function, is achievable with the IMRT technique for delivery of post-operative radiotherapy in patients with high grade glioma without compromise in prescribed dose delivery.