1. Introduction
It is well known that most pancreas tumors are adenocarcinoma, and stromal tumors of pancreas are not very common. The most common non-epithelial pancreatic sarcomas are GIST and neurogenic tumors (1).
Sarcoma of the pancreas is a rare disease and consists of 0.1% of pancreas cancers. Although this disease has been known since the 19th century, the standard treatment is not well known (2, 3). Little is also known about the origin of these tumors. Leiomyosarcoma probably originates from smooth muscle cells, in vessels or ducts of pancreas. Surgery may be the only curative treatment (4).
Until 2014, 45 cases of pancreatic leiomyosarcoma were reported (5). This disease affects both genders equally and mean age of the patients is in the 6th decade of life. Survival may be less than 6 months or more than 5 years.
Treatment options are surgery, radiotherapy, and chemotherapy (6). The aim of this report was to share the experience of the current researchers with other clinicians.
2. Case Presentation
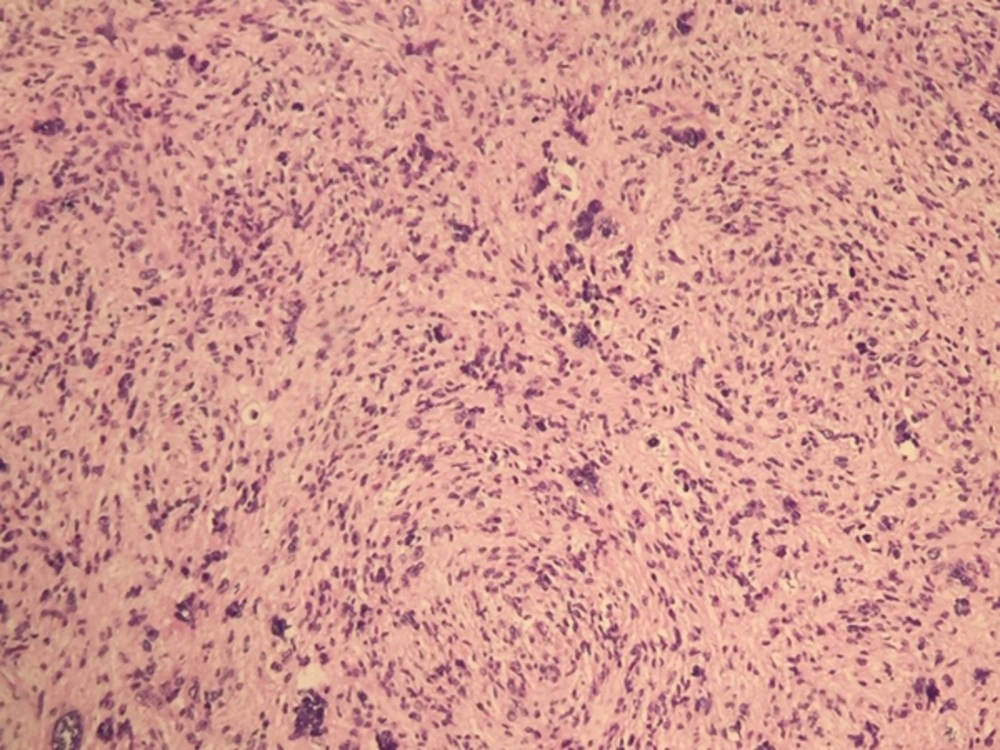
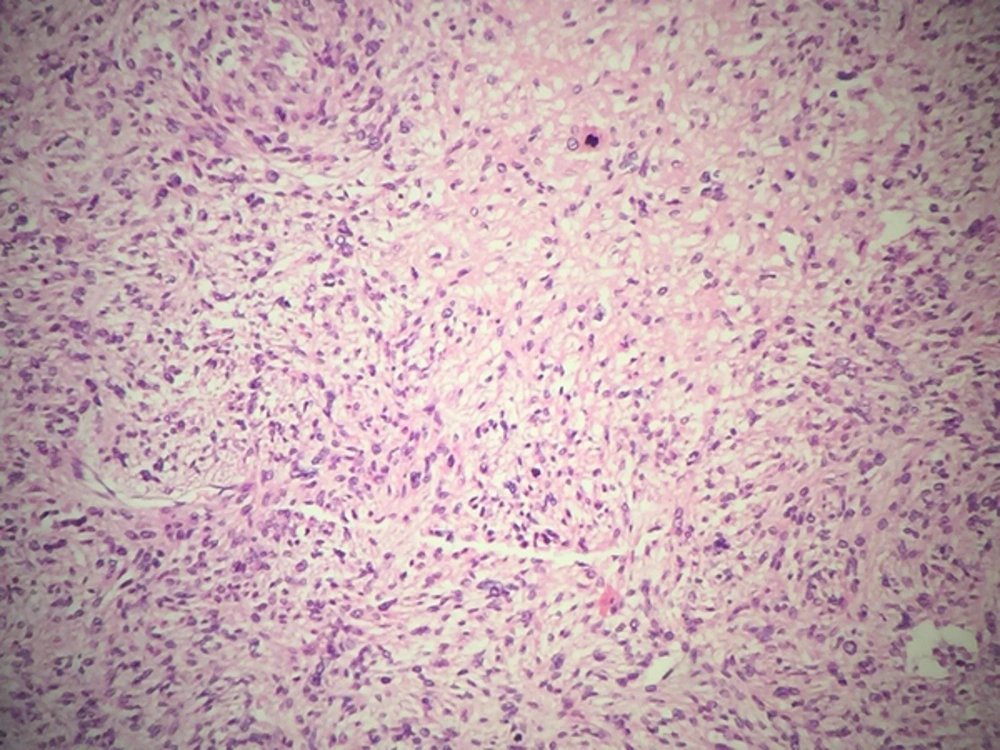
The patient was a 57-year-old male, who had epigastric pain for several months before referring to the general surgeon. Laboratory tests, consisting liver function tests, renal function tests, and complete blood count were normal. Upper gastrointestinal (GI) endoscopy and abdominal sonography was done and showed a large mass in the pancreas tail. At that time, chest and abdominal and pelvic CT scan with contrast were normal and no metastasis was found. Subtotal pancreatectomy and splenectomy was done for the patient. A 12 × 6 × 5 cm lesion was detected in the pancreas. Histological examination showed leiomyosarcoma (Figures 1 and 2). The resected margins were free of tumor. He received radiotherapy of the tumor bed up to 45 Gy in 25 fractions (1.8 Gy per fraction, 5 fractions per week). No chemotherapy was administered. He was well in the follow-up visits and imaging. After 11 months, abdominopelvic sonography, for routine surveillance, revealed a 6 × 5 × 4 cm mass in the liver. He received no chemotherapy and succumbed to death 3 months later.
3. Discussion
Leiomyosarcoma is a rare (less than 1%) human malignancy. It mostly occurs in the uterus and soft tissues. Pancreatic leiomyosarcoma is even a rarer tumor and differentiating this type of malignancy from other pancreatic tumors without pathologic diagnosis is not possible. In these cases, preoperative needle sampling is not easily performed, because obtaining adequate tissue is difficult. Until 2014, 45 cases were reported.
Pancreatic leiomyosarcoma affects older people (mean age of 53 years) and both males and females are equally involved (5, 7-9). These tumors have no specific symptom and usually present large masses (mean size = 11 cm). Smaller tumors are detected incidentally. Head and tail of the pancreas are involved equally (8).
Some authors believe it has an aggressive course and usually presents in advanced stages (1, 8). Shimizu reported a 49-year-old female with pancreas leiomyosarcoma. She presented abdominal pain and jaundice, and had lung metastasis at the same time. She received chemotherapy, but died after 3 months. Chemotherapy regimen was not well described in the article (10). Muhammad also reported a 73-year-old male with pancreatic leiomyosarcoma and liver metastasis at presentation. He had weight loss and had a 10-cm mass in the body of the pancreas. Despite chemotherapy, he died after 3 months (11).
These patients had metastasis at presentation and a short survival duration. Moletta reported a case of pancreas leiomyosarcoma, who had liver metastasis at presentation. She was a 57-year-old lady, who had a liver operation and pancreas lesion. Shortly (1 month) after the 1st operation, she developed lung and ovary metastasis. She received ifosfamide and liposomal doxorubicin and her lung lesion was operated. She had an adenocarcinoma in her lung. She received gemcitabine docetaxel, trabectedin, and dacarbazine in sequence. After 27 months, her ovary lesions were removed and she developed liver metastasis again. At the time of the report, the patient was alive with liver metastasis (4).
In contrast to the above reports, the literature review found cases with an indolent course. Deveaux reported on a 44-year-old female with a 5-cm leiomyosarcoma in the head of the pancreas. Her pancreatic leiomyosarcoma presented as an epigastric mass and the mass was completely removed. No chemotherapy or radiotherapy was offered to her and she was alive for 4 years, at the time of the report (12).
As noted above, a few patients with pancreatic leiomyosarcoma have been reported thus far. It is difficult to find a predictable pattern of clinical course in this small group of patients. Maarouf reported on a 40-year-old female with a 4-cm leiomyosarcoma in the tail of the panaceas. The lesion was solid cystic and FNA was not successful. After distal pancreatosplenectomy, no adjuvant treatment was offered. She was alive and well after 20 years (13). The researchers found no case of pancreatic leiomyosarcoma and longer survival.
Data is very sparse on chemotherapy for these patients, and standard chemotherapy regimens are not well defined. Kocakoc in 2014 and Feather in 1950 reported 2 cases of pancreatic leiomyosarcoma. In older reports, total pancreactomy was done for young patients (29 years old). Although lymph node metastasis was present, he was alive and well for 16 months. A recent case was a 56-year-old female, who underwent distal pancreatectomy and was also alive and well after 1 year. None of them received adjuvant treatment (2, 5). During this period of time, little question on treatment are responded. In conclusion, further studies are needed to draw a conclusion on treatment and outcome of pancreatic leiomyosarcoma.