1. Introduction
Extramedullary plasmacytoma (EMP) is a rare plasma cell neoplasm that involves the soft tissue (1). They are solitary lesions, and are most frequently situated in the head and neck area (2). The EMP of the head and neck accounts for only 3% of all the plasma cell tumors. It occurs more frequently in the upper respiratory tract, particularly in the nasal cavity and paranasal sinuses. It comprises less than 1% of the head and neck tumors (1).
It is a destructive tumor with a tendency for local recurrence (3, 4). It has a male preponderance and is more common during the fifth and sixth decades of life (1).
Multiple myeloma, plasmacytoma, or Waldenström macroglobulinemia of the bone should be ruled out with a systemic work-up and continuous follow-up, including electrophoresis of the serum proteins, Bence-Jones protein in urine, skeletal survey, and bone marrow biopsy (2, 5, 6).
The best treatment for EMP of the sinonasal cavity has not been well-established yet (7). However, radiotherapy has been proposed as treatment of choice for EMP by several researchers (2). Complete resection of a tumor is a treatment option for EMP (2).
A patient with EMP of the nasal cavity and right maxillary sinus presented to the Outpatient Clinic of Baqiyatallah Hospital, which is a tertiary referral hospital affiliated to Baqiyatallah University of Medical Sciences, Tehran, Iran. The aim of this case report is to review clinical presentation, diagnosis, and treatment of this rare disease. The EMP should be considered as a differential diagnosis of the nasal cavity and paranasal masses.
2. Case Presentation
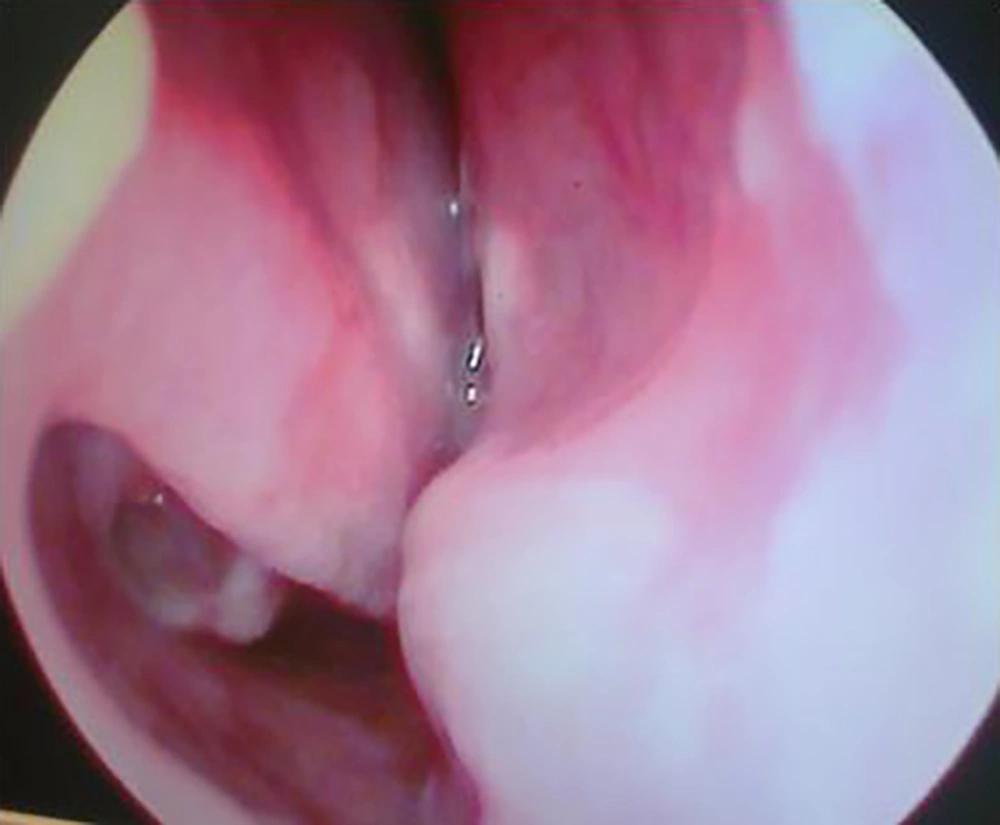
We presented a 78-year-old man with right facial swelling, right exophthalmos, diplopia, and decrease in visual acuity of right eye for three weeks. On examination, a facial swelling was noted around the right eye (Figure 1A). The surrounding skin was erythematous, the mass was firm on palpation, and it was not tender or pulsatile. Neither skin puckering nor tethering was noted. On the nasal endoscopy examination, a nasal mass occupying right nasal cavity, with vascular appearance and friable consistency was identified (Figure 2).
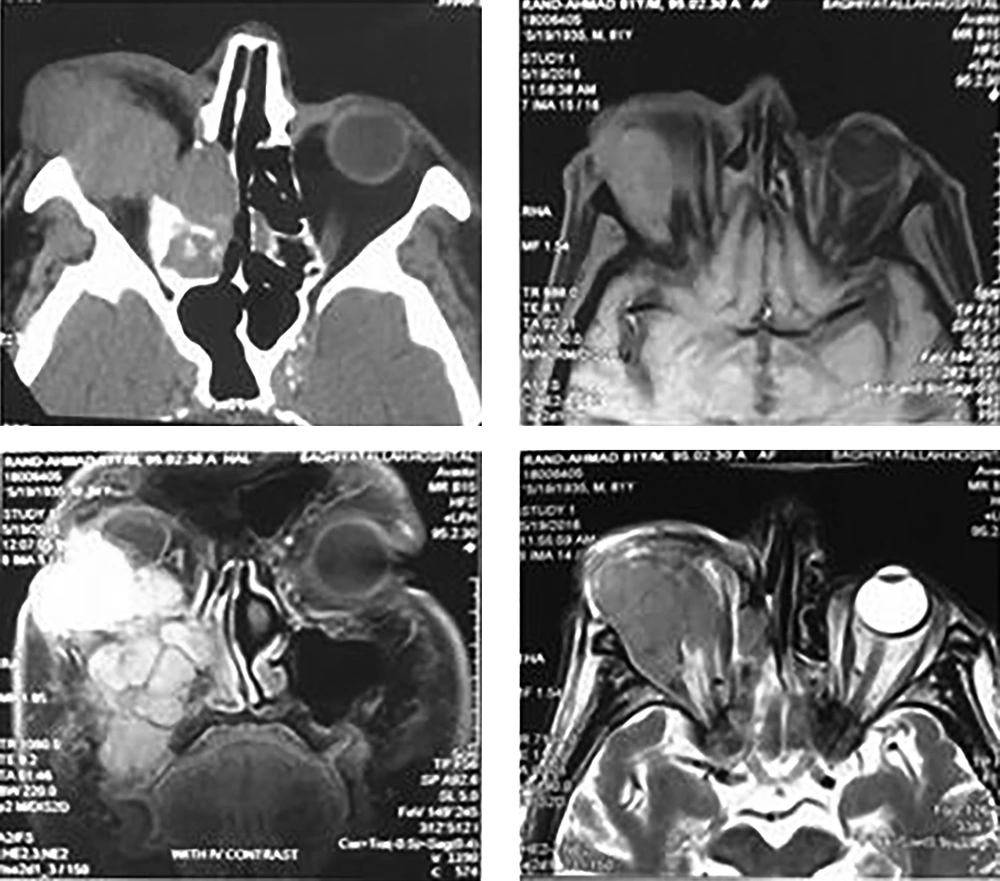
In addition, the patient had an oral fistula with pus discharge since six weeks before presentation. Ophthalmologic examination revealed right exophthalmos and visual acuity of the right eye was decreased to light perception. Oral cavity examination showed a fistula near upper premolar tooth. No cervical lymphadenopathy was noted. Computed tomography (CT) scan of paranasal sinuses revealed a mass in the right maxillary and ethmoid sinuses with orbital extension (Figure 3A). The magnetic resonance imaging (MRI), with contrast, showed a mass with intermediate intensity and orbital extension that was enhanced with contrast. The mass was hypointense on T1 and T2 MRI (Figure 3B - 3D).
A, axial plane of CT scan shows soft tissue density in the right nasal cavity; B, axial plane of T1 MRI shows hypointense mass in right orbital space; C, coronal plane of T1 MRI with contrast shows a right nasal mass with intraorbital extension which is enhanced with contrast; D, axial plane of T2 MRI shows right hypointense nasal mass with intraorbital extension (CT: computed tomography).
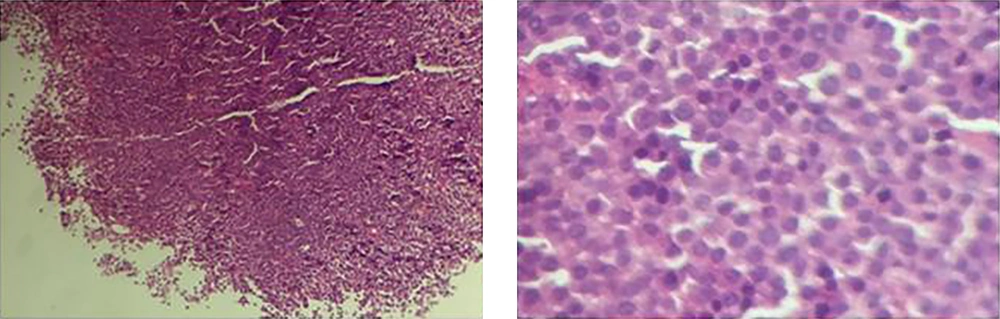
An immunohistochemical panel including CD38, CD138, CD20, CD3, cytokeratin, kappa, and lambda light was performed. Cells lacked CD20, CD3, and cytokeratin expression and were positive for CD38, CD138, kappa, and lambda light chains, which was in favor of plasmacytoma. Histopathologic examination showed plasmacytoma of paransal sinuses (Figure 4). Patient received 56 gray (Gy) in 28 fractions of radiotherapy. He was well in the follow-up visits during the next one year (Figure 1B). Neither recurrence nor developing into multiple myeloma was detected. The CT examinations after three and six months post-radiotherapy were performed. Biopsy was taken from maxillary sinus after three months post-radiotherapy due to residual opacity, which was seen on the CT examination. Histopathologic examination revealed only necrotic tissue. The CT scan after six months revealed disease stabilization. No serious complications of treatment were observed thus far. Informed consent was obtained from the patient to publish case report.
3. Discussion
Plasma cell neoplasms (plasma cell dyscrasia) presents either as a solitary plasmacytoma (a single lesion) or as a multiple myeloma (multiple lesions). Solitary plasmacytomas can present as a solitary plasmacytoma of bone (SBP) or extramedullary plasmacytoma (EMP) (2, 8, 9).
EMPs are most frequently situated in the head and neck area (2). Approximately 80% to 90% of them affect the mucosa-associated lymphoid tissue (MALT) of the upper airways, 75% of which affect the nasal and paranasal areas (10). EMPs make up 4% of all non-epithelial sinonasal tumors (7).
Inhaled irritants or viral infection may be the etiology of EMP (10). The most common clinical findings of EMP of paranasal sinuses and nasal cavity include nasal obstruction, soft tissue mass that is fleshy, yellowish grey to dark red sessile, polypoid, or pedunculated. Epistaxis, nasal discharge, pain, and more rarely cranial nerve palsy and neck lymphadenopathy are other manifestations of EMP (1).
Distinguishing EMP from other plasma cell tumors is vital in predicting the prognosis properly and providing better treatment. Multiple myeloma and Waldenström macroglobulinemia are its main differential diagnoses (1, 2).
In the present case, multiple myeloma was excluded with performing a systemic work-up including blood profile, liver and renal function, serum and urinary protein electrophoresis, serum immunoglobulin level, skeletal survey, and bone marrow biopsy (1).
Tissue biopsy, serum electrophoresis, radiological examination of the skeletal system (either a positron emission tomography/computed tomography (PET/CT) scan or magnetic resonance imaging (MRI) of the entire spine and pelvis), and bone marrow study are necessary to establish a proper diagnosis (9).
The treatment of EMPs of the sinonasal cavity has not been well-established yet (7). It is widely believed that the treatment of choice for EMP is radiation therapy (RT), given with curative intent at the recommended dose of 40 to 50 Gy over 4 weeks’ duration (11, 12). If resection was performed completely to make a diagnosis, the role of adjuvant RT is not very clear. Surgical resection may be an effective cure for small lesions, and no adjuvant RT is indicated unless surgeon has a suspicion of residual tumor (2). The five-year survival rate of EMP ranges from 30% to 82% and 10-year rate ranges from 50% to 90% (1). Patients with head and neck EMP, age <50 years, and tumor size of <4 cm without monoclonal protein (M-protein, M-spike) in serum protein electrophoresis (SPEP) have better outcomes (13).
Generally speaking, long-term follow-up is vital due to 16% to 32% chance of developing multiple myeloma in patients with EMPs (14). The patients are seen at three-month intervals for the first two years, next at six-month interval for an additional three years, then yearly or every other year after five years. At follow-up visits, a history and physical examination, complete blood count, serum creatinine, serum calcium, urine and serum protein electrophoresis with immunofixation are performed. For patients with head and neck EMP, a fiberoptic nasopharyngoscopy is performed at each visit. All patients have to undergo CT/PET or MRI (whichever imaging modality was initially performed) every six to 12 months in the first five years (2).
Radiotherapy is the treatment of choice for EMP of the head and neck, without extension to the floor of the anterior and middle cranial fossae or into the orbit (15). In the current case, the size, location, and intra-orbital extension of the tumor led us to perform radiotherapy. Although visual acuity of the patient was not good postradiotherapy, we could preserve the eye with success. No recurrence was detected at clinical examination one year after radiotherapy.
Although the follow-up visits are not sufficiently long to consider the complete remission of tumor definitive, the therapeutic strategy can be adopted in similar nasal and paranasal EMP cases with limited intraorbital extension.
3.1. Conclusions
EMP of the sinonasal tract is uncommon and should be considered in the differential diagnosis of nasal cavity masses particularly during the fifth and sixth decade of life. The treatment of choice for EMP is curative radiation therapy (RT), unless the tumor was completely resected prior to radiotherapy. Follow-up is necessary for EMP patients to assess possible relapse, treatment complications, or developing multiple myeloma. Over the years, EMP can develop into multiple myeloma and therefore, long-term follow-up is absolutely essential.