1. Background
The association between thrombocytosis and malignancies has been known for over a century (1). Numerous studies have been carried out to evaluate thrombocytosis as a prognostic marker (2-8). Thrombocytosis is associated with various gynecological and non-gynecological cancers, especially in thoracic and gastrointestinal malignancies (2, 3, 6). Malignancy-related thrombocytosis is seen in about 4% to 55% of the patients, in particular, more in the advanced stages (9).
Most studies that have investigated the prognostic implications of thrombocytosis in patients with cervical cancer have yielded contradictory results; few have shown positive correlation while others found no such correlation (4, 5, 10-16). India has the largest burden of cervical cancer but there is a lack of studies regarding the incidence of thrombocytosis and its correlation with response and survival.
2. Objectives
We have performed the present study to investigate the incidence and prognostic significance of thrombocytosis in patients with cervical cancer, treated with definitive chemoradiotherapy.
3. Methods
Between January 2008 and December 2012, 195 patients with locally advanced cervical cancer (International Federation of Gynaecology and Obstetrics [FIGO] stages IIB-IIIB) were treated with external beam radiotherapy (EBRT) with a dose of 45 Gy in 25 fractions, on cobalt 60, along with weekly concurrent cisplatin. High dose rate (HDR) brachytherapy, to a dose of 7 Gy in 3 fractions, was delivered either by intracavitary or interstitial brachytherapy. All patients included in the study had completed the planned radiation.
The response to the treatment was assessed 3 months post-treatment in accordance with response evaluation criteria in solid tumors (RECIST). Patients underwent periodic detailed clinical evaluation and imaging (computerized tomography scan) during the follow-up period.
Thrombocytosis was defined as a platelet count greater than 400 × 109/liter on at least 2 separate occasions. Blood tests of all the patients were carried out, including complete blood count at the time of diagnosis and before the start of chemoradiation. Patients who had a previous history of cancer or predisposing conditions to thrombocytosis such as a history of splenectomy, rheumatoid disease, myeloproliferative disorders, acute inflammatory disease, and a history of malignancy were excluded from the study.
3.1. Statistical Analysis
This is a retrospective analytical study. The Kaplan-Meier method was used for determining the overall survival (OS) and disease-free survival (DFS). Statistical significance was defined as a probability value of ≤ 0.05. The significance of potential prognostic factors was assessed by the Cox proportional hazards model. The SPSS software version 15 was used for statistical analysis.
4. Results
In this study, 195 patients were divided into two groups based on their platelet counts. The patients having a platelet count greater than 400 × 109/liter were placed in the thrombocytosis group at presentation (31 patients, 15.8%) and those with platelet counts less than 400 × 109/liter were placed in the non-thrombocytosis group (164 patients, 84.2%). The patient characteristics in both groups are summarized in Table 1.
| Characteristics | All Patients (195) | Patients Without Thrombocytosis (164) | Patients with Thrombocytosis (31) | P Value |
|---|---|---|---|---|
| Age, y | 0.721 | |||
| Mean | 45 | 45 | 44 | |
| < 45 | 113 | 93 | 20 | |
| > 45 | 82 | 71 | 11 | |
| Stage | 1.009 | |||
| II | 101 | 85 | 16 | |
| III | 94 | 79 | 15 | |
| Heamaglobin, g/dL | 0.401 | |||
| < 10 | 28 | 20 | 8 | |
| > 10 | 167 | 144 | 23 | |
| Cumulative cisplatin dose, mg | 0.441 | |||
| ≤ 250 | 134 | 113 | 21 | |
| > 250 | 61 | 51 | 10 | |
| Treatment response | 0.001 | |||
| Partial or complete response | 146 | 131 | 15 | |
| Stable or progressive disease | 49 | 33 | 16 |
Patient Characteristics Classified According to Platelet Level
The mean age of the entire retrospective study was 45 years. The total number of patients with stage II and stage III disease was 101 and 94, respectively and they were comparable in both groups. The hemoglobin level at presentation was more than 10 g/dL in 167 patients in comparison to 28 patients who had levels less than 10 g/dL. Concurrent chemotherapy with weekly cisplatin to a cumulative dose of 250 mg or more was received by 113 patients in the non-thrombocytosis and 21 patients in thrombocytosis group. The response to treatment was evaluated clinically and by imaging.
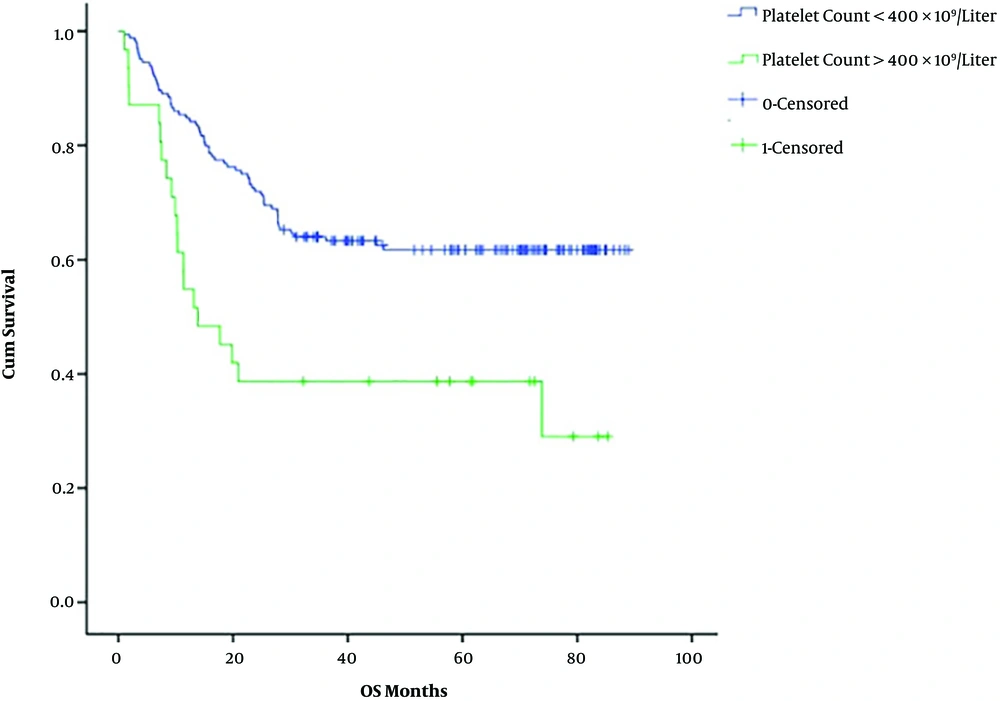
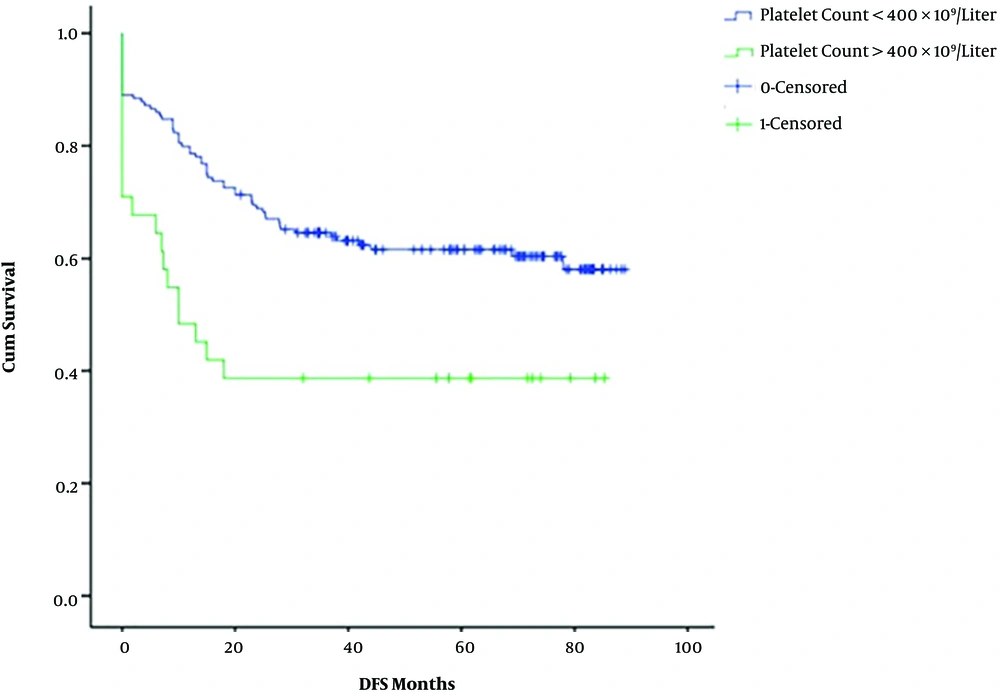
In the non-thrombocytosis group, 131 patients showed complete or partial response and 33 had stable or progressive disease. In the thrombocytosis group, 15 patients showed complete or partial response and 16 patients had stable or progressive disease. This study shows a significant association between platelet levels at diagnosis and the response to treatment (P value < 0.001). The 5-year-OS in the non-thrombocytosis group was higher (62%) than the thrombocytosis group (41%); similarly, the 5-year DFS was 61% and 39%, respectively. The OS and DFS had statistical significance in both arms (P value < 0.001) across platelet counts at diagnosis (Figures 1 and 2). In multivariate analysis, platelet counts greater than 400 × 109/liter and age less than 45 years had poor survival and other factors didn’t show any significance (Table 2).
| Variable | P Value | 0.95% Confidence Interval | |
|---|---|---|---|
| Lower | Upper | ||
| Age group | |||
| < 45 years vs. > 45 years | 0.006 | 2.503 | 233.106 |
| Cumulative chemotherapy received | |||
| > 250 mg vs. < 250 mg | 0.506 | 0.742 | 1.832 |
| Staging | |||
| II vs. III | 0.439 | 0.766 | 1.847 |
| Hemoglobin level | |||
| < 10 g% vs. > 10 g% | 0.553 | 0.426 | 1.580 |
| Platelets level | |||
| < 400 × 109/litre vs. > 400 × 109/litre | 0.004 | 1.290 | 3.784 |
Multivariate Cox Proportional Hazards Analysis of Variables That Could Impact the Survival
5. Discussion
Few studies on cervical cancer have assessed thrombocytosis as a prognostic indicator in patients receiving chemoradiation (5, 10-16). Two studies conducted by Sharma and Singh (14), Cheng et al. (15), in 2017, reported a positive correlation between thrombocytosis and poor outcome. We defined platelet count higher than 400 × 109/liter as thrombocytosis in our study. In this regard, most of the studies have considered the same cut-off (Table 3). Our intention was to assess thrombocytosis as a prognostic factor in Indian patients with cervical carcinoma.
| Study | No. of Patients | Treatment | Platelet Level Cut Off | Incidence of Thrombocytosis | Results | Significance | P Value |
|---|---|---|---|---|---|---|---|
| Hernandez et al. (4) | 113 | Radiotherapy alone | > 400 × 109/liter | 18% | The 5-year-survival for patients with normal platelet counts was 65%, whereas it was 25% for patients with thrombocytosis. | < 0.0001 | |
| Hernandez et al. (10) | 294 | Radiotherapy and concurrent hydroxyurea or misonidazole | > 400 × 109/liter | 30% | Thrombocytosis had a 55% greater chance of dying than those who had a normal platelet count. | Risk ratio: 1.55 95% confidence interval: 1.08 - 2.21 | 0.02 |
| Kawano et al. (12) | 286 | Radiotherapy with or without platinum-based concurrent chemotherapy | > 350 × 109/liter | 14% | Thrombocytosis is an independent predictor of compromised survival. | Hazard ratio of 1.65 for death95% confidence interval: 1.03 - 2.56 | 0.0395 |
| Lopes et al. (11) | 643 | Surgery or radiotherapy with or without chemotherapy | > 400 × 109/liter | 17% | The 5-year survival rate for patients with thrombocytosis was 57.1%, which was significantly worse than the 76.5% for those with normal platelet counts. | No significance on multivariate analysis | < 0.01 |
| Kozasa et al. (16) | 684 | Surgery or radiotherapy with or without chemotherapy | > 400 × 109/liter | 12.7% | Pre-treatment thrombocytosis and elevated PLR were identified as independent predictors in cervical cancer patients. | Elevated platelet count is a significant predictor of outcome on multivariate analysis |
Studies on Prognostic Significance of Thrombocytosis in Patients with Cervical Carcinoma Treated with Chemoradiotherapy
We observed thrombocytosis in 15.8% of the patients during diagnosis, which was similar to most of the published studies (4, 10-12), except for one by Hernandez et al. (10) where it was 30%.
Thrombocytosis was shown to be associated with advanced stages, bulky disease, and pelvic node positivity (10-12). Only Lopes et al. did not show any association of thrombocytosis with nodal positivity because most of the patients had early-stage disease where the incidence of nodal metastasis was low (11, 12). As all our patients had locally advanced disease, we found no correlation of thrombocytosis with age, stage, and pre-treatment hemoglobin levels. We did not evaluate correlation with the nodal status. A study by Kawano et al. (12) and Kozasa et al. (16) showed an association of thrombocytosis with young age (< 50 years) and low hemoglobin (< 11 g%), and only young age (< 50 years); however, no such correlation was seen in any of the other studies, including our study. Our findings revealed that there is a significantly better response to treatment in patients without thrombocytosis in comparison to thrombocytosis group (P value ≤ 0.001).
The patients with thrombocytosis had significantly poor OS and DFS of 41% and 39%, respectively at 5 years in our study. A similar trend was seen in all of the studies with chemoradiation (Table 3) (4, 10-12, 16). The first study by Hernandez et al., in 1992, showed a 5-year-survival advantage of 65% in non-thrombocytosis versus 25% in patients with thrombocytosis. Again in the year 2000, the same authors showed that patients with thrombocytosis had a 55% greater chance of dying than those who had a normal platelet count (4, 10). Kawano et al. also showed that patients with thrombocytosis had poor outcomes in terms of survival, with a hazard ratio of 1.65 for death (12). The recent study by Kozasa et al. showed an elevated platelet count was associated with poor OS and DFS. In addition, the authors showed elevated platelet/lymphocyte ratio was also associated with poor survival outcomes (16).
In our study, multivariate analysis showed that thrombocytosis is an independent prognostic factor (Table 3). Only Lopes et al. found no significant difference in survival when the patients were analyzed by the stage of the disease (11).
Irrespective of the platelet count at diagnosis, survival in young patients (< 45 years) is associated with poor outcome on multivariate analysis (Table 2), which is similar to the studies by Hernandez et al. (10), and Kawano et al. (12), who declared that the age less than 50 years was associated with poor outcome.
Most of the studies have shown that patients with thrombocytosis fail locally in comparison to systemically (12). The increased risk of local recurrence is probably due to poor response of the tumor to chemoradiation as seen in our study; also increased platelet counts have a role in stimulating tumor growth. However, platelet count may not influence the process of metastasis (17, 18).
The drawback of our study is that it is a retrospective study and the results need to be verified in a prospective trial. The cut-off value for thrombocytosis is variable ranging from 350 × 109/liter in Japanese studies to > 400 × 109/liter in European studies. We considered a platelet count > 400 × 109/liter to be the cut-off for this study similar to the most of the studies; however, there is no available confirming data regarding the same value for Indian patients. Nevertheless, to establish an optimal cut-off value for the platelets, we need larger and multicentral studies, containing patients from various ethnicities.
The data from our study and previous studies suggested that thrombocytosis could be a potential marker of prognosis, especially in patients with locally advanced and bulky diseases.
5.1. Conclusions
In conclusion, our study found thrombocytosis could be a potential prognostic marker in locally advanced cervical cancer treated with concurrent chemoradiation. We need further and larger prospective studies to categorize thrombocytosis as a prognostic factor for poor response.