1. Background
Radiotherapy plays an important role in the treatment of breast cancer, and its effects in reducing local recurrence have been proven (1). In breast conserving treatment, the breast radiotherapy is done after the surgery, and chemotherapy is administered in two steps with 50 Gy in 25 fractions firstly, followed by a boost of 10 - 20 Gy in 5 - 10 fractions to the tumor bed (2, 3). In performed trials, this boost dose has decreased local recurrence (1-3). Although most radiation oncologists are in agreement with the boost treatment, especially in patients with higher risks of recurrence, they have different ideas about the method to be used in terms of the type of beam (electron or photon) and the method of radiation delivery (4-7). Delivering the 10 - 20 Gy boost dose necessitates the accurate determination of the area and depth of the tumor bed. Additionally, the normal tissue of the breast is less exposed to radiation when the tumor bed is determined more accurately, and thus fewer consequent side effects appear. Different methods have been used to determine the tumor bed, including scar surgery, asking the patient to remember the mass, radiography, ultrasound, CT scan, and surgical clips (7-10). The accuracy of the aforementioned methods has been studied. There are different ideas about the accuracy of these methods in different studies. Although using surgical clips is not the best method, most studies have shown that it is the most appropriated one (11). The role of ultrasound in boost radiotherapy treatment has been widely studied, and different results have been obtained.
2. Objectives
The present study has investigated the accuracy of ultrasound in determining the depth of the tumor bed in comparison with using CT-clips.
3. Patients and Methods
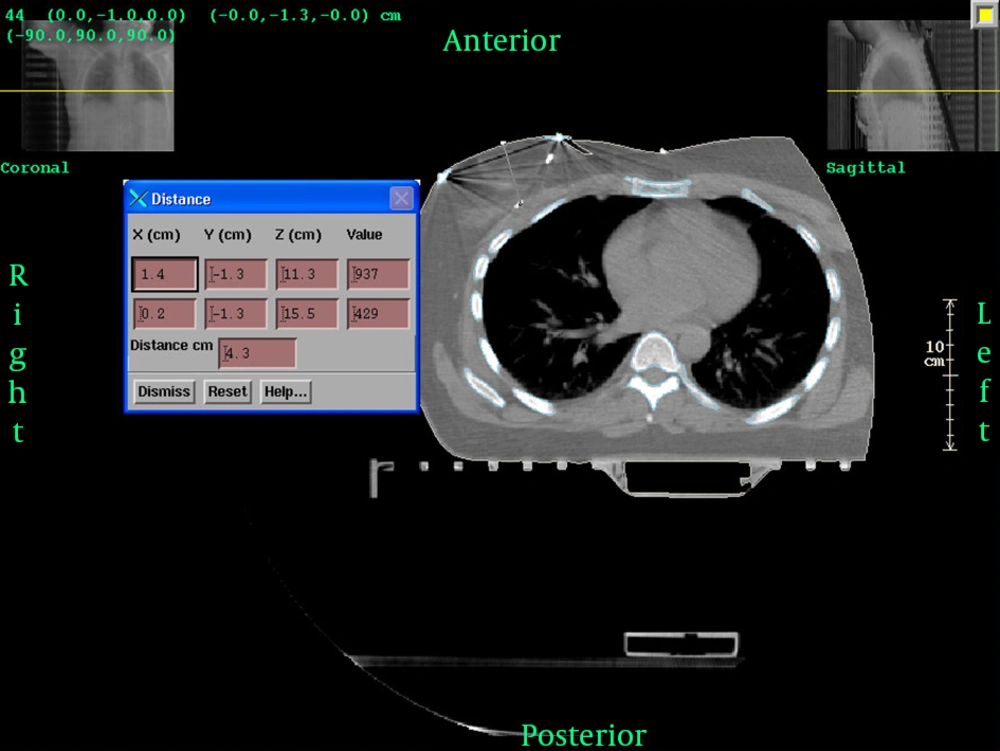
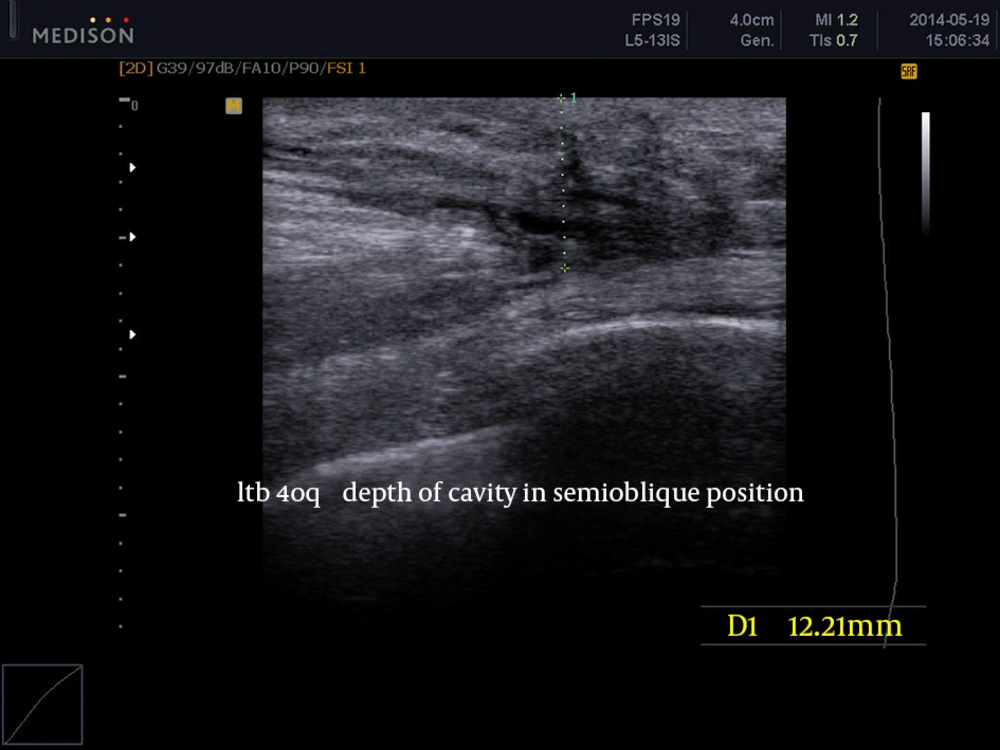
This study has been done in the radiotherapy-oncology department of a cancer institute. The inclusion criteria for cases were as follows: women who had undergone breast conserving surgery, more than 20 days passed from the date of the operation, and at least 5 titanium clips were placed by the surgeon in the upper, lower, medial, lateral, and floor areas of the tumor bed margins. Initially, the patient was requested to specify her tumor bed depth and its area on breast skin. The sonographist mentioned the depth of the tumor bed in all patients. It is noteworthy that all ultrasound tests were performed by a sonographist who was skillful in breast ultrasonography, and the ultrasound was done during the radiotherapy process. After the localization of the tumor bed by the sonologist in the skin, the boost field was defined by a 2.5 cm margin around the bed and a lead wire marker was placed on it. Then, the CT scan simulation (Siemens, SOMATOM Sensation 16) using the breast board (in radiotherapy treatment position) was performed. All scans were done with 5 mm slices from mandible angle to 2 cm under the breast. The planning was done using PCRT3D Activation software (manufacturer: tecnologo radiacion, version 6). In addition to treatment planning, the distance of the placed clips from tumor bed depth and the breast skin was measured (Figures 1 and 2).
Statistical method: the calculated sample size was 25 patients based on former studies and the sample size calculation relation in even data with the confidence interval of 95% (alfa = 0.05, z = 1.96) (12). The obtained results were analyzed using the SPSS software (version 20.0) and the hypothesis was tested using the paired t test.
4. Results
From January 2013 to February 2014, twenty five women were recruited for this study. The mean age of patients was 49 years (from a minimum age of 29 to a maximum age of 70). The most frequent cancer stages were stage I. The average time passed from surgery was 163 days with standard deviation of 64 days (minimum 27 days, maximum 263 days). 23 patients were under the adjuvant chemotherapy, and two of them had no indication for chemotherapy. The PTV (planning target volume) was 95 mL ± 45 mL (range 41 - 261 mL). The effects of time passed from surgery and chemotherapy on tumor cavity dimensions like depth and PTV, were also studied. The correlation between time passed from the surgery and PTV was not significant (P Value = 0.06). Also, no significant difference was observed between time passed from surgery with depths reported in ultrasound (P Value = 0.18) while the difference between the measured depths in CT scan with surgical clips was significant (P Value = 0.04). Since 23 patients out of 25 had undergone chemotherapy, the chemotherapy effect on cavity dimensions, including depth, was not evaluated in this research. The average depth reported from ultrasounds was 18 mm ± 3 mm (range: 10-26 mm), while the average depth measured from CT scan-surgical clips was 48 mm ± 13 mm (range: 24 - 80 mm). Almost in all cases, the depth reported from ultrasounds was less than that obtained from CT scan-surgical clips and in paired t test analysis; this difference was strongly significant (P Value = 0.001) (Table 1). Additionally, a positive and direct correlation was observed between depths obtained from ultrasonography and that obtained from CT scan- surgical clips (Pearson coefficient = 0.45), which is statistically significant (P Value = 0.027).
| Depth Obtained From CT Scan- Surgical Clips, mm | Depth Obtained From Ultrasound, mm | Patient Number |
|---|---|---|
| 15 | 1 | |
| 16 | 2 | |
| 16 | 3 | |
| 21.1 | 4 | |
| 18 | 5 | |
| 20 | 6 | |
| 21 | 7 | |
| 21 | 8 | |
| 10 | 9 | |
| 20 | 10 | |
| 18 | 11 | |
| 25 | 12 | |
| 20 | 31 | |
| 14 | 14 | |
| 20 | 15 | |
| 19.5 | 16 | |
| 17 | 17 | |
| 26 | 18 | |
| 25 | 19 | |
| 16 | 20 | |
| 19 | 21 | |
| 17 | 22 | |
| 25 | 23 | |
| 17.6 | 24 | |
| 21 | 25 |
The Measured Depth Observed Between Depths Obtained From Ultrasonography and That Obtained From CT Scan-Surgical Clips
5. Discussion
The present research has been performed to determine the accuracy of ultrasonography in the determination of the depth and area of the tumor bed in planning the radiotherapy boost for breast cancer, as the tumor depth is important for selecting the proper energy of electron beams. The efficacy of adjuvant radiotherapy in breast conservative therapy and boost to the tumor bed has been proven in least at 4 valid trials (EORTC BOOST TRIAL, LYON BOOST TRIAL, EBCTCG TRIAL, and NSABP TRIAL). The accurate determination of boost field is of much importance, since delivering the perfect boost to the tumor bed results in reduction of the risk of local recurrence; and also reduces the delivered dose to normal breast tissue and diminishes the side effects (1-3, 7, 13). The effect of variables like time passed from surgery and having chemotherapy or radiotherapy on the dimension and volume of the tumor cavity has been widely studied, indicating that these variables can affect the dimensions and also the cavity position (14-17). In this study, the correlation coefficient of time passed from surgery and tumor cavity dimensions (including depth and PTV) was demonstrated a relation between the measured depth based on CT scans with surgical clips and time passed from surgery. Although no significant relationship was observed between PTV and time passed from surgery, it was close to being statistically significant, which can be important medically. The reason for insignificance may be the limited number of samples and also high variety and distribution compared to other studies. In two separate studies, Sharma et al. (16) and Tersteeg et al. (14) have suggested that the CT scan treatment planning should be conducted again after the radiotherapy treatment of breast to treat the boost. The use of ultrasounds to determine the boost field of radiotherapy has been widely studied. Rabinovitch et al. (8) have compared the ultrasound and surgical clips for 29 patients, indicating that the ultrasound estimates less treatment volume and consequently less electron beam energy. Therefore, it should not be applied in determining the boost field, especially in patients receiving adjuvant chemotherapy treatment. Rabinovitch et al. (8) have measured the length, width, and depths of tumor using ultrasound in patients having surgical clips, showing that the tumor bed depth has been significantly underestimated by ultrasound in 23 out of 29 patients (8). Chitapanarux et al. (18) have considered 41 patients in 2009 using ultrasound with radiography to determine the tumor bed depth, indicating that the ultrasound underestimated the depth in 85% of patients (P Value = 0.27). In this work, the findings show that the determined depth by ultrasound is less than that estimated by surgical clips in almost all 25 patients. Thus, it can be concluded that ultrasonography is not an appropriate method to estimate the depth of boost field since it will result in using lower energy electron beams and insufficient coverage for planning target volume (PTV). The main reasons for the difference between depth measured with ultrasound and that of surgical clips include: having different criteria to determine the floor of tumor cavity by sonographists and surgeons, changes of dimension and tumor cavity position during the time elapsing since surgery, and the effects of chemotherapy on dimension and tumor cavity position (14-17). In fact, surgeons remove the normal breast tissue under the tumoral zone in addition to the tumor mass, then clean the zone to the pectoralis major muscle and place the posterior clips on the edge of the anterior fascia of the pectoralis muscle. The sonographists often observe the seroma in the cavity and measure its distance from the breast skin. Underestimating the depth potentially increases the chance for local recurrence because of insufficient boost dose. Additionally, it may cause cosmetic side effects by delivering higher doses to normal tissues.
Ultrasound is not an accurate method for planning the boost dose to breast and its use is discouraged. Treatment planning based on surgical clips and CT scan seems to be a better choice. We suggest that more comprehensive studies to be done on the cavity size and position changes as well as its dependence on radiotherapy, chemotherapy, and amount of time passed from surgery.