1. Background
Approximately 600,000 patients afflict annually with head and neck squamous cell carcinoma (HNSCC) worldwide (1). At the present time, locally advanced HNSCC (LAHNSCC) without metastasis is seen in sixty percent of patients. The most common pattern of recurrence is a locoregional failure, and most fatalities result from uncontrolled loco-regional or local disease. The preferred primary treatment approach for LAHNSCC patients is surgery with radiation therapy or chemo-radiation therapy. In HNSCC patients treated with radical intent, the recurrence is seen in 30% - 50% of the patients (2, 3).
Better local control can be achieved with maximum debulking surgery combined with a primary or a second new course of radiation therapy. External Beam Radiotherapy (EBRT) or High Dose-Rate Brachytherapy (HDR-BRT) can be used to deliver radiation therapy. Owing to the difficulty to spare adjacent normal tissues, which leads to undesirable late effects on the salivary glands, mandible, muscles of mastication, and serial structure spinal cord, re-irradiation for recurrent disease using EBRT is always challenging. In these cases, the use of intra-operative interstitial implantation is an option, as it is ideally suited to deliver a high dose to a limited volume with minimizing dose to normal structure due to rapid dose fall-off thus minimizing sequelae and improving local control (4). Also, HDR-BRT can increase total biological effective dose administered compared to the second course of EBRT, with decreased overall treatment time (5).
2. Objectives
Hence the feasibility in terms of toxicity and outcome of surgery followed by intraoperative interstitial-brachytherapy in recurrent head and neck cancer was studied.
3. Methods
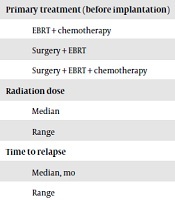
Institutional Medical Ethics Review Board approved the study protocol and consent procedure. Informed consent was taken. Ten biopsy-proven HNSCC patients with a mean age of 47 years (range 36 - 65 years) were analyzed. Surgery followed by chemoradiation therapy was given in 33% (3) of the patients and chemoradiation was given with cisplatin (weekly 40 mg/m2) in 77% (7) of the patients. Pre-brachytherapy patient characteristics are shown in Table 1.
| Characteristics | No. (%) |
|---|---|
| Gender | |
| Male | 10 (100) |
| Age, y | |
| Median | 45 |
| Range | 30 - 65 |
| Primary tumor and LN stage | |
| T2 | 4 (40) |
| T3 | 6 (60) |
| N0 | 1 (10) |
| N2 | 9 (90) |
| Primary tumor site | |
| Oropharynx | 2 (20) |
| Hypopharynx | 4 (40) |
| Oral cavity | 3 (30) |
| Parotid | 1 (10) |
| Primary treatment (before implantation) | |
| EBRT + chemotherapy | 6 (60) |
| Surgery + EBRT | 3 (30) |
| Surgery + EBRT + chemotherapy | 1 (10) |
| Radiation dose | |
| Median | 66 |
| Range | 60 - 70 |
| Time to relapse | |
| Median, mo | 12.1 |
| Range | 6 - 71 |
Patient Characteristics (N = 10)
Before re-irradiation, all patients were evaluated for eligibility and the following selection criteria were applied: histologic evidence of disease relapse, Karnofsky performance score (KPS) ≥ 80, no bony invasion by the tumor, and no evidence of distant metastases. These patients were at high risk of the second recurrence in view of a fixed node to the underlying structure.
Ten patients with locoregional recurrent disease underwent surgery followed by interstitial brachytherapy. Eight patients had neck nodal recurrence, which was stuck to the underlying structures and hence was considered high risk for recurrence even after surgical resection. Two patients with soft tissue recurrences at the BOT and Vallecula were considered for volume implant, where surgical clear margins were difficult to achieve. Nodal recurrence patients underwent Radical neck dissection (RND) and intraoperative catheter placement in the tumor bed in a single plane at 10 - 12 mm apart and stay sutures were placed to retain the catheters in their position. Subsequently, CT simulation with a slice thickness of 2.5 mm was performed on 5th or 7th postoperative day depending on the healing of surgical wounds. Major vessels of the neck were taken as organs at risk. Volumetric optimization method was used for planning with 5 mm dwell positions. Dwell timings over carotid vessels were minimized to prevent hyper dose sleeve. The dose of 30 Gy/10 fractions, 3 Gy/fraction, twice-daily fractions with 6 hours apart over 5 days was prescribed. Details of re-irradiation and implant characteristics are depicted in Table 2.
| Characteristics | No. (%) |
|---|---|
| HD-RBRT alone | 1 (10) |
| Surgery + HD-RBRT | 9 (90) |
| Implant location | |
| Neck | 10 (100) |
| Re-irradiation dose | |
| For all patients | 30 Gy/10 fr |
Details of Recurrent Disease and Implant Characteristics (N = 10)
3.1. Follow-Up
Overall follow-up ranged from 31 to 71 months (median 41 months) for survivors. Four patients reached a one-year follow-up. Two patients reached the three-year follow-up, 1 patient reached 5-year follow-up and 3 patients were alive at the time of reporting in April 2019.
4. Results
Statistical analysis was done using ‘R’ software ver.3.6.1 to calculate overall survival (OS) and disease-free survival (DFS).
4.1. Local Control
Over a median follow-up of 14 months, six patients developed local recurrence and one patient developed distant metastasis. The disease-free survival rates for the entire group in 1 and 2 years were 60% and 40%, respectively.
4.2. Overall Survival
The OS rate for the entire group was 60% and 40% in 1 and 2 years, respectively.
4.3. Toxicity
One patient had carotid blow-out who had disease stuck to the carotid and was managed with carotid embolization and doing well till today. Remaining 9 (90%) patients had grade I/II toxicity.
5. Discussion
Better local control can be achieved with debulking surgery in combination with primary radiation therapy or re-irradiation in recurrent loco-regional disease. In recurrent diseases, which are not amenable to surgery a low response rate of 50% - 60% and a median survival of 5 - 6 months is seen with chemotherapy (6, 7).
Re-irradiation using external beam therapy (EBRT) is limited by normal tissue complications caused by cumulative radiation doses. In RTOG 96-10, patients treated with EBRT and concurrent chemotherapy (5-fluorouracil and hydroxyurea) showed an overall survival of 41.7% and 16.2% at one and two years, respectively, with 7% grade V toxicity and 23% grade IV acute toxicity (8). In the RTOG 96-11 phase II trial of hyper-fractionated EBRT with cisplatin and paclitaxel, the OS at one and two years were 50.2% and 25.9%, respectively. The incidence of grade V toxicity was 8% and 23% was reported for grade IV acute toxicity. Osteonecrosis was noted in 5% of the patients (9). In our study, one (10%) patient had carotid blowout who had the disease stuck to carotid and remaining 9 (90%) patients had grade I/II toxicity.
Both trials showed high-grade IV and V toxicities for re-irradiation with EBRT. But toxicity may be reduced with the use of newer techniques like intensity-modulated radiotherapy (IMRT) for re-irradiation in recurrent HNSCC. Sulman et al. and Duprez et al. have reported OS of 35% to 58% at two years and LC of 64% to 65%, with 13% - 20% toxicity rate (10, 11). Roh et al. and Unger et al. reported 30% to 30.9% of OS and 41% to 52% of LC in 2 years, respectively, with late severe toxicity rate of 8.6% to 11% for re-irradiation using fractionated stereotactic radiotherapy (12, 13).
Recurrent head and neck cancers are less radio-responsive compared to primary non-irradiated cancer. Therefore, surgery followed by a sufficient dose of irradiation must be delivered to the treatment of a recurrent tumor. Using Brachytherapy high doses of radiation can be delivered to the tumor bed along with sparing the surrounding normal tissues. In our study, we could achieve local control as well as OS of 60% and 40% at one and two years, respectively, without significant acute or late toxicities.
The review of the literature shows that two-year local control of 31% - 69% and overall survival of 13% - 57% can be achieved with Low Dose-Rate Brachytherapy (LDR-BRT) in recurrent head and neck cancer (14-18).
Better dose distribution, dose homogeneity within the target area and radiation safety and patient comfort can be obtained with HDR-BRT compared to LDR-BRT. There are only a few retrospective studies published on the role of HDR-BRT in recurrent HNSCC (19-22). A study done by Hepel et al. in which 30 patients with recurrent head and neck carcinoma were treated with two daily fractions of 3 - 4 Gy to a mean dose of 34 Gy (18 - 48Gy) showed local control rate of 54% and 45 % and overall survival of 56% and 37%, respectively in 1 and 2 years. Nineteen percent non-cancer related deaths were noted (19). Tselis et al. showed OS and DFS rates of 42%, 19%, 6%, and 42%, 37%, 19%, respectively at 1, 2, 3 years in patients treated with HDR-BRT with a median dose of 30.0 Gy (12.0 - 36.0) Gy delivered at twice-daily fractions of 2 - 5 gray (21). A study on hyper fractionated interstitial HDR-BRT by Kolotas et al. in which patients received twice-daily fractions of 3 Gy/fraction to a total dose of 30 Gy in 37 of 49 patients and 36 gray in 12 of 49 patients showed local control rate of 69% and OS rate of 52%, 31%, 6% at 1, 2, 3 years, respectively (22). In another study done by Narayana et al., 30 patients were included in which 18 patients were treated with HDR-BRT using 3.4 Gy/fractions, two fractions per day to a total dose of 34 Gy followed by surgery, nine patients received HDR-BRT alone at 40 Gy (4 Gy/fraction two fractions per day) and three patients were treated with EBRT (40 - 50 Gy) and HDR-BRT (20 Gy, 4 Gy bid). The entire group showed an OS and local control of 63% and 71%, respectively in 2 years (20). In all HDR-BRT studies, the majority of patients were treated with daily fractions of 3 Gy for a total dose of 30 Gy or 4 Gy for a total dose of 40 Gy.
In our study, we could achieve a DFS of 60% and 40% in 1 and 2 years and OS of 60% and 40% in 1 and 2 years, respectively, with no significant acute or late toxicity even though nodes were stuck to tumor bed in our patients because they were at a high risk for the second recurrence. Six (60%) patients were locally controlled in 1 year. One patient had carotid blow-out who had disease stuck to the carotid vessel and was managed with carotid embolization. Hence, carotid should be carefully delineated and doses should be restricted with no hyper dose sleeve falling on carotids in the re-irradiation setting.
5.1. Conclusions
HDR interstitial brachytherapy in recurrent high-risk head and neck cancers with intraoperative placement of catheters at the tumor bed provides excellent local control by precisely defining the target volumes and conformal coverage of the target.