1. Background
The novel coronavirus (SARS-CoV-2), responsible for coronavirus disease 2019 (COVID-19), was first reported in Wuhan, China, in late 2019 (1). Considering the highly contagious nature of this disease, the world is now dealing with a global pandemic (2). The Centers for Disease Control and Prevention (CDC) reported a wide range of symptoms that may appear 2 - 14 days following exposure to the virus. These symptoms include fever or chills, cough, shortness of breath or difficulty breathing, fatigue, muscle or body aches, headache, loss of taste or smell, sore throat, nasal congestion, nausea or vomiting, and diarrhea (3). Asymptomatic or pre-symptomatic patients may be responsible for the transmission of SARS-CoV-2 (4).
This virus can spread via saliva or aerosol droplets produced through coughing, sneezing, speaking, or breathing (5, 6). It is known that infectious aerosols can remain suspended in the air for a long time (7). COVID-19 can also be transmitted through contact transmission or fomite transmission. This type of viral spread is through direct contact with an infected person or a contaminated object (8).
Since COVID-19 can be transmitted through various ways, it is crucial to pay serious attention to hygiene and sanitation in dental clinics. Patients and staff must practice regular hand hygiene with antiseptic solutions and use masks with pores smaller than 50 µm and appropriate goggles or face shields. In addition, the use of an antiseptic oxidative mouth rinse by the patient before and after every dental procedure is recommended (9). Face-to-face appointments in dental offices can be reduced by teledentistry (10). Due to the shortage/lack of global vaccine accessibility, the COVID-19 protective protocols must be followed rigorously (11).
Throughout the COVID-19 pandemic, radiography examination should only be considered for urgent dental procedures (2, 12). During intraoral radiography procedures, aerosols can be produced through potential gag reflexes and coughing induced by the placement of film holders. Therefore, extraoral radiography, including panoramic radiography and cone-beam computed tomography (CBCT), is recommended (6, 13). In this study, we evaluated the characteristics of patients who were referred to the Radiology Department of Shiraz University Dental School during the COVID-19 outbreak.
To the best of our knowledge, limited studies have been performed on this issue because of the unprecedented crisis caused by the COVID-19 pandemic.
2. Objectives
This study seeks to evaluate the necessity of prescribed intraoral radiographs and estimate the number of unnecessary prescriptions during the pandemic using a checklist. We hope that the presented findings can improve adherence to the pandemic guidelines in dentistry.
3. Methods
This cross-sectional study was approved by the local Ethical Committee of Shiraz University of Medical Sciences (code: #IR.SUMS.REC.1399.172). We used the convenience sampling method, which is a non-random, non-statistical method of sampling. Although there was a reduction in the total number of patients seeking dental care during the outbreak, all routine appointments were carried out as usual in the Department of Radiology, and all patients referred to us for radiography purposes were included in this study. A sample size of 97 individuals was calculated based on the expected prevalence of non-urgent radiographies (P = 50%), the estimation error of d = 10%, and the error rate of α = 0.05. However, to increase the accuracy of the results and reducing deviations, we increased the sample size to n = 143 people.
A total of 143 checklists were filled out using the information gathered from the patients referred to the Radiology Department of Shiraz University during the COVID-19 outbreak peak in July 2020. Informed consent was obtained from the participants. The checklist consisted of the following questions:
(1) Are you a confirmed or suspected COVID-19 patient who has recovered after treatment?
(2) Are you a confirmed or suspected COVID-19 patient with no symptoms?
(3) Have you recently shown any COVID-19 symptoms, such as fever, cough, fatigue, and vomiting?
(4) Have you been in contact with a confirmed or suspected COVID-19 patient recently?
(5) Are you suffering from any systemic diseases (according to the CDC, the risk factors include asthma, chronic lung disease, diabetes, sickle cell anemia, thalassemia, immunodeficiency disorders, liver disease, severe cardiac diseases, severe obesity, and people aged ≥ 65 years living in nursing homes or long-term care facilities)?
(6) What kind of radiologic imaging is prescribed for you?
(7) (A) Intraoral: Periapical (PA) or bitewing (BW); (B) extraoral: Panoramic (OPG) or CBCT (3D)
(8) What type of dental problem has brought you to the radiology department? (A) Prescriptions (pain/abscess/trauma/dentist’s call); (B) non-prescriptions (cosmetic reasons/new implant placement/checkups with no signs or symptoms).
(9) Which dental school department prescribed radiography for you? (A) Orthodontics; (B) pediatric dentistry; (C) periodontics; (D) prosthodontics; (e) oral and maxillofacial surgery; (F) oral and maxillofacial pathology; (G) endodontics; (H) public health dentistry; and (I) oral medicine.
For designing the checklist, we asked Yu et al. for their permission to use their questionnaire with some modifications to suit our purposes (14). We asked a team of experts, supervised by a radiologist, to translate it into Farsi. Then, we asked another group of language experts to back translate it into English to ensure that the main content was not lost. Afterward, the content and face validity of the checklist was assessed by a team supervised by a public dental health expert. We first asked 20 test subjects to complete the checklist and then asked them to complete it again later to ensure its reliability. We measured Cronbach’s alpha coefficient as one of the most commonly used reliability coefficients. In our assessments, Cronbach’s alpha coefficient was approximately 0.8; in other words, the questionnaire was reliable.
Moreover, the content relevance was examined by an expert panel that scored the relevance of each question from 1 to 4 (4 = the least relevant), and all the potentially irrelevant questions were removed. After revisions by the expert panel, the checklist was finalized. Using the checklist as a guide, we asked all the patients referred to us at the Radiology Department of Shiraz University during the COVID-19 outbreak peak in Shiraz for their information. The checklists were later filled out by an oral and maxillofacial postgraduate student based on the patients’ information and their referral papers from the respective departments.
The patients were classified based on age, gender, radiography technique (intraoral/extraoral), dental procedure (urgent/elective), systemic disease (high/low risk of COVID-19), and referring dental department. The necessity of referrals to the Radiology Department was determined based on the dental treatment demands. Any dental care procedure that could be postponed, such as aesthetic veneers, bleaching, and periodic dental checkups, was considered unnecessary, whereas abscess, pain, and follow-ups were described as necessary procedures (6).
3.1. Statistical Analysis
All the data were analyzed using SPSS version 22.0 (SPSS Inc., IBM Corporation, NY, USA). Chi-squared test and Fisher’s exact test were used to assess the relationships between the variables. A P-value of less than 0.05 was considered statistically significant.
4. Results
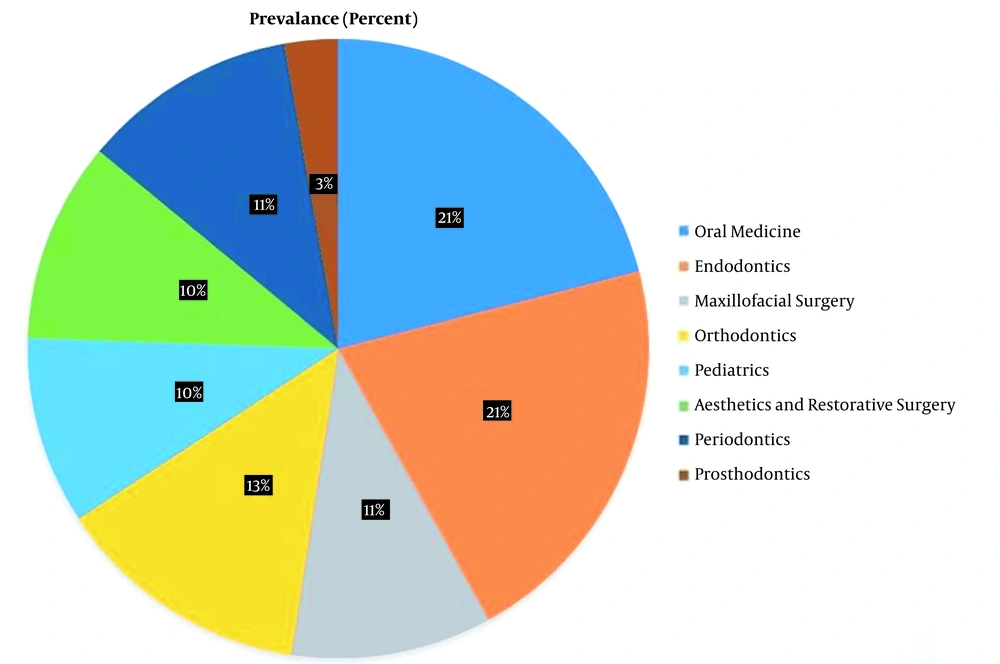
This study was conducted among 62 men and 81 women. The subjects were within the age group of 4 - 65 years, with a mean age of 29.36 ± 14.11 years. Eight patients with a history of systemic diseases, including asthma, diabetes, cardiovascular disease, and severe hypertension, were detected. Fever was not found in any of the patients. Figure 1 demonstrates the percentage of referred patients from various dental departments to the Radiology Department during the COVID-19 outbreak. Among all the patients, the endodontics and oral medicine departments had the highest percentage of referrals, followed by orthodontic, periodontology, aesthetics and restorative dentistry, maxillofacial surgery, pediatrics, and prosthodontic departments, respectively.
Table 1 presents the percentage of patients referred from each department based on the necessity of radiography prescriptions. The relationship between the necessity of radiography prescriptions and dental departments was significant (P = 0.001). Different departments prescribed diverse numbers of unnecessary referrals. The highest number of unnecessary referrals was from the Aesthetic and Restorative Dentistry Department (73.3%), followed by the departments of orthodontics (57.9%) and periodontics (56.3%), respectively. The lowest rate of unnecessary referrals was from the Department of Endodontics (13.3%).
| Departments | Urgent, % | Elective, % |
|---|---|---|
| Oral medicine | 53.3 | 46.7 |
| Endodontics | 86.7 | 13.3 |
| Maxillofacial surgery | 73.3 | 26.7 |
| Orthodontics | 42.1 | 57.9 |
| Pediatrics | 85.7 | 14.3 |
| Aesthetics and restorative surgery | 26.7 | 73.3 |
| Periodontics | 43.8 | 56.3 |
| Prosthodontics | 50 | 50 |
| Total | 60.1 | 39.9 |
Table 2 demonstrates a significant relationship between dental department and the type of radiography prescription. Of all the departments, the Orthodontics Department was the only one with more extraoral radiography prescriptions than intraoral prescriptions. All the other departments preferred intraoral radiography for their patients during the pandemic. Also, no extraoral radiography was prescribed by the Aesthetic and Restorative Dentistry Department. In addition, the relationship between the necessity of radiography prescriptions and the two variables of age and gender was evaluated, and no significant differences were found (P = 0.861 and P = 0.357, respectively). We found that one-third of all prescribed intraoral radiographs and half of extraoral radiographs were unnecessary, with a significant difference during the pandemic (P = 0.019).
| Departments | Intraoral, % | Extraoral, % |
|---|---|---|
| Oral medicine | 70 | 30 |
| Endodontics | 80 | 20 |
| Maxillofacial surgery | 60 | 40 |
| Orthodontics | 42.1 | 57.9 |
| Pediatrics | 64.3 | 35.7 |
| Aesthetics and restorative dentistry | 100 | 0 |
| Periodontology | 81.3 | 18.8 |
| Prosthodontics | 50 | 50 |
| Total | 70.6 | 29.4 |
5. Discussion
The COVID-19 pandemic has become a major public health concern, affecting every field, including oral and maxillofacial radiology (2). Due to continuous lockdowns worldwide, dental treatments have been limited to urgent cases (15). During the peak of the pandemic, of all the referred patients to the Radiology Department of Shiraz Dental School, the departments of endodontics (21%) and oral medicine (21%) had the highest percentage of referrals, followed by the departments of orthodontics (13.3%), periodontology (11.2%), aesthetics and restorative dentistry (10.5%), maxillofacial surgery (10.5%), pediatrics (9.8%), and prosthodontics (2.8%), respectively.
The present results are consistent with the findings of Yu et al. (14), which showed an increase in the percentage of endodontic emergency cases from 17.96% in 2018 and 13.47% in 2019 to 50.26% during the COVID-19 outbreak. The higher rate of referrals may be due to the fact that patients sought treatment for their dental emergencies more than unnecessary procedures that could be postponed. Also, the low referral number from the oral surgery department might be due to a decrease in the incidence of trauma during lockdowns.
In this regard, Hamedani and Farshidfar (2) suggested that only urgent conditions, such as facial and dentoalveolar traumas, fractured teeth or tooth pulp exposure, and hard or soft tissue infection treatments, should continue during the COVID-19 pandemic. Moreover, Cral et al. reported that dental emergency services, including dental extractions and pulpitis, must continue during the pandemic, while non-emergency dental treatments must be postponed (6). Despite the high rate of referrals from the Department of Endodontics, the lowest number of unnecessary radiography prescriptions (13.3%) was reported in this department, based on the mentioned classifications (2, 6).
One-third of all the prescribed intraoral radiographs and half of the extraoral radiographs in the present study were unnecessary during the pandemic. Although intraoral radiography has the advantage of superior resolution, there are numerous studies suggesting that intraoral radiography must be replaced by CBCT and panoramic radiography during the current pandemic (16-18). The Restorative Department had the most unnecessary radiography prescriptions, and all of the prescribed radiographs were intraoral, which is probably preferred due to its higher resolution (19). It is a significant dilemma for restorative specialists to decide which type of radiography to prescribe during this viral crisis.
The American Dental Association (ADA) also recommends avoiding or decreasing the prescription of intraoral radiography during the COVID-19 pandemic (11). Dentists around the world need to use the extraoral radiography approach as a substitute for intraoral radiography. Among all the departments included in our research, the Orthodontics Department was the only one with more extraoral radiography prescriptions than intraoral prescriptions, which was relatively expected since the Orthodontics Department usually requires/prescribes more extraoral radiographs. All the other departments preferred to prescribe intraoral radiographs for their patients despite the respiratory pandemic. Since the Oral Medicine Department is the first stop in patients’ admission, it requested more intraoral radiographs such as bitewings, and the associated results were relatively reasonable. In general, the more prescription of intraoral radiographs can be justified by the fact that extraoral bitewing radiography produces more false-positive results in proximal caries detection and alveolar bone loss, and CBCT has a higher effective dose with more artifacts (11, 13, 20).
Based on our findings, the association between the necessity of radiography prescriptions and dental departments was significant. Most dental departments prescribed some unnecessary referrals. The highest number of unnecessary referrals was related to the Department of Aesthetics and Restorative Dentistry, followed by the departments of orthodontics and periodontics.
Moreover, Currie et al. (21) reported a greater number of male patients seeking dental emergencies. On the other hand, in a study by Yu et al. (14), the same male-to-female ratio of patients was found for endodontic emergencies during the COVID-19 outbreak. In contrast to other studies, the present research included 62 males and 81 females. It was found that the relationship between the necessity of radiography prescriptions and age and gender was not significant.
In the current study, eight patients had systemic diseases with an increased risk of severe disease exacerbated by COVID-19 (22). These systemic diseases included asthma, diabetes, cardiovascular disease, and hypertension. Half of the patients sought urgent procedures, and the other half needed elective services. The results showed no significant link between the patients’ clinic attendance and systemic diseases. We suggest further studies with larger sample sizes for a better statistical evaluation of the relationship between systemic diseases and the patients’ visits to clinics during the COVID-19 outbreak.
To diminish the risk of transmission, we suggest that in addition to following the published radiography guidelines, dentists consult with radiologists before prescribing any radiographs. We also recommend that the Radiology Department should send a checklist to other departments containing easy-to-understand steps designed specifically for each department so they can follow and benefit from the guidelines.
Since Shiraz Dental School includes all the dental sub-disciplines and they all refer their radiography prescriptions to the Radiology Department, the obtained information from this study is comprehensive and can be generalized to other dental centers.
Statistically significant differences were found between some departments in terms of radiography prescriptions (intraoral/extraoral). However, due to the small sample size of this study, we could not compare all dental departments in terms of radiography types prescribed; thus, we suggest further studies with larger sample sizes in the future.
5.1. Conclusions
Despite rapid advances in the development of COVID-19 vaccines, several scholars believe that this pandemic cannot be easily eradicated due to the virus continuously changing through mutations. Therefore, until the complete eradication of the virus, it is essential to follow the established guidelines and postpone all unnecessary procedures for the safety of the community.