1. Introduction
Haemophilia is one of the hereditary recessive diseases linked to sex-induced coagulation disorder, which is characterized by bleeding episodes. In patients with hemophilia, bleeding occurs spontaneously or as a result of minor trauma. Joint arthropathy is one of the clinical manifestations of hand hemophiliac, which may be affected by repeated spontaneous joint bleeding. This study reported a rare case with a hemophilic pseudotumor of the distal phalanx.
2. Case Presentation
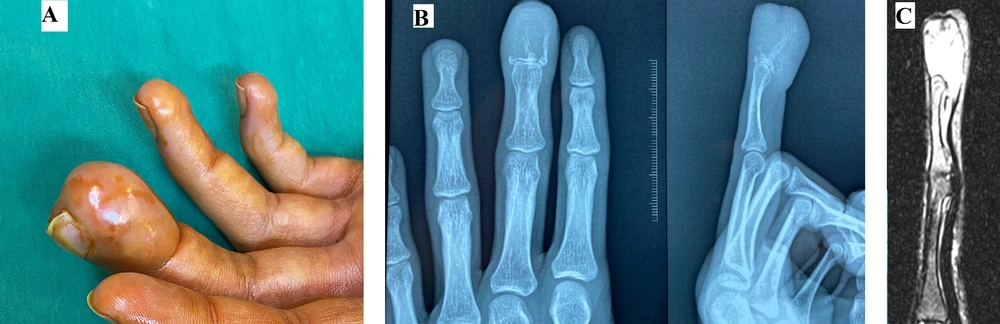
The distal phalanx of the left middle finger of a 21-year-old man was crushed in a closing door 18 months before. The distal phalanx was fractured, and a large hematoma developed under the nail plate, which separated the nail plate from its bed. The nail plate was surgically avulsed by a general surgeon elsewhere; however, pain and bleeding continued. One month later, he referred us, complaining of continuous pain and bleeding from his injured fingertip. The patient was not aware of his probable underlying bleeding tendency. Laboratory tests demonstrated an increased activated partial thromboplastin time to 56 seconds (normal ≤ 30 seconds). Further laboratory tests also demonstrated that the levels of von Willebrand factor were 35 IU/dL (normal 100 IU/dL; range 50 - 200 IU/dL), and clotting factor VIII activity was 9% (normal value ≥ 50%). His unknown bleeding disorder was diagnosed as a case of von Willebrand disease (VWD). Noteworthy, the levels of blood clotting factor VIII activity are usually parallel with those of the von Willebrand factor, explaining their parallel reduction. Moreover, the laboratory findings ruled out the infection and osteomyelitis in the distal phalanx based on an erythrocyte sedimentation rate (ESR) of 24.3 mmol/h and the C-reactive protein (CRP) of 4.5 ng/mL. The patient was treated with the replacement of von Willebrand factor and factor VIII, but the distal phalanx demonstrated progressive swelling (Figure 1). Eighteen months after the injury, plain radiographs demonstrated an expansile lesion with extensive destruction of the distal phalanx (Figure 1). Magnetic resonance images also revealed a well-defined and encapsulated cystic lesion with the dimension of 27 × 17 × 16 mm3 at the distal phalanx with low signal density on T1 images and high signal intensity on T2 images (Figure 1). Regarding the patient’s history and abnormal clotting tests, the development of a hemophilic pseudotumor was considered at the distal phalanx because of the enlarging nature of the coagulum that induced compression and pressure necrosis on the adjacent bone and structures. Regarding the isolated distal phalanx involvement and patient history, there was no need for an initial biopsy. Given the extensive destruction of the distal phalanx, the medical team offered and performed distal phalanx amputation under the cover of adequate levels of von Willebrand factor and factor VIII. Histopathological examination was compatible with a hemophilic pseudotumor of the distal phalanx.
(A) Eighteen months after the injury, the distal phalanx of the middle finger was deformed and swollen; (B) 18 months after the injury, anteroposterior and lateral radiographs demonstrated extensive destruction of the distal phalanx. (C) MRI T2 images of the lesion demonstrated high signal density.
3. Discussion
Musculoskeletal complications of the hand are rare in the hemophilia patient; however, hemarthrosis, synovitis, arthropathy of the small joints of the hand, hemophilic cysts, hemophilic pseudotumors, carpal tunnel syndrome, vascular aneurysms, and vascular pseudoaneurysms have been reported (1-3).
The incidence of hemophilic pseudotumors among hemophilic patients has been estimated at 1.14%. Most hemophilic pseudotumors have been reported in the proximal skeleton. The incidence of hemophilic pseudotumors in the small bones of the hand has been rarely reported (1-4).
The main differential diagnosis in similar cases is the infection presented with osteomyelitis and malignancy. Based on the literature, the hand tumors, most of them are benign, and a large number of them presented without any pain or tenderness. Metastatic tumors are very rare in hand, especially in osseous tissues. The malignant lesions are most commonly presented by pain, swelling, and nail deformity. Chondrosarcoma is the most common non-metastatic malignant bony tumor of the hand and is usually recognized as the secondary chondrosarcoma in previous Ollier's disease. It is presented with a painful lytic lesion with popcorn calcification in small tubular bones of the hand (5), so that the primary evaluation is important to rule out primary malignancy and infection.
Non-surgical treatments of hemophilic pseudotumors include aspiration of lesions and fibrin injection, embolization of the bleeding vessel, and radiotherapy (1-4). Embolization is not an appropriate solution for hand lesions due to the potential for vascular compromise (1). Radiotherapy induces inflammation and fibrosis of blood vessels; however, this option should be selected with caution as the stiffness and neuropathy following irradiation can affect the function of the hand (1-4).
Failure of non-surgical treatment and extensive lesions are among the indications of surgical excision of the hemophilic pseudotumors. Thomas et al. expressed that the hemophilic pseudotumors larger than 3 cm in diameter did not respond to nonsurgical management (2).
VWD affects 0.6 to 1.3% of the population. It is the most prevalent hereditary bleeding disorder. (3). The current case is the development of a hemophilic pseudotumor in the hand of a patient suffering from a very rare VWD complication.