1. Background
Prematurity is the most common cause of neonatal death, resulting in approximately 80% of the deaths of infants without congenital abnormalities (1). The low birth weight (LBW) rate has increased because of an increase in preterm births (2). LBW neonates are sub-grouped according to the degree of smallness at the first weight determination after birth: LBW, < 2500 g; very low birth weight (VLBW), < 1500 g; and extremely low birth weight (ELBW), < 1000 g. LBW is caused by preterm birth, intrauterine growth restriction (IUGR), or both. LBW infants are 40 times more likely to die than infants with normal birth weight, and VLBW infants are 200 times more likely to die (2). The improvement in survival rates of preterm infants has been well-documented over past two decades (3, 4). Following the widespread use of antenatal steroids and surfactants, a marked reduction in the mortality rate has been reported (5). However, the survival and outcomes of preterm neonates in different regions vary widely. Hence, outcome studies on preterm infants in each population and region are essential (5).
With the development of new therapies, the surveillance of up-to-date patient outcomes is essential in monitoring the effectiveness of current practices (6). Although some evidence has shown that mortality in high-risk infants is more closely related to gestational age than to birth weight (7-9), a combination of both variables may provide an even more accurate prediction of outcome (10). Despite the apparent importance of LBW as an indicator, there have been few studies of outcomes for LBW infants in developing countries.
2. Objectives
The main objective of the present study was to determine neonatal mortality of infants weighing less than 2500 g at birth.
3. Patients and Methods
This retrospective study was conducted in the neonatal intensive care unit (NICU) of a referral hospital (Izadi Hospital) in Qom, Iran, over a period of 48 months from March 2010 to February 2014. The outcome measure was the number of hospital deaths. Survival was defined as the discharge of a live infant from the hospital within 75 days.
All newborns weighing less than 2500 g who were admitted to the aforementioned NICU were included in the study. Newborns with congenital anomalies and those who were discharged voluntarily by their parents were excluded. The collected data included age of mother, type of delivery, neonate sex, vital condition of newborn upon delivery, birth weight, gestational age, details of morbidities, and mortality during the hospital stay (if any). If an infant died before discharge from the hospital, an immediate verbal autopsy was sought and the diagnosis was confirmed by the attending doctors. Gestational age was calculated using the first day of the last normal menstrual period, and also estimated by obstetric sonography and the Ballard score.
SPSS for Windows (version 21) was used for data analysis. The Kaplan-Meier method was used to estimate the survival of infants during the hospital stay and the survival function from lifetime data. P values of less than 0.05 were considered to indicate statistical significance.
The Ethics Committee of Qom University of Medical Sciences, Qom, Iran, approved this study.
4. Results
There were 33,020 live births at the hospital over the 4-year study period, including 798 infants who met our inclusion criteria. Of these, 115 (14.4%; 95% CI = 11.9% – 16.8%) died during their hospital stay. Increased birth weight and gestational age were associated with decreased mortality (Table 1).
| Variables | Number of Infants | Number of Deaths (95% CI) | P Value |
|---|---|---|---|
| Birth weight, g | <0.001 | ||
| < 1000 | 108 | ||
| 1000 - 1499 | 221 | 35 (11.1 - 20.3) | |
| 1500 - 2499 | 469 | 26 (3.5 - 7.6) | |
| Gestational age, w | <0.001 | ||
| ≤ 30 | 255 | 79 (24.8 - 36.8) | |
| 31 - 34 | 398 | 26 (4.2 - 9.2) | |
| 35 - 39 | 145 | 10 (3.1 - 11) |
Overall, 48 of 384 girls (12.5%; 95% CI = 9% – 16%) and 67 of 414 boys (16.2%; 95% CI = 12.5% – 19.7%) died. The higher mortality rate in males than in females was not statistically significant (P = 0.139). The deaths included 43 of 212 (20.3%; 95% CI = 15.5% – 26%) infants born by normal vaginal delivery and 72 of 586 (12.3%; 95% CI = 9.7% – 15%) born by cesarean section (P=0.004).
Overall, death occurred in 39.2% (95% CI = 32% – 46.2%) of newborns with a first-minute Apgar score of ≤ 5/10, and in 6.2% (95% CI = 4.2% – 8.2%) of those with a first-minute Apgar score of > 5/10 (P < 0.001), as well as in 54.4% (95% CI = 44.6% – 63.2%) of infants with a 5-minute Apgar score of < 7/10 and in 7.7% (95% CI = 5.8% – 9.8%) of those with a 5-minute Apgar score of ≥ 7/10 (P < 0.001).
Neonatal illnesses were documented in 620 infants (Table 2). The most frequent illness was respiratory distress syndrome (RDS).
| Illness | LBW Infants (n = 798) | VLBW Infants (n = 329) | ELBW Infants (n = 108) | |||
|---|---|---|---|---|---|---|
| Frequency 95% CI | Mortality Rate, 95% CI | Frequency 95% CI | Mortality Rate, 95% CI | Frequency 95% CI | Mortality Rate, 95% CI | |
| RDS | 559 (66.8 - 73.4) | 16.8 (13.8 - 19.9) | 273 (78.7 - 86.9) | 29.3 (23.9 - 35) | 98 (84.8 - 95.5) | 52 (41.6 - 62.1) |
| Septicemia | 74 (7.2 - 11.5) | 18.9 (10.6 - 27.9) | 40 (8.6 - 15.7) | 32.5 (18.6 - 47.6) | 13 (5.9 - 18.9) | 38.5 (12.5 - 66.7) |
| PDA | 135 (14.3 - 19.6) | 23.7 (16.2 - 31.3) | 88 (21.9 - 31.6) | 30.7 (21.6 - 40.2) | 32 (21 - 38.3) | 43.8 (26.5 - 61.3) |
| IVH | 35 (3 - 5.9) | 5.7 (0 - 14.3) | 25 (4.7 - 10.7) | 4 (0 - 13.3) | 8 (2.8 - 12.8) | 0 |
| Asphyxia | 10 (0.5 - 2) | 40 (10 - 75) | 4 (0.3 - 2.5%) | 50 | 0 | NA |
| Pneumothorax | 78 (7.9 - 11.8) | 43.6 (32.5 - 54) | 55 (12.5 - 20.5) | 30 (40.9 - 67.4) | 23 (13.5 - 28.9) | 65.2 (42.9 - 85) |
| IUGR | 137 (14.7 - 19.8) | 12.4 (7 - 18.4) | 62 (15 - 23.6) | 19.4 (9.8 - 30.3) | 16 (8 - 22.1) | 43.8 (20 - 70.6) |
Abbreviations: IVH, intraventricular hemorrhage; IUGR, intrauterine growth restriction, NA, not available; PDA, patent ductus arteriosus; RDS, respiratory distress syndrome.
Umbilical vein catheters and chest tubes were used, respectively, in 40 (5%; 95% CI = 3.5% – 6.5%) and 66 (8.3%; 95% CI = 6.5% – 10.3%) of the 798 infants. The mortality rate in infants without umbilical vein catheters was 14% (95% CI = 11.4% – 16.5%), and in infants with umbilical vein catheters, it was 22.5% (95% CI = 10.5% – 37.5%). The mortality rates in the two groups were not significantly different (P = 0.135).
The mortality rate in infants without chest tubes was 12% (95% CI = 9.7% – 14.5%) but in infants with chest tubes, it was 40.9% (95% CI = 28.3% – 52.7%), which was significantly higher (P < 0.001).
Of the 261 (32.7%; 95% CI = 29.6% – 35.9%) infants who received ventilators, the mortality rate was 32.6% (95% CI = 26.8% – 38.4%), while in those who did not receive a ventilator, it was 5.6% (95% CI = 3.7% – 7.5%) (P < 0.001).
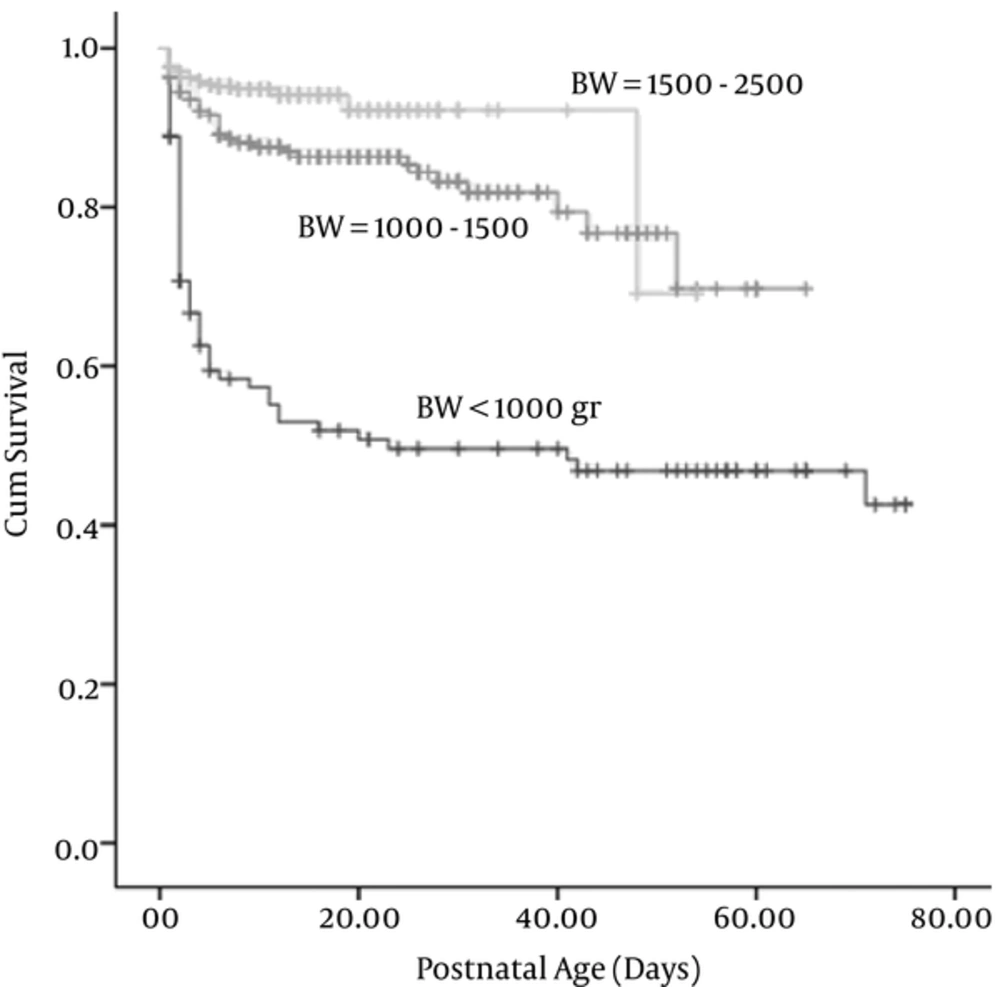
The survival time of infants was investigated with the Kaplan-Meier method. The average age at the time of death was 7.65 days, with a standard error of 12.25 days (95% CI = 5.46 – 9.93). It is expected that 75% of infants would survive after 52 days. The survival rates of newborns in different birth weight groups were significantly different (P < 0.001) (Figure 1).
An Apgar score of < 7 at 5 minutes had the highest effect on survival, with an odds ratio of 8. A first-minute Apgar score with an odds ratio of 2.2 had a greater effect on survival than birth weight and gestational age (Table 3).
| Characteristic | Birth Weight | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| < 2500, g | < 1500, g | < 1000, g | |||||||
| Odds Ratio | 95% CI | Odds Ratio | 95% CI | Odds Ratio | 95% CI | ||||
| Cesarean Section | 0.983 | 0.575 | 1.678 | 1.540 | 0.769 | 3.086 | 1.937 | 0.649 | 5.785 |
| Female | 0.770 | 0.477 | 1.242 | 0.824 | 0.450 | 1.506 | 1.137 | 0.426 | 3.038 |
| Apgar < 5 at 1 minute | 2.371 | 1.276 | 4.406 | 1.539 | 0.706 | 3.355 | 0.715 | 0.183 | 2.797 |
| Apgar < 7 at 5 minutes | 4.217 | 2.232 | 7.969 | 3.874 | 1.792 | 8.376 | 9.208 | 2.588 | 32.764 |
| IUGR | 1.086 | 0.582 | 2.029 | 1.227 | 0.477 | 3.158 | 2.749 | 0.573 | 13.187 |
| Gestational age | 0.931 | 0.813 | 1.065 | 0.856 | 0.705 | 1.039 | 0.715 | 0.501 | 1.020 |
| Birth weight | 0.999 | 0.998 | 1.000 | 0.998 | 0.996 | 1.000 | 0.998 | 0.994 | 1.002 |
5. Discussion
Neonatal death is a serious concern in both developed and developing countries. While overall infant mortality rates have been decreasing worldwide, changes in neonatal mortality rates have occurred much more slowly (11).
In our study, the mortality rate in LBW infants (14.4%) was similar to that reported by other studies (14%–18.7%) (12, 13). The mortality rate in the VLBW neonates (27%) was less than in other Iranian studies that have reported a prevalence of 50%–64% (12, 14), and similar to or less than that reported in studies from other countries (15, 16). In the ELBW infants in our study, the mortality rate was 54%, which was less than in other studies that have reported a prevalence of 68% – 94% (14, 17).
In Yazd, Iran, 18.7% of LBW infants, 50% of VLBW infants, and 94 % of ELBW infants die (12). In Italy, the mortality rate for VLBW infants was reported as 19.6% (18). In a study from New Delhi, India, the neonatal mortality rate until discharge was 15.7% in the VLBW group and 33.3% in the ELBW group (19), while in Thailand, the survival rates for VLBW and ELBW infants were reported as 81% and 52%, respectively (20). In Sao Paulo, Brazil, for birth weights of 500 – 749 g, 750 – 999 g, 1000 – 1249 g, and 1250 – 1499 g, the survival rates in the year 2000 were 15%, 71%, 93%, and 96%, respectively (21).
The frequency of neonatal illness in our study was similar to that reported by others. In one study, the rates of RDS, septicemia, and asphyxia in LBW infants were reported to be 59%, 12%, and 20%, respectively (12). In our study, the frequency of RDS in the VLBW infants was more than in other studies, which reported a prevalence of 43% – 76%. However, the frequency of septicemia, patent ductus arteriosus, and intraventricular hemorrhage was lower in our study than in others, which reported rates of 22% – 34%, 34% – 44%, and 3% – 27%, respectively (5, 14, 22).
The Kaplan-Meier method was used to assess the survival of VLBW infants in one previous study; the result was 50% on the second day of the hospital stay and 25% on the 14th day (23). The survival rate of VLBW neonates in our study was approximately 75% on the 16th day of the hospital stay. Consistent with other studies, mortality declined with increased birth weight, gestational age, and Apgar score (11, 14), but not with statistical significance.
A previous study documented higher mortality in male neonates (6); in the present study also, the mortality rate of LBW and VLBW infants was higher in males than in females. The difference was not statistically significant, but might be of clinical importance. In our study, the mortality rate in LBW infants born by normal vaginal delivery was higher than in those delivered by cesarean section, but the mortality in VLBW and ELBW infants delivered by cesarean section was higher than in those delivered by normal vaginal delivery. This may be of clinical concern, but it is not statistically significant. Vaginal delivery has been reported to be significantly associated with intraventricular hemorrhage (5), and other studies (24, 25) have found a lower VLBW mortality rate for infants delivered by cesarean section.
The varying survival rates of LBW infants are dependent upon the resources and caretaker experience in the NICU (26, 27), and increased infant mortality is associated with substandard neonatal care and early neonatal factors (28).
In conclusion, our study showed that the mortality rate of LBW infants was low compared to other studies in Iran; nevertheless, early deaths of ELBW infants are common in our hospital. The current improved survival rates compared to the past may be the result of enhanced perinatal and neonatal care, improved standard resuscitation protocols, and increased administration of antenatal steroids and surfactants.