1. Background
Tuberculosis (TB) is an infectious disease and a major healthcare problem worldwide. It is recognized as one of the major causes of mortality in developing countries (1). According to reports by the World Health Organization (WHO), about two billion people around the world have been infected with TB, and 10 to 20 million new TB cases are added to this number annually, 95% of which is attributed to developing countries (1-3). Nearly 1.3 million children are infected with TB every year around the world, and 450000 children die annually due to TB (2-4). Based on WHO reports, one billion people will be infected with Mycobacterium tuberculosis by the end of 2020 (3-5).
TB is more prevalent in marginal areas, and the highest rate has been reported in Sistan and Baluchestan Province (6-8). This province has shown the highest rate and incidence of TB in the country in the past years (2, 6). The overall incidence of TB in the province is estimated at 109.7 per 100000 people, and the incidence of smear-positive TB is 64.3 per 100000 people (6, 8). Accurate and complete treatment and management of TB are the most important approaches for the control and prevention of this disease (7-9).
2. Objectives
The aim of the present study was to monitor and evaluate program performance and management control system of TB in Sistan and Baluchestan Province by comparing the annual indicators over ten years.
3. Methods
This cross-sectional, descriptive study was performed, using census sampling method. The data of TB patients (indicators of national TB control), which were recorded in the health department of Sistan and Baluchestan Province from January 2006 to January 2016. This study was approved by the Research Ethics Committee of Islamic Azad University of Medical Sciences, Tehran, Iran. SPSS version 23 was used for data analysis, and scatter plots and linear regression models were applied.
4. Results
According to the information on the provincial TB control system, an improving trend was observed in almost all indicators, especially regarding smear-positive pulmonary TB and new cases of smear-positive pulmonary TB. It represents a downward trend with a negligible slope for completion of treatment for new extra pulmonary and smear-negative patients during 2006 - 2016.
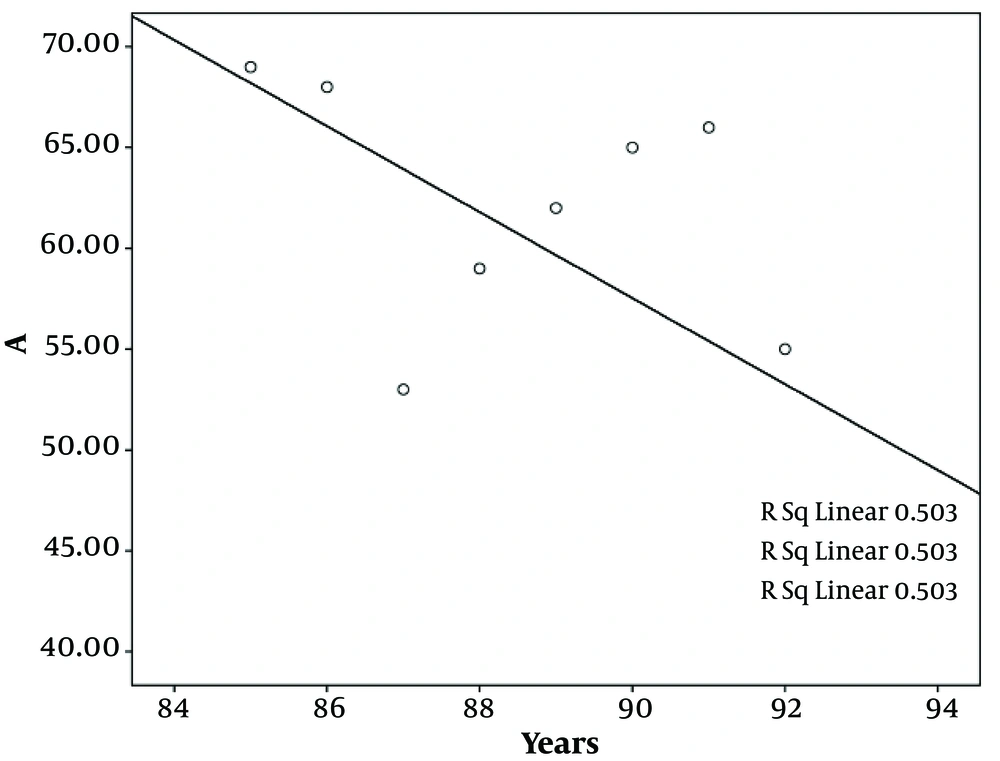
The middle line in the Figure 1 indicates the results of the current system and represents a downward trend, with a relatively high incidence of new smear-positive pulmonary TB during 2006 - 2016. The results of this study shows a downward trend in TB-related mortality during 2006 - 2016.
5. Discussion
The findings confirm that by DOTS strategy, the rate of treatment success increases. Our findings showed that the success of management system in case detection followed a downward trend in Sistan and Baluchestan Province during 2006 - 2016. The success rate of management system was significant in reducing the incidence of new smear positive TB cases in Sistan and Baluchestan during the evaluated period.
Also, the results of this study showed that an increase in per capita income, per capita expenditure on health, per capita expenditure on education, per capita expenditure on sports, reduced smoking, and marriage could have positive effects on the reduction of TB risk. On the other hand, the results showed that simultaneous HIV infection, delayed treatment, poverty of households, lack of access to health facilities, smoking and alcohol, mismanagement of daily activities, and illiteracy increased the mortality rate and reduced the success of TB treatment (4, 8, 10).
Abbreviation: EMRO, Eastern Mediterranean Regional Office.
aPer 100000 general population.
bValues are expressed as No. (%).
The findings showed that other factors, such as age, alcohol consumption, tobacco use, improper nutrition, and lack of access to health facilities and local medicines increased the rate of treatment failure and reduced the success of TB treatment (3, 7). The middle line of the Figure 1 shows the results of the current system and indicates a completely downward trend in TB recurrence during 2006 - 2016. Dooley et al. showed that the success rate of TB treatment increases by implementing DOTS strategy (9).
Evaluation of the success rate of management systems in reducing the number of treatment-resistant TB cases in Sistan and Baluchestan Province during 2006 - 2016 showed a promising trend. The global problem of drug resistance and possible diagnostic issues in Iran indicate the necessity of case detection and proper treatment to improve the conditions. Adineh showed the highest resistance to isoniazid, while PCR assay was found to be an appropriate method for identifying strains sensitive to isoniazid and rifampin (11-13). Some studies suggest that important factors of treatment failure include positive sputum smear in two months after TB and poverty; this finding is almost consistent with the present study (14-16).
Panickar and Hoskyns showed latent TB infection with three months of rifampin-isoniazid treatment was a major part of the TB prevention program (15). The results of this study indicated an acceptable reduction in the incidence of TB treatment failure after treatment of latent TB infection with a rifampin-isoniazid regimen for three months; the results of this study are somehow similar to those of the present study.
5.1. Conclusion
This study showed that TB can be eliminated through correct implementation of DOTS strategy, implementation of educational and tuberculosis drug programs, and execution of correct management policies. The DOTS strategy is also suggested as the most reliable method for confronting drug resistance and recurrence of TB.