1. Background
Tuberculosis (TB), as a reemerging disease, is known as a major global health problem (1). It was the second leading cause of death from infectious diseases and among top 10 causes of death worldwide in 2015 (1). The world health organization (WHO) introduced the “End TB Strategy” in May 2014 as one of the most important health targets of sustainable development goals to promote the downward trend of global TB mortality by 2030 (2).
Evidence has revealed the importance of adequate physician knowledge and practice regarding the diagnosis and treatment of TB (3, 4). In fact, rapid and accurate diagnosis of TB is important in preventing disease transmission and mortality (5). A systematic review by Van der Werf et al. in 2012 indicated the adequate knowledge of healthcare workers about anti-TB drug treatments, including duration of treatment and drug dosage (3). Moreover, another study showed that the most important cause of the emergence of multidrug-resistant TB (MDR-TB) is irrational prescription of drugs by physicians (6).
2. Objectives
There are some studies, which aimed to measure the knowledge, attitude, and practice (KAP) of medical students and general practitioners (GPs) about TB. However, to the best of our knowledge, the present study is the first longitudinal research in Iran, which aimed to examine both knowledge and practice of medical students before and 2 years after education.
3. Methods
This interventional study was conducted between 2014 and 2016 at Shiraz University of Medical Sciences (SUSM), Shiraz, Iran. The knowledge and practice of 60 final-year medical students about national TB guidelines were assessed before education, 1 month after education, and 2 years after education at the Tuberculosis Center of SUMS. We reached a sample size of 60 (alpha, 0.05; beta, 0.2; knowledge score difference, 1.6; standard deviation, 3.1) according to a pilot study before and 1 month after training of 15 students.
Every month, 10 to 15 students were referred from the department of community medicine to the Tuberculosis center, affiliated to SUMS. First, students referred to the TB center were asked to complete a questionnaire, which consisted of 18 questions on knowledge (10 questions) and practice (8 questions) of national TB guidelines. After 1 month, they were asked to complete the questionnaire again. In addition, the students were contacted through E-mail and phone calls to fill out the questionnaire 2 years after graduation.
The third questionnaire was similar to the main questionnaire, except that it included any type of training about TB, besides strategies for TB-suspected patients after graduation. The content validity of the questionnaire was confirmed by infectious diseases specialists and the TB coordinator of the province. The reliability of the questionnaire was also estimated at 62% (Cronbach’s alpha). The only exclusion criterion was unwillingness to participate in the study. Level of knowledge and practice ≥ 50% was considered acceptable.
In this study, parametric (independent t test) and nonparametric (Chi square and Mann-Whitney U) tests were applied in IBM SPSS version 20. The accuracy of data entry was assured by comparing the data of the completed questionnaires versus the corresponding data in SPSS. P value less than 0.05 was considered statistically significant.
3.1. Ethics Statement
Consent to participate in the study was obtained from the participants, and confidentiality of the data was respected. The study protocol was approved by the ethics committee of SUMS with the registry number, 14192.
4. Results
A total of 60 medical students participated in this study. The mean age of the students was 24 ± 1.5 years. The male-to-female ratio (n, 27; 45% vs. n, 33; 55%) was 0.81. The mean time from the internship period was 7.1 ± 4.4 months, and the median interval was 6.5 months. Thirty-two (53.3%) students stated that they had attended the infection ward during their clinical course, although no significant difference was found between male (15/27; 55.5%) and female (18/33; 54.5%) students (P = 0.9).
Thirty-four (56.7%) students reported that they had visited patients who were suspected of TB after graduation from university. Based on the results, 13 (21.7%), 4 (6.7%), and 3 (5%) participants had passed a type of TB training, i.e., reading the national TB guidelines, participation in workshops, and virtual learning, respectively. On the other hand, 9 (15%) subjects reported other types of learning, and 31 (51.7%) did not report any type of TB training.
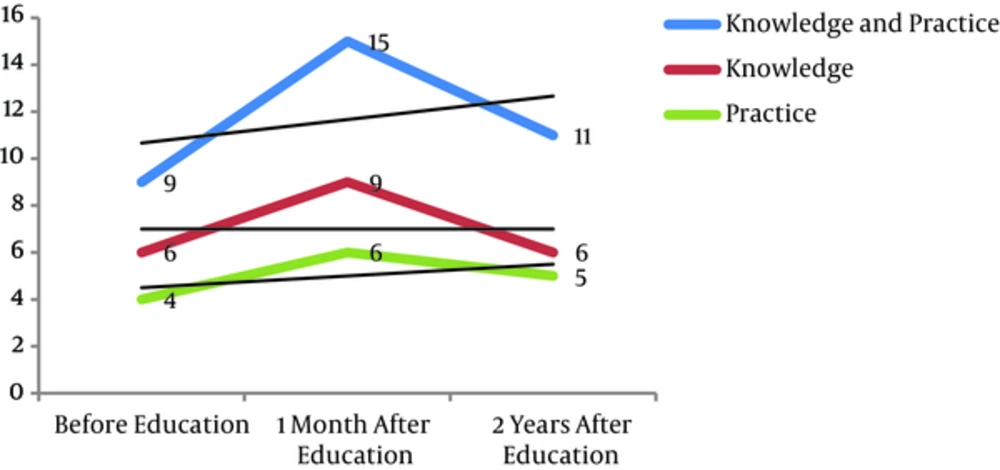
It was revealed that the knowledge of symptoms, diagnosis (except for the definition of MDR-TB), control, and prevention of TB (except for the importance of proper diagnosis and treatment of acid fast bacilli [AFB]-positive TB) was acceptable in the pre-education phase. However, knowledge of airborne transmission, contraindication to treatment with pyrazinamide (PZA) in TB patients, and simultaneous chronic liver disease was unacceptable. Within 1 month after education, knowledge of all related items was found to be acceptable. Also, the knowledge level was acceptable after 2 years, except for airborne transmission, MDR definition, and contraindications to PZA treatment (Table 1). In other words, the median of knowledge score was 6 (out of 10) before education, while it increased to 9 at 1 month after education and reduced to 6 after 2 years (Table 2 and Figure 1).
| Items | Before Education | After Education | |
|---|---|---|---|
| Pre-Education, n (%) | One Month After Education, n (%) | Two Years After Education, n (%) | |
| Chronic cough as the most common symptom of pulmonary TB in adults | 51 (85) | 48 (80) | 56 (93.3) |
| Inadequate weight gain as the most common sign of TB in pediatrics | 31 (51.7) | 48 (80) | 33 (55) |
| Airborne transmission as the most common transmission route of pulmonary TB | 16 (26.7) | 38 (63.3) | 19 (31.7) |
| CXR cannot be the only tool for initiating or ending pulmonary TB treatment. | 48 (80) | 44 (73.3) | 49 (81.7) |
| The results of PPD test should be interpreted with respect to the endemic status of the patient’s living area and his/her characteristics. | 34 (56.7) | 40 (66.7) | 39 (65) |
| MDR-TB is defined as positive AFB sputum smear pulmonary TB resistant to at least INH and rifampin. | 17 (28.3) | 39 (65) | 23 (38.3) |
| The most important cause of MDR-TB is irrational prescription of anti-TB drugs for patients. | 44 (73.3) | 47 (78.3) | 45 (75) |
| Pyrazinamide is contraindicated for the treatment of TB in patients with chronic liver disease. | 19 (31.7) | 43 (71.1) | 22 (36.7) |
| BCG vaccination does not cause lifelong immunity against TB. | 47 (78.3) | 45 (75) | 43 (71.7) |
| The most important strategy for the prevention of TB transmission in the community is timely and correct diagnosis and treatment of AFB-positive pulmonary TB. | 23 (38.3) | 37 (61.7) | 30 (50) |
Abbreviations: AFB, acid fast bacilli; BCG, Bacille Calmette-Guerin; CXR, chest X-ray; INH, isoniazid; MDR-TB, multidrug-resistant TB; PPD, purified protein derivative.
| Questions | Pre-Education, n (%) | Post-Education (1 Month), n (%) | Post-Education (2 Years), n (%) | |
|---|---|---|---|---|
| Knowledge | Mean ± SD (out of 10) | 5.5 ± 2.4 | 7.1 ± 3.7 | 5.9 ± 2.0 |
| Median | 6.0 | 9.0 | 6.0 | |
| 95% CI | 4.8 - 6.1 | 6.1 - 8.1 | 5.4 - 6.5 | |
| Min-Max | 0 - 10 | 0 - 10 | 1 - 10 | |
| Interquartile range | 3.0 | 3.7 | 2.0 | |
| Kolmogorov-Smirnov test of normality | 0.008 | < 0.001 | < 0.001 | |
| Distribution | Abnormal | Abnormal | Abnormal | |
| Proportion with at least 50% of total score | 71.7% | 80% | 76.7% | |
| Practice | Mean ± SD (out of 8) | 3.7 ± 1.9 | 5.3 ± 2.8 | 4.5 ± 1.6 |
| Median | 4.0 | 6.0 | 5.0 | |
| 95% CI | 3.2 - 4.2 | 4.5 - 6.0 | 4.1 - 4.9 | |
| Min-Max | 0 - 7.0 | 0 - 8.0 | 0 - 8.0 | |
| Interquartile range | 3.0 | 2.7 | 2.7 | |
| Kolmogorov-Smirnov test of normality | 0.07 | < 0.001 | < 0.001 | |
| Distribution | Normal | Abnormal | Abnormal | |
| Proportion with at least 50% of total score | 53.3% | 80% | 75% |
The findings also showed that before education, the students’ practice was unacceptable regarding the following tasks: wearing filter masks in contact with pulmonary TB patients, use of purified protein derivative (PPD) test, treatment of patients with negative AFB sputum smear, treatment of children with TB, and management of drug-induced hepatotoxicity. However, one month after primary education, practice was acceptable in all items. Also, after 2 years of education, only practice of PPD test and treatment of patients with negative AFB sputum smear test was unacceptable (Table 3). In other words, the median score of practice regarding TB was 4 (out of 8) before education, which increased to 6 at 1 month after education and decreased to 5 after 2 years of education (Table 3 and Figure 1).
| Items | Before Education | After Education | |
|---|---|---|---|
| Pre-Education, n (%) | One Month After Education, n (%) | Two Years After Education, n (%) | |
| Wearing a filter mask in contact with pulmonary TB patients | 27 (45) | 42 (70) | 30 (50) |
| Performing AFB sputum smear test for the diagnosis of pulmonary TB | 38 (63.3) | 44 (73.3) | 47 (78.3) |
| Conducting a PPD test with an intradermal injection (0.1 cc) and interpretation of results after 48 - 72 hours | 28 (46.7) | 40 (66.7) | 26 (43.3) |
| Referring a patient who is suspected of pulmonary TB to the nearest health center for AFB sputum smear test | 42 (70) | 46 (76.6) | 33 (55) |
| Starting anti-TB treatment for patients suspected of pulmonary TB and 2 positive AFB sputum smear tests | 36 (60) | 42 (70) | 47 (78.3) |
| Two weeks of treatment using broad-spectrum antibiotics as the initial step for patients who are suspected of pulmonary TB and have 3 negative AFB sputum smear tests | 12 (20) | 38 (63.3) | 27 (45) |
| Initiation of anti-TB treatment for children with inadequate weight gain, PPD test ≥ 5 mm, and close contact with patients with active pulmonary TB | 16 (26.7) | 35 (58.3) | 32 (53.3) |
| Cessation of anti-TB drugs and emergency admission of TB patients whose liver enzymes show a 3-fold increase and right upper quadrant tenderness | 24 (40) | 31 (51.7) | 30 (50) |
Abbreviations: AFB, Acid Fast Bacilli; PPD, Purified Protein Derivative.
The sum score of knowledge and practice was 9, 15, and 11 (out of 18) before education, 1 month after education, and 2 years after education, respectively (Figure 1). The trend analysis showed that the median of both knowledge and practice increased by about 50% after 1 month of education, compared to the pre-education period. However, no increase was reported in the level of knowledge, and only a 25% increase was found in the practice of students after 2 years of education, compared to the pre-education period. The median of the sum score of knowledge and practice showed an increase of 66% and 22% after 1 month and 2 years of education, respectively (Figure 1).
This study also revealed that the frequency of acceptable knowledge (χ2, 1.9; P = 0.1) and acceptable practice (χ2, 1.1; P = 0.2) was not significantly different between genders. However, the frequency of acceptable sum score of knowledge and practice was higher among males (23/27; 85.1%), compared to females (19/33; 57.5%; χ2, 5.39; P = 0.02). After 2 years of graduation, knowledge (χ2, 0.02; P = 0.8), practice (χ2, 0.2; P = 0.6), and sum score of knowledge and practice (χ2= 0.5; P = 0.4) were not significantly different between students who passed the continued medical education (CME) course after graduation and those who did not.
Our findings also showed that after 1 month and 2 years of graduation, knowledge, practice, and sum score of knowledge and practice were not significantly different between subjects who attended the infection ward during their internship and those who did not (P > 0.05). An acceptable level of knowledge was more frequent among students who visited patients suspected of TB (30/34; 88.2%), compared to those who did not have such an experience (16/26; 61.5%) after graduation (χ2, 5.8; P = 0.01). However, no significant difference was found between these 2 groups regarding the level of practice (χ2, 0.8; P = 0.3) and sum score of knowledge and practice (χ2, 3.3; P = 0.06).
5. Discussion
This study showed that the overall knowledge and practice of national TB guidelines was acceptable, but not optimal among medical students. We also found that the median score of both knowledge and practice of TB increased by nearly 50% after 1 month of education; nonetheless, only practice showed a 25% increase after 2 years of education. Based on the findings, knowledge and practice were not significantly different between males and females. Also, no significant difference was found among individuals who attended the infection ward and those who did not. Similarly, there was no significant difference among individuals who passed the CME course and those who did not; a similar finding was reported among individuals who visited patients with suspected TB and those who did not. However, adequate knowledge was more frequent in those who visited TB-suspected patients, and the sum score of knowledge and practice was higher among male students.
According to the TB global report by WHO in 2016, the incidence of TB in the world and Eastern mediterranean region was 142 and 116 per 100 000 people, respectively, and the case notification rates were 85% and 77% in 2015, respectively (1). In these regions, the prevalence of TB was 174 and 160 per 100 000 population in 2014, while the mortality rates were 24 and 13 per 100000 population in 2015, respectively (1). Generally, more than 95% of mortality due to TB occurs in low- and middle-income countries; six countries, including India, Indonesia, China, Nigeria, Pakistan, and South Africa, account for 60% of these mortalities, respectively (2). In Iran, the incidence, prevalence, and mortality due to TB were 13, 32, and 1.8 per 100 000 population, respectively, while about 28% of TB cases were not detected in 2015 (7).
According to the global targets of “End TB Strategy” by WHO, it is expected to reduce TB mortality by 90%, to decrease new cases by 80%, and to reduce families’ costs by 2030 (2). Evidence reveals that without proper treatment of active TB, mortality of these patients will reach 45% - 100% with respect to the HIV status (2). Therefore, rapid and accurate diagnosis of TB is important in preventing its transmission and mortality (5). In Iran, about two-thirds of TB cases are primarily diagnosed in the private sector by GPs (7). On the other hand, after implementation of the rural family physician (FP) program in 2005 and urban FP program in 2012 in Iran (8, 9), comprehensive national FP guidelines have been presented for the management of patients because of the importance of KAP improvement in the management of patients with chronic diseases (e.g., TB) (10).
A systematic review of knowledge about appropriate TB treatment among healthcare workers showed that they had adequate knowledge about anti-TB drug treatments, including duration of treatment and dose of drugs (3). Moreover, Olarewaju Sunday et al. conducted a survey of TB knowledge among 241 Nigerian final-year medical students and reported poor knowledge and management in 69% of students (11); evidently, this rate is higher than the present result (28.3%).
Laurenti et al. reported a positive association between internship in wards and greater knowledge of TB diagnosis (55.9% vs. 51.6%) and treatment (48.4% vs. 41.8%) (12); in contrast, our study showed that attendance in special wards does not increase the level of knowledge about TB. Laurenti et al. also found a moderate level of knowledge about TB (56.6%) and showed that students, who had visited at least 1 active pulmonary TB patient, had a slightly higher rate of correct answers about TB diagnosis, compared to those who had not visited such patients (55.5% vs. 51.4%) (12); these results are similar to our findings.
Moreover, Zhao et al. conducted a survey of TB knowledge among 1486 medical students in Southwest China and revealed that only 24.1% of students had knowledge about TB symptoms (13); nonetheless, this figure was higher in our study (80%). Zhao et al. also revealed that exposure to health education messages was significantly associated with greater knowledge of symptoms, disease transmission, curability, services provided by local TB dispensaries, and free TB treatment (13). In addition, a survey by Teixeira et al. in Brazil showed that about half of 1094 medical students from 5 medical schools were not informed about the main routes of TB infection, and more than two-thirds of these students did not use protective masks when examining an active TB case (14).
Another survey from India by Acharya et al. on TB knowledge and attitude showed that 98.5% of final-year medical and nursing students (n, 200) were informed about person-to-person transmission of TB. This rate is higher than that of the present study, which showed that two-thirds of medical students were familiar with airborne transmission as the most common route of TB (15). On the other hand, this study revealed that only 27% of medical students used surgical masks in contact with TB patients, while less than 45-70% of medical students in our study followed this practice (15).
The study by Acharya et al. showed that 72% of students did not think that healthcare workers are at a greater risk of TB, while 52% knew that non-directly observed treatment, short course (non-DOTS) strategies are associated with a higher risk of drug resistance and mortality (15). Acharya et al. also showed that 98.5% of medical students had a positive attitude towards TB prevention and treatment (15). Finally, they recommended knowledge improvement about TB transmission and its preventive aspects among healthcare students (15).
In addition, Montagna et al. conducted a multicenter survey to evaluate the knowledge and practice of TB among 2220 undergraduate healthcare students at 15 Italian universities. They showed a sufficient level of knowledge about TB (16). Up to 95% of students correctly answered the questions about TB etiology. Also, 60% of students gave correct answers to questions about Bacille Calmette-Guerin (BCG) vaccine, which is lower than the knowledge level of our students about this vaccine (78.3%). Medical students (85.4%) had better knowledge than nursing students (65.7%) (16).
As Kiefer et al. reported in their survey, physicians and nurses in Peru had a fair mean knowledge of TB (10 ± 1.9 out of 14), which is higher than the present study (5.5 ± 2.4 out of 10) (17). We similarly showed that the level of knowledge, practice, and total score of knowledge and practice were not significantly different among individuals who attended the infection ward during their internship and those who did not.
Furthermore, in a study from Golestan and Mazandaran provinces (North of Iran), the mean knowledge of TB and DOTS strategy among 80 final-year medical students was lower (18) than the present study (1.8 ± 1.6 out of 15 vs. 5.5 ± 2.4 out of 10). In addition, the survey revealed that knowledge of diagnosis, treatment, and monitoring of TB was poor, and similar to our study, no significant difference was found between the knowledge of students who had attended the infection ward and those who had not (18).
Additionally, another survey at Mashhad University, Northeast of Iran, assessed the knowledge of TB among 90 public health and medical students. Based on the findings, the knowledge level of medical students was low (8.6 ± 1.9 out of 20) (19). Furthermore, the mean score of knowledge of medical students about both diagnosis and treatment of TB was 16.4+3.7 out of 40, and no significant association was found between gender and knowledge (19). This finding is in contrast to our study, which showed that the acceptable level of knowledge was more frequent in males (23/27; 85.1%), compared to females (19/33; 57.5%; P = 0.02). Another study from Karaj, Iran showed that only 2% of private GPs (n, 340) had adequate knowledge about national TB programs. Also, 27.1% were familiar with the most important symptom of pulmonary TB, and about 43% had information about 4 main drugs for TB treatment (20).
Behnaz et al. also conducted a survey to assess KAP among final-year medical students in Yazd, Central Iran (21) and found that knowledge and practice of students were moderate to high in 99.3% and 88.1% of cases, respectively (21); this rate is higher than what we estimated in our study. However, in their study, 43% of students did not know that the sputum smear test is the most important method for the diagnosis of pulmonary TB (21). On the other hand, in our study, 78.3% of postgraduate medical students reported that patients who are suspicious of pulmonary TB should be referred to TB laboratories for AFB sputum smear test. Moreover, we found that 78.3% of medical students did not believe that BCG vaccine provides lifelong immunity, while more than 50% of students had this opinion in the study by Behnaz et al. (21).
The most important limitation of our study was related to the target group, which was hardly accessible due to the wide geographical job distribution. However, after several contacts via E-mail, SMS, and social networks, we could finally assess their knowledge and practice. We recommend a large-study at the national level, including both public and private sectors to present a more comprehensive image of the level of TB knowledge and practice among medical students, GPs, and nurses, as similarly suggested in another study (22). In addition, we suggest effective educational protocols in national TB guidelines. Also, study of the efficacy of CME courses for TB is recommended.
5.1. Conclusion
This study indicated the need for regular, continuous, and patient-centered training courses of TB before, during, and after graduation for all medical students.