1. Background
There has been a tremendously increasing trend in the elderly population, compared to other age groups throughout the world (1). According to the World Health Organization (WHO), the elderly population will exceed one billion by 2020, and developing countries will face the highest rate of growth in the elderly population (2). Similarly, an increase was reported in the elderly population of Iran in 2010 and 2016 by 8.2% and 10.1%, respectively (3).
Sleep is one of the physiological necessities associated with major human functions (4). Desirable sleep maintains physical health, reduces moodiness and anxiety, strengthens one’s ability to adapt, and increases concentration in daily life activities (5). The aging process leads to palpable physiological changes in sleep patterns, which need to be differentiated from sleep disorders. These changes include a reduction in the total sleep duration and efficiency, an increase in sleep fragmentation, and greater difficulty in falling asleep (6). Although some of these changes may be a function of normal aging, others may be attributed to the underlying medical conditions (7).
Researchers have reported that poor quality of sleep (QOS), following headache, and gastrointestinal disorders, is the third most common problem of the elderly population. Sleep disturbances are common symptoms in elderly people, which is referred to as primary care physicians and psychiatrists (8). The prevalence of at least one sleep complaint is over 50% in the elderly worldwide (9). In addition, 67% of the elderly population in Iran suffers from sleep disorders, and 61% have insomnia (10). 82.6% of retired elderly people who participated in a survey in Iran had poor sleep quality (11). Furthermore, a survey in Kashan demonstrated the low sleep quality in hospitalized elderly people, and it was associated with sex, marital status, and also previous hospitalization experience (12).
According to the literature review, no study has examined the prevalence of sleep disorders in the elderly population of Fars province, Iran. The relevance of sleep components and the associated sleep quality predictors were mentioned separately, which was not studied before in Iran. Also, there are factors observed for the first time in correlation with sleep quality, including being a provider of living cost, relativity with a spouse, being the main decision maker about family finance and sexual dysfunction. Therefore, the present study aimed to determine the prevalence and predictors of sleep disorders and the associated factors in this population.
2. Methods
This population-based and cross-sectional study was conducted in 2017 - 2018 (1.5 years). The sample size was calculated to be 408, based on the sample size calculation formula (n = z2pq/d2) by considering the prevalence of sleep disorder to be 67% at 95% confidence interval, 5% error, and 20% dropout (10). We selected adults above 60 years from the population of Shiraz (1.9 million people), which is the capital of the Fars province in the South of Iran.
For sampling, we first defined the proportion of the elderly population in three health networks (Valfajr, Enghelab, Shohadaye Gomnam), which is affiliated to Shiraz University of Medical Sciences (SUMS). Then, the proportion of the sample size in each network was determined. Each of these networks covers several urban health centers. In the next step, several clusters were selected randomly from the list of urban healthcare centers in each of the three-mentioned networks by considering each urban health center as a cluster. Then, we defined the sample size in each cluster, according to the number of registered elderly. The final samples were selected from the records in each cluster via systematic random sampling.
Data, including the phone numbers of the selected samples, was extracted from the healthcare center records. The samples were contacted via phone calls. After the trained researchers introduced themselves and explained the objectives of the study, they asked the elderly if they were willing to visit the clinics on weekends. The phone numbers of two researchers, involved in the study implementation, were also given to the participants so that they could ask their questions or requests related to the study.
At the clinic, detailed explanations were given to every participant, and a checklist, including information (age, gender, educational status, marital status, source of income, and birth place), health status (anthropometric indicators, physical activity, presence of chronic diseases, psychiatric problems, and medications), and nutritional status (a 72-hour recall), was completed for each interviewee.
Quality of life (QOL) was also determined by completing the elderly quality of life questionnaire (LIPAD). Also, QOS was assessed using the valid and reliable (89.5%) Persian version of the Pittsburgh Sleep Quality Index (PSQI) (13). PSQI assessed QOS during the last month before the study and consisted of questions on seven dimensions: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medications, and daytime dysfunction. The questions related to each dimension were scored from zero to three: zero, without sleep disturbance; one, moderate sleep disturbance; two, severe sleep disturbance; and three, very serious sleep disturbance. The total score was measured by summing the scores of seven dimensions (range, 0 - 21); total scores above five indicated poor sleep quality.
Data were entered in IBM SPSS version 25. We used the Univariate Analysis to determine the association of different factors with QOS. Then, we performed a binary logistic analysis (Forward Wald selection) for factors correlated with QOS at P ≤ 0.2. Moreover, a linear regression model was used to evaluate the correlation of each dimension with the total score of QOS. P values less than 0.05 were considered statistically significant. Also, for assessing the correlation of each QOS component with sleep disturbance, Kendall’s tau-b correlation coefficient was measured.
2.1. Inclusion and Exclusion Criteria
All selected individuals whose information forms were fully completed in this research were included; however, incomplete relevant forms were removed from the study and replaced by the alternative codes. Moreover, since the participation in this study was entirely optional; if a person expressed dissatisfaction with the participation he or she was removed from the study, and as mentioned, the alternative code was used instead. Also, the elderly with Alzheimer’s disease could not be assessed in terms of QOS.
3. Results
In this study, 22 out of 408 samples were excluded due to a history of Alzheimer’s disease. Finally, 386 participants were studied, consisting of 200 (51.8%) females. Among the samples, 272 (70.5%) were married, and 350 (90.7%) had 12 years of education. The mean age of the participants was 67 ± 6.1 years. Out of all interviewees, 213 (55.2%) had sleep disorders. The analysis of socioeconomic, demographic, and anthropometric characteristics of the participants, as well as their medical history, is presented in Table 1.
| Characteristic | No. (%) | Characteristic | No. (%) | Characteristic | No. (%) |
|---|---|---|---|---|---|
| Age (y) | Provider of living cost | Psychological disease | |||
| 60 - 69 | 248 (64.2) | His/herself | 222 (57.5) | Yes | 84 (21.8) |
| 70 - 79 | 114 (29.5) | Other | 159 (41.2) | No | 302 (78.2) |
| ≥ 80 | 24 (6.2) | Supplementary insurance | Chronic pain | ||
| Gender | Yes | 281 (72.8) | Yes | 259 (67.1) | |
| Male | 186 (48.2) | No | 105 (27.2) | No | 127 (32.9) |
| Female | 200 (51.8) | House ownership status | Kidney disease | ||
| Level of education (y) | Landlord | 346 (89.6) | Yes | 78 (20.2) | |
| ≤ 12 | 350 (90.7) | Tenant | 40 (10.4) | No | 308 (79.8) |
| > 12 | 36 (9.3) | Being the main decision maker about family finances | Osteoporosis | ||
| Marital status | Yes | 254 (65.8) | Yes | 175 (45.3) | |
| Married | 272(70.5) | No | 132 (34.2) | No | 211 (54.7) |
| Single | 114(29.5) | Occupation | Blood disease | ||
| Birth place | Having job | 43 (11.1) | Yes | 65 (16.8) | |
| Village | 33(8.5) | Jobless | 343 (88.9) | No | 321 (83.2) |
| City | 353(91.5) | People living under one roof | Auditory impairment | ||
| Relativity with spouse | Mean ± SD | 3 ± 1.59 | Yes | 378 (97.9) | |
| 1ST degree | 90(23.3) | Median (min - max) | 3 (11) | No | 8 (2.1) |
| Non 1st degree | 294(76.2) | Quality of life | Diabetes mellitus | ||
| BMI (Bassy) Kg/m2 | < 70 (of 93) | 97 (25.1) | Yes | 119 (30.8) | |
| 6.07 - 15.26 | 9(2.3) | ≥ 70 | 282 (73.1) | No | 267 (69.2) |
| 15.27 - 24.46 | 114(37.3) | Daily calories intake | Hyperlipideamia | ||
| 24.47 - 33.66 | 211(54.7) | < 1600 | 266 (68.9) | Yes | 184 (47.7) |
| 33.67 - 52.06 | 19(4.9) | ≥ 1600 | 117 (30.3) | No | 202 (52.3) |
| Use of water pipe | Heart disease | Sexual dysfunction | |||
| Yes | 44(11.4) | Yes | 66 (17.1) | Yes | 58 (15) |
| No | 342(88.6) | No | 320 (82.9) | No | 328 (85) |
| Income to cost ratio | Hypertension | Taking medical supplement | |||
| ≤ 1 | 206(53.3) | Yes | 216 (56) | Yes | 346 (89.6) |
| > 1 | 84(21.8) | No | 170 (44) | No | 40 (10.4) |
The univariate analysis showed that gender, marital status, source of income, QOL, daily calorie intake, heart disease, chronic pain, diabetes mellitus, psychological diseases, osteoporosis, blood diseases, and use of medications and vitamin supplements were correlated with sleep problems (P ≤ 0.05) (Table 2). In addition, body mass index (BMI), measured by Bassey’s equation (14), water consumption, hyperlipidemia, kidney diseases, and hypothyroidism showed associations with sleep disorder (0.05 < P ≤ 0.2). However, other factors did not show any significant associations (P > 0.2). Out of 213 interviewees with sleep disturbances, 135 (35%) were female, and 78 (28.2%) were male (OR, 0.4; P < 0.001).
| Characteristic | Yes, N (%) | No, N (%) | Chi-Square | P Value | OR (CI 95%) |
|---|---|---|---|---|---|
| Gender | |||||
| Male | 83 (21.5) | 103 (26.7) | |||
| Female | 130 (33.7) | 70 (18.1) | 16.2 | < 0.001 | 0.4 (0.3 - 0.6) |
| Marital status | |||||
| Married | 135 (35.0) | 137 (35.5) | |||
| Single | 78 (20.2) | 36 (9.3) | 11.5 | 0.001 | 2.2 (1.4 - 3.5) |
| Provider of living cost | |||||
| His/herself | 105 (27.2) | 117 (30.3) | |||
| Other | 105 (27.2) | 54 (14.0) | 13.1 | < 0.001 | 2.2 (1.4 - 3.3) |
| Quality of life | |||||
| < 70(of 93) | 73 (18.9) | 24 (6.2) | |||
| ≥ 70 | 137 (35.5) | 145 (37.6) | 20.8 | < 0.001 | 0.3 (0.2 - 0.5) |
| Daily calories intake | |||||
| < 1600 | 159 (41.2) | 107 (27.7) | |||
| ≥ 1600 | 53 (13.7) | 64 (16.6) | 6.9 | 0.010 | 0.6 (0.4 - 0.9) |
| Heart disease | |||||
| Yes | 44 (11.4) | 22 (5.7) | |||
| No | 169 (43.8) | 151 (39.1) | 4.2 | 0.042 | 1.8 (1.0 - 3.1) |
| Chronic pain | |||||
| Yes | 165 (42.7) | 94 (24.3) | |||
| No | 48 (12.4) | 79 (20.5) | 23.1 | < 0.001 | 2.9 (1.9 - 4.5) |
| Diabetes mellitus | |||||
| Yes | 76 (19.7) | 43 (11.1) | |||
| No | 137 (35.5) | 130 (33.7) | 5.2 | 0.027 | 1.7 (1.1 - 2.6) |
| Psychological disease | |||||
| Yes | 57 (14.7) | 27 (7.0) | |||
| No | 156 (40.4) | 146 (37.8) | 6.9 | 0.009 | 2.0 (1.2 - 3.3) |
| Osteoporosis | |||||
| Yes | 117 (30.3) | 58 (15.0) | |||
| No | 96 (24.9) | 115 (29.8) | 17.6 | < 0.001 | 2.4 (1.6 - 3.6) |
| Blood disease | |||||
| Yes | 53 (13.7) | 24 (6.2) | |||
| No | 160 (41.4) | 149 (38.6) | 7.2 | 0.007 | 2.1 (1.2 - 3.5) |
| Taking medication and /or vitamin | |||||
| Yes | 199 (51.5) | 147 (43.8) | |||
| No | 141 (38.3) | 26 (6.7) | 7.3 | 0.007 | 2.5 (1.3 - 4.9) |
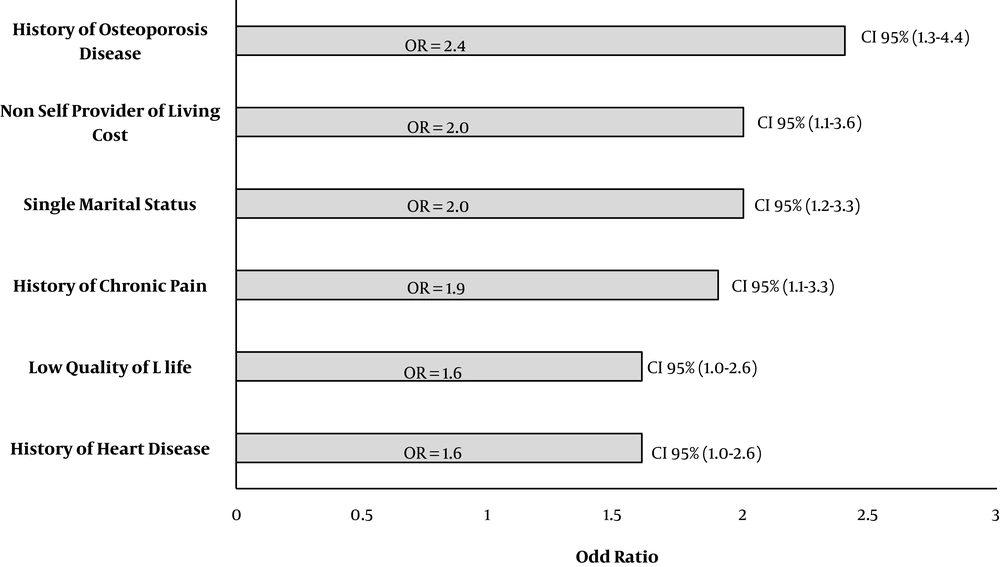
The multivariable analysis showed that heart disease (OR, 2.4; P = 0.008), QOL (OR, 2.0; P = 0.015), chronic pain (OR, 2.0; P = 0.005), marital status (OR, 1.9; P = 0.019), osteoporosis (OR, 1.6; P = 0.047), and being the main income provider (OR, 1.6; P = 0.045) were correlated with sleep disorders in the elderly, respectively (Figure 1). In addition, evaluation of correlations showed that sleep latency (r, 0.479; P < 0.001), habitual sleep efficiency (r, 0.469; P < 0.001), subjective sleep quality (r, 0.399; P < 0.001), sleep disturbance (r, 0.340; P < 0.001), sleep duration (r, 0.333; P < 0.001), daytime dysfunction (r, 0.278; P < 0.001), and use of sleep medications (r, 0.228; P < 0.001) were correlated with sleep disturbances, respectively.
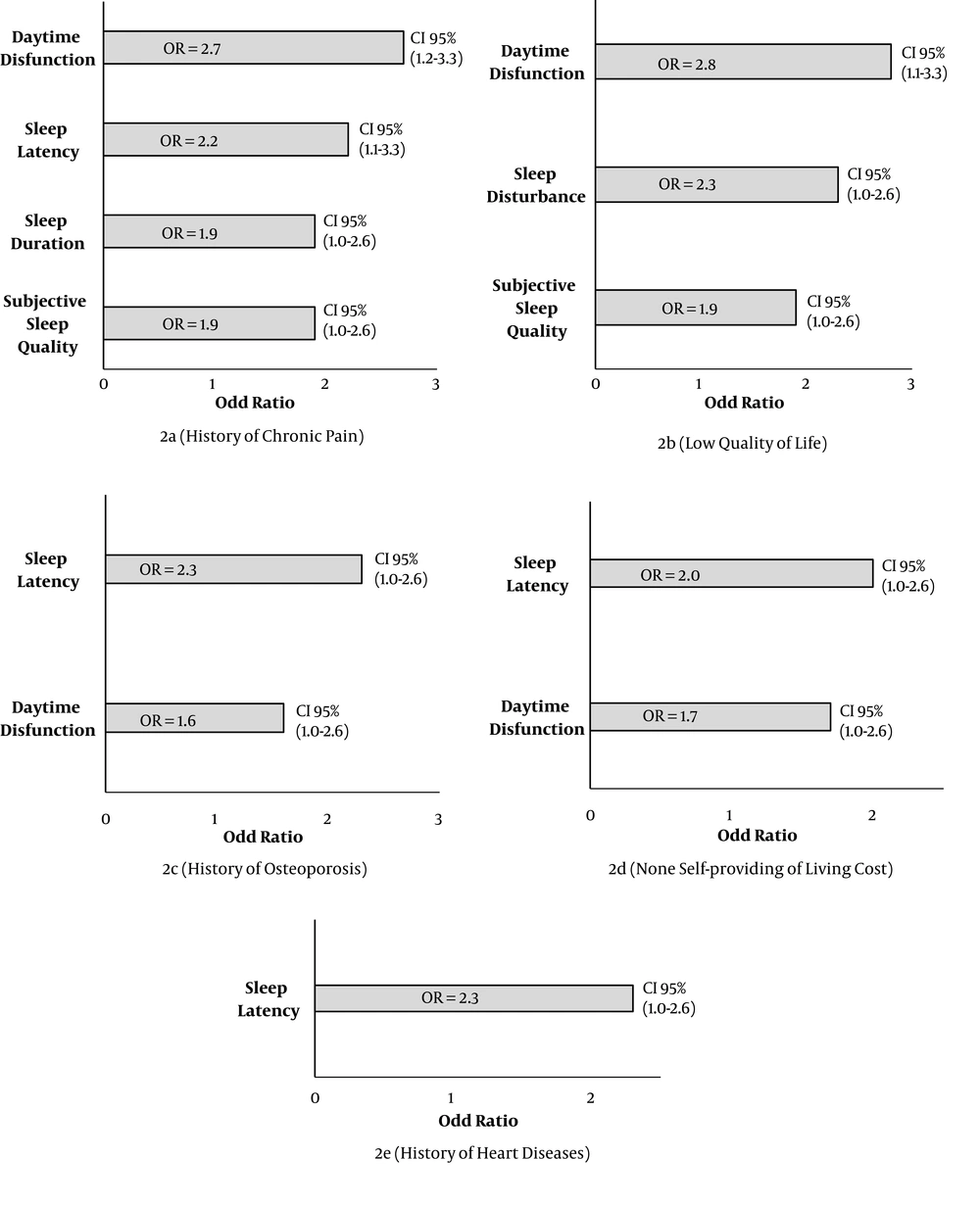
Based on the findings, sleep latency (OR, 2.0; P = 0.002) and daytime dysfunction (OR, 1.7; P = 0.025) were more frequent in non-providers, while the elderly with low QOL mostly complained about daytime dysfunction (OR, 2.8; P < 0.001), sleep disturbances (OR, 2.3; P < 0.001), and subjective sleep quality (OR, 1.9; P = 0.008). As the results indicated, singles were more influenced by sleep latency (OR, 2.3; P < 0.001). Also, the elderly with a history of osteoporosis suffered from not only sleep latency (OR, 2.3; P < 0.001), but also daytime dysfunction (OR, 2.7; P = 0.001).
Based on the results, the elderly with chronic pain complained of problems related to sleep latency (OR, 2.2; P = 0.002), sleep duration (OR, 1.9; P = 0.040), and subjective sleep quality (OR, 1.9; P = 0.008) (Figure 2). Finally, the assessment did not show any significant association between sleep duration and daily intake of carbohydrates, fats, proteins, and calories (P > 0.05).
5. Discussion
The present study showed that almost half of the elderly in our region have sleep disturbances. It was also found that sleep latency is highly correlated with sleep problems, whereas daytime dysfunction and the use of sleep medications have the least significant correlation. Moreover, this study revealed that heart disease, QOL, chronic pain, marital status, being an income provider, and history of osteoporosis were strongly associated with QOS. Also, chronic pain and lower QOL were the main determinants of daytime dysfunction, while single marital status, history of osteoporosis, and being a provider were the main correlates of sleep latency. However, sleep duration was not correlated with the nutritional status of the elderly.
According to statistics, the elderly population in Iran is expected to reach more than 25 million by 2050. The elderly people also comprise 10.2% of the Fars province population (3).
According to previous studies, sleep problems are prevalent in 80% of the world’s elderly population. Also, 40% - 50% of the elderly population is not satisfied with sleep quality and suffers from chronic sleep problems (2, 4). In addition, based on a previous study conducted in Iran, 67% of elderly people have sleep disorders (10). The present findings are in line with a previous study, which showed that QOS was associated with QOL in the elderly; however, there are contradictions regarding the association between QOS and nutrition (15).
In this regard, a meta-analysis revealed that female gender, pain, low health status, low level of education, low QOL, major depression, mild cognitive impairment, and poor physical activity were correlated with sleep complaints (16). Other reports show that QOS is significantly correlated with socioeconomic status, and unemployed people were found to have poor QOS; however, there was no obvious association between age and sleep problems (17).
Other studies have supported a significant direct correlation between desirable QOS and male gender, high level of education, and lack of disease (18, 19). The results of the present study did not show any significant associations between sleep disorders and gender, level of education, physical activity, diabetes mellitus, hypertension, depression, or violence. These findings are somehow consistent with a previous study, which reported no significant correlations between sleep disorders and gender, educational level, or hypertension (15).
In the present study, a history of heart disease was shown to influence QOS in the elderly. A survey showed a 50% higher risk of heart failure in men with impaired awakening and found that women with sleep disturbances and frequently irritated/tired eyes were at risk of stroke, long-term cardiovascular events, and heart failure (20). Another study reported a higher prevalence of cardiovascular diseases in the elderly with poor QOS (21). Conversely, men and women with confirmed angina were found to have more trouble falling asleep than others (1.6 times) (22). Other studies have also examined the effects of impaired sleep on cardiovascular prognosis (23-25).
We also noted that the elderly with lower QOL had lower QOS. According to some studies, QOS plays a pivotal role in QOL; in other words, individuals with poor QOS have a lower level of QOL (20, 26-28). Chronic pain is a common symptom in the elderly population (29) and is often associated with sleep disturbances (30). In fact, sleep disturbances, such as sleep latency, decreased sleep duration, and increased frequency of awakening, are more prevalent in the elderly with consistent chronic pain, compared to those with lower pain intensities (31, 32); our study also reported somewhat consistent results.
A review study concluded that pain produced both short- and long-term negative effects on sleep. In fact, a reciprocal association was found between sleep and pain (33). In this regard, a previous study revealed that pain contributes to insomnia, and insomnia exacerbates pain (34); therefore, pain relief medications may improve QOS in the elderly (35).
Additionally, we concluded that marital status had a significant correlation with QOS. Based on the findings, single people had poorer QOS, compared to their married counterparts. This finding may be explained by the greater family and social support of married individuals (36-38). Other studies have also reported that lack of social support could reduce health and result in poor sleep quality (39).
Our study indicated an association between osteoporosis and QOS, which is in agreement with a previous study, indicating a strong association between osteoporosis and sleep disturbances (40). On the other hand, a survey showed an inverse association between sleep disturbances and physical activity in older women (41); this finding is in contrast to our study, which did not detect any correlations between these variables. According to another study, the elderly, who had a history of frequent hospitalizations and physician visits, had higher scores in the components of habitual sleep efficiency and sleep disturbances (42); nevertheless, we did not assess these variables in our study.
The present study had some limitations. We only studied the elderly population covered by public health centers and discarded those who were referred to private health centers. It should be noted that family physician programs and integrated elderly care programs have covered more than 95% of all families, including older adults in our region (43). On the other hand, to the best of our knowledge, the present study is among few studies evaluating QOS in the elderly and determining its association with different health indicators in this province. Moreover, the association between QOS and source of income was studied for the first time in this survey.
In conclusion, sleep disorder is common among the elderly, especially in those with a history of heart disease, low QOL, chronic pain, and osteoporosis, as well as non-providers of family’s costs. Therefore, these factors, as somewhat modifiable factors, should be integrated in the interventions for QOS improvement in the elderly.