1. Background
Improved performance is one of the central goals of any organization, which relies on the realization of two crucial economic principles: increased efficiency and quality. Research evidence suggests that the public sector has often failed to satisfy these two attributions (1, 2). Accordingly, policymakers and managers have constantly sought initiatives to overcome these defects (3, 4) appropriately. In response to these weaknesses, new public management (NPM) as a constructive alternative was coined (5). Exposure of the public sector with a quasi-market state was the key feature of this new approach. Given this, the public sector could improve the efficiency and quality of delivered services due to exposure to a competitive condition. The more competitive a market is, the higher the efficiency and quality of services will be (6-11).
Outsourcing or contracting out as a public-private partnership (PPP) arrangement has been one of the central strategies of NPM, which could benefit public organizations from the competitive market advantages. Providing all or part of the internal activities of a public organization is transferred to a third party or contractor through building on this paradigm (12). Due to its functional nature, the health sector is costly, and using efficiency-oriented strategies in this sector is of high priority (13, 14).
In Iran, outsourcing as decentralization and market-type policy (8, 13, 15) gained much attention roughly 15 years ago, coincident with the third four-year national development plan bill (16, 17). In line with this policy, Iran's Health Ministry asked its affiliated universities to implement this strategy (18). Although this policy has undergone some changes with altering the governments, concerning the consensus on its advantages and despite some pessimism derived from unsuccessful experiences (19), it has always been an alternative strategy for materializing the values of the private sector in public bodies (2, 20).
2. Objectives
In the current study, we aimed to investigate the number of outsourced services concerning the standard outsourcing models at Bushehr University of Medical Sciences after 15 years of ups and downs in implementing this policy.
3. Methods
This cross-sectional study was conducted at Bushehr University of Medical Sciences in 2020. The research population included deputies, hospitals, and healthcare networks affiliated with Bushehr University of Medical Sciences. This research was conducted in three stages. In the first stage, in order to extract PPP models, the literature review was done in several databases such as PubMed, Science Direct, Scopus, Magiran (in Persian), and Google Scholar using applied keywords including outsourcing, contracting out, PPP, and their Persian equivalents between 1990 - 2019 upon which 56 articles and two research reports were found. They were refined step by step, and finally, concerning the aim of the study and after reading titles, abstracts, and full texts, 25 articles and two research reports were selected. They were carefully reviewed, and seven outsourcing service models were obtained, as shown in Table 1 (20, 21). In the second stage, to correspond the outsourced services with their pertained PPP models, a three-part checklist was constructed, including the name of the outsourced contract, the kind of the outsourced model, and the kind of the outsourced service (clinical, non-clinical) sent to the relevant units to complete it. During the third stage, after receiving the completed checklists, to ratify and ensure the quality of the data recorded in the checklists, two experienced members of the research team randomly contrasted the recorded information in checklists with concluded contracts as a reference. Excel software version 2016 was used to calculate descriptive indices..
| Outsourcing Models | Definitions | Number of Outsourced Services | Total Suitable Services for Outsourcing | Percentage of Outsourced Services | ||
|---|---|---|---|---|---|---|
| Clinical | Non-clinical | Total | ||||
| 1. Service purchasing | Based on this model, in return for receiving certain services, the public sector will pay a private contractor. | 77 | 81 | 158 | 310 | 50.97 |
| 2. Management outsourcing | Regarding this outsourcing model, the management of a public body or department to increase efficiency and quality is delegated to a qualified person or team, whether or not inside or outside the public facility. | 1 | 0 | 1 | 5 | 20 |
| 3. Cooperative outsourcing | Upon this model, both sides of the contract are committed to providing the resources needed for delivering services. Share of each side from expected profits and other details is explicitly embedded in the contract. | 14 | 0 | 14 | 25 | 56 |
| 4. Leases contract | Upon this model, the private sector rents a public facility or a department. In return for this contract, the private firm acquires the right to collect revenues and employ human forces. The public sector may be responsible for providing capital equipment. | 0 | 0 | 0 | 0 | NA |
| 5. Complete outsourcing | According to this model, the government pays the private firm to manage and provide the required services in a public health facility. The private sector (firm) is committed to employing staff and providing logistic services and all the required equipment. | 14 | 0 | 14 | 80 | 17.50 |
| 6. Concession contract | Within the framework of this model, the public sector grants a concession to a private company to finance, build, operate and transfer or not a health facility to the public sector. BOT and BOO are two of the most prominent models of this kind. | 2 | 0 | 2 | 6 | 33.33 |
| 7. Divestiture contract (privatization) | Based on this model, ownership of a public entity like a hospital is transformed into a private sector. The private sector is responsible for delivering services, but the government's supervisory role is still maintained. | 0 | 0 | 0 | 0 | NA |
| 8. Total | 108 | 81 | 189 | 426 | 44.37 | |
Classification of Common Outsourcing Models and the Number and Percentage of Use of Each of Them at Bushehr University of Medical Sciences
4. Results
The study results showed that there were seven standard different outsourcing models on which public organizations can materialize PPP arrangements and pave the way for increasing productivity. The name and functions of each model are elaborated in Table 1.
The study’s findings also indicated that the private sector was providing a total of 189 cases of service delivered by the public sector. Of the189 outsourced cases, 108 were clinical, and the rest were non-clinical.
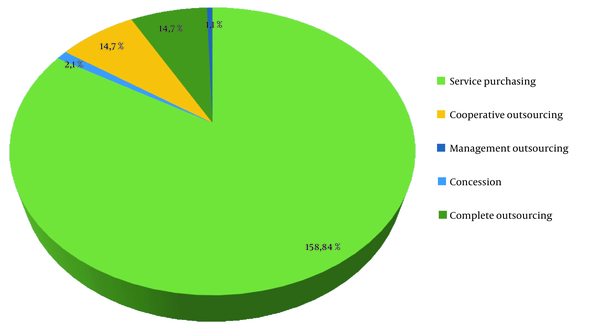
Based on the outsourcing models, the results highlighted that the service purchasing model with 158 cases accounted for the maximum share of outsourced services; meanwhile, the managerial outsourcing model with merely one case had the lowest share compared with other used models. Furthermore, the findings underlined that the complete outsourcing and cooperative models with 14 cases had the same proportion of contracted-out services (Figure 1 and Table 1).
Examining the usage rate of different outsourcing models in non-clinical services indicated that the only used model was service purchasing. However, various models have been used to outsource clinical services. It is noteworthy that two models, leases and divesture contracts, have not been used.
The investigation of the penetration rate of outsourcing models in all hospitals affiliated with Bushehr University of Medical Sciences implies that nearly 44% of services included in the checklist compatible with outsourcing are now being delivered through PPP, and the rest are still provided by the public sector itself.
5. Discussion
The public-private partnership, followed by the adoption of outsourcing models, is a strategy that can fulfill sustainability and increase the quality of services in the public sector. According to our information based on the latest literature review, this is the first study dealing with outsourced services and their associated models in the Bushehr healthcare sector.
The findings revealed that the scope of outsourcing health services included both clinical and non-clinical services. However, this is still a huge gap between the number of contracted-out services and the ones that potentially could be outsourced. This finding is of tremendous importance and shows that if managers are familiar with the objectives and functions of outsourcing, it can be more smoothly spread at the organizational level. This notion that clinical services are challenging to be outsourced is declined. In this regard, Sadeghi et al., in their study entitled review of models of PPP in the provision of hospital services, concluded that the scope of partnership depended on the studied country encompassed both clinical and non-clinical services. Several models have been used to achieve this goal, and this strategy has led to positive outcomes for patients and hospitals (20).
Barati et al., in their study (22), examined outsourced clinical units and concluded that three PPP models, including lease, cooperative and managerial, had been used, and outcomes were primarily satisfactory.
In another study, researchers revealed that several clinical services through a managerial model had been delegated, resulting in improved access and satisfaction (6).
The results of Ferdosi et al. (19) showed that outsourcing had been utilized for purchasing nursing services, and staff's perceptions had been negative toward it. Another research conducted by Ferdosi et al. showed that outsourcing had been used to provide nursing services in ENT and neurosurgery departments using the service purchasing model (23).
Studies by Khooban et al. and Tourani et al. showed that outsourcing had been successfully undertaken to provide pharmaceutical services, and service purchasing had been the used model (6, 24). Outsourcing of clinical and non-clinical services, as well as its positive and negative consequences, has been studied in several more studies (25-28). Furthermore, in some cases, the outsourcing model has been mentioned (29-31).
The present study's findings also showed that the dominant model had been service purchasing, as 84% of total outsourced services have been finalized using this model. This part of the findings is consistent with the results of some studies (32, 33). One of the reasons attributed to the high usage of this model is that this model has been used for a long time, and as a result, managers are familiar with the terms and conditions of this type model. Additionally, simplicity in implementation of this model has paved the way for its institutionalization.
From another perspective, the obtained results underscore that the two models, including leases and divesture contracts (privatization), have not yet been operationalized, which comes to a large extent back to the insufficient knowledge of managers and their conservativeness toward outsourcing. However, legal problems are worth noting (13, 34).
Generally, the conducted studies show that although various models exist to outsource services, this capacity has not been fully utilized. In most cases, policymakers and managers have considered one or two models. Low motivation and tendency of managers, lack of complete understanding of outsourcing philosophy, the unfamiliarity of managers with standard outsourcing models, unsuccessful outsourcing experiences, lack of eligible private providers, and weakness in law and regulation have hindered outsourcing expansion (7-9).
5.1. Study Limitation
Lack of access to the outsourced services annually was a limitation that did not allow us to track this policy's implementation rate by years at Bushehr University of Medical Sciences.
5.2. Conclusions
The results revealed that nearly 44% of clinical and non-clinical services embedded in the checklist compatible with outsourcing were being provided by the private sector at Bushehr University of Medical Sciences. The practical importance of this study is that by using the full capacity of outsourcing policy and maximizing the use of common models, it is possible to contract out the preparation of a large fraction of services to the private sector. Hence, it is strongly recommended to educate managers about the philosophy and methods of outsourcing as a priority in their training courses.
Examination and comparison of outsourcing models in terms of efficiency and quality would be an excellent subject for subsequent research.