1. Background
Infertility means not being pregnant after one year of regular sexual contact without using contraceptives (1). Studies have shown that about 10 - 15% of couples have infertility problems, with male infertility being the cause of 50% of cases (2). Currently, many infertility treatment centers use semen tests to differentiate between fertile and infertile people (3). The first step in assessing fertility and the health of the male reproductive system is to evaluate sperm parameters by a semen analysis. Sperm analysis involves calculating the concentration and percentage of motility and examining the morphology of the sperm.
Semen analysis is one of the most important and primary ways to diagnose fertility in men (4). According to the WHO definition, in semen analysis, parameters such as semen volume, total sperm count, sperm concentration, sperm motility, morphology, and pH of semen are examined (5). Examination of semen creates a beneficial prognosis for the health of the reproductive system. This is a non-invasive method, followed by other methods to find the cause of infertility (6). In semen examination, factors such as concentration, motility, volume, number, and morphology of sperm are measured to assess sperm quality (7). Studies have shown a relationship between mobility and fluid concentration and male fertility potential (8).
Follicle-stimulating hormone (FSH) and corpus luteum hormone (LH) regulate spermatogenesis. By secreting the hormone gonadotropin and its effect on the anterior pituitary lobe, it releases the hormones FSH and LH from the pituitary gland. These two hormones affect the testes and cause the production of sperm (9). Increasing concentrations of LH and FSH and decreasing concentrations of gonadal steroids cause gonadal insufficiency, which is a reason for infertility. The researchers reported an association between increased levels of FSH and the absence of sperm and infertility (10). Increased serum FSH indicates severe testicular damage, such as Sertoli cell syndrome or early cessation of spermatogenesis (11). Sperm DNA damage is an essential factor in male infertility (12). Studies have shown a link between the increasing age of men and decreasing sperm chromatin quality (13). Also, the risk of sperm DNA damage increases with age and may even lead to congenital disabilities (14). In assisted reproductive techniques, spermatozoa with damaged DNA have lower fertility, lower pregnancy rates, poor quality fetal growth, and increased risk of miscarriage, congenital disabilities, and neonatal diseases such as cancer (15). Hence, semen analysis is crucial in predicting male fertility potential (16).
2. Objectives
This study aimed to compare sperm parameters (volume, concentration, motility, count, morphology, pH, LH, FSH, and percentage of sperm DNA damage) between fertile and infertile males.
3. Methods
This study was performed by laboratory method to evaluate sperm parameters in 96 men referred to Narges Genetics Laboratory in Ahvaz. First, semen samples were collected after 2 to 7 days of abstinence. Samples were collected artificially. First, the samples were examined for color and odor. Then, the ejaculated samples were kept in an incubator at 37°C for 10 - 15 minutes. Semen samples were evaluated regarding sperm parameters, including volume, number, motility, morphology, and pH.
The normal range of seminal fluid volume from 1.5 mm to more than 2 mm and the percentage of normal sperm morphology between 40 and 50% were considered for fertile people, and less than this value were considered infertile. Also, infertile people participating in the study must have been married for one year and not have any contraception.
The number of sperm using the Makler Counting Chamber and sperm motility by computer aided sperm (CASA) software were evaluated according to the standards of the World Health Organization in 2010. After this step, the samples were transferred to the shaker for homogeneity. Semen samples were examined for sperm parameters, including concentration, motility, and morphology, according to the WHO criteria (17). To analyze the FSH and LH hormones, a blood sample was taken from veins, left at room temperature for 30 minutes, and then transferred to a centrifuge at 3,000 rpm for 15 minutes. Next, the tubes containing the hormones were kept at a temperature of 36°C. The ELISA technique (enzyme-linked immunosorbent assay; BioTek ELx808) and its specific kit wer eused to evaluate FSH and LH (PishtazTeb Co., Iran).
Also, sperm DNA health is essential for fertilization and fetal development. The WHO criteria of TUNEL (labeling deoxynucleotidyl transferase-mediated dUTP nick end) method was used to assess DNA health. This method was used to investigate double-stranded DNA damage. In this method, a DNA fragment at the 3 'OH site was labeled by the enzyme deoxynucleotide transferase in the presence of a nucleotide with a fluorescent substance. After staining using a fluorescent microscope, the reddened sperm showed sperm with healthy DNA, and the green sperm showed sperm DNA damage (16). To assess DNA damage by the TUNEL method, first, we washed the semen twice with phosphate-buffered saline (PBS). After preparing a smear on the slide and fixing it with 4% paraformaldehyde, it was dried in the air. The slides were painted according to the instructions of the TUNEL kit of Promga Company (Germany). In each sample, about 500 sperms were examined using a fluorescence microscope (BX51, Olympus, Japan) with a magnification of × 100. The obtained data were analyzed using SPSS software with chi-square and independent t-test. P < 0.05 was considered statistically significant.
4. Results
In this applied study, 96 men participated. After performing basic tests (volume, concentration, and motility of sperm) and additional tests (DNA damage and sex hormones), it was found that these people could be divided into two groups: Fertile and infertile. Next, these groups were divided according to age.
The study population was 96 people. The number of fertile people was 45, and the number of infertile people was 51. The mean age of fertile individuals was 32 ± 1.2 (20 - 53), and the mean age of infertile individuals was 36 ± 1.1 (23 - 53) (Table 1).
| Status | Average Age (y) | Number |
|---|---|---|
| Fertile persons | 32, (20 - 53) | 45 |
| Infertile persons | 36, (23 - 53) | 51 |
| Total | 35, (20 - 53) | 96 |
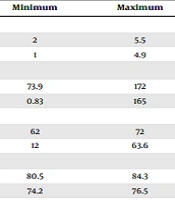
The mean volume of semen was 3.8 ± 0.1 mL (2.5 - 5 mL) in fertile individuals and 2.1 ± 0.1 mL (1 - 1.9 mL) in infertile individuals. The mean concentration was 124 ± 3.4 mL (73.9172 mL) in fertile individuals and 20 ± 5.6 mL (0.83 - 0.165) in infertile individuals. The mean mobility was 65 ± 0.3 (62 - 72) in fertile individuals and 59.8 ± 1.9 (12 - 63.6) in infertile individuals. The sperm count per milliliter was 82 ± 9.1 (80.5 - 84.3) in fertile men and 73.1 ± 2.3 (74.2 - 76.5) in infertile men. The FSH hormone levelwas4 ± 1.8 (2.4 - 4) mIU/mL in fertile men and 11.5 ± 1.5 (10 - 13.1) mIU/mL in infertile men. The LH hormone level was 3.4 ± 1.2 (1.3 - 3.8) mIU/mL in fertile men and 6.3 ± 0.3 (3.4 - 7.2) mIU/mL in infertile men. The mean pH was 7.2 ± 1 (7.1 - 7.2) in fertile men and 7.4 ± 1 (7.2 - 7.5) in infertile individuals. The percentage of sperm with abnormal morphology was 91 ± 1.8 (91.1 - 91.3) in fertile men and 95 ± 1.35 (94.2 - 96.9) in infertile individuals. The percentage of sperm DNA damage was 8 ± 1.2 (7.9 - 8.1) in fertile men and 16.05 ± 0.4 (14 - 18.1) in infertile individuals (Table 2).
| Parameters and Group | Minimum | Maximum | Mean ± SE | P-Value |
|---|---|---|---|---|
| Volume (mL) | < 0.005 | |||
| Fertile | 2 | 5.5 | 3.8 ± 0.1 | |
| Infertile | 1 | 4.9 | 2 ± 0.1 | |
| Density (106/mL) | < 0.005 | |||
| Fertile | 73.9 | 172 | 124 ± 3.4 | |
| Infertile | 0.83 | 165 | 20 ± 5.6 | |
| Mobility (%) | < 0.005 | |||
| Fertile | 62 | 72 | 65 ± 0.3 | |
| Infertile | 12 | 63.6 | 59.8 ± 1.9 | |
| Sperm count (mL) | > 0.001 | |||
| Fertile | 80.5 | 84.3 | 82 ± 9.1 | |
| Infertile | 74.2 | 76.5 | 73.1 ± 2.3 | |
| FSH (mIU/mL) | > 0.005 | |||
| Fertile | 2.4 | 4 | 4 ± 1.8 | |
| Infertile | 10 | 13.1 | 11.5 ± 1.5 | |
| LH (mIU/mL) | > 0.005 | |||
| Fertile | 1.3 | 3.8 | 3.4 ± 1.2 | |
| Infertile | 3.4 | 7.2 | 6.3 ± 0.3 | |
| pH | > 0.005 | |||
| Fertile | 7.1 | 7.2 | 0.9 ± 1 | |
| Infertile | 7.2 | 7.5 | 0.9 ± 2 | |
| Percentage of sperm with abnormal morphology | > 0.005 | |||
| Fertile | 91.1 | 91.3 | 91 ± 1.8 | |
| Infertile | 94.2 | 96.9 | 95 ± 1.35 | |
| Percentage of sperm DNA damage | < 0.005 | |||
| Fertile | 7.9 | 8.1 | 8 ± 1.2 | |
| Infertile | 14 | 18.1 ± 0.4 | 16.05 |
Abbreviations: SE, standard error; FSH, follicle-stimulating hormone; LH, luteum hormone.
Sperm volume, density, and mobility, the percentage of sperm DNA damage, and their relationships with age are shown in Table 2. Table 3 shows that sperm volume, density, and mobility and the percentage of sperm DNA damage decreased with increasing age. Sperm concentration was significantly reduced with increasing age. Also, the percentage of sperm DNA damage was significantly reduced in people over 40.
| Semen Parameters (y) | Mean ± SE | P-Value |
|---|---|---|
| Volume (mL) | ||
| < 30 | 2.75 ± 1.1 | 0.42 |
| 30 - 40 | 1.9 ± 0.1 | 0.35 |
| Over 40 | 1.2 ± 0.3 | 0.33 |
| Density (106/mL) | ||
| < 30 | 46.1 ± 10.1 | 0.04 |
| 30 - 40 | 19.9 ± 9 | 0.05 |
| Over 40 | 19.4 ± 5 | 0.06 |
| Mobility (%) | ||
| < 30 | 20 ± 4.5 | 0.15 |
| 30 - 40 | 20 ± 3.5 | 0.21 |
| Over 40 | 20 ± 1.2 | 0.12 |
| Percentage of sperm DNA damage | ||
| < 30 | 14 | 0.71 |
| 30 - 40 | 14.01 ± 1.1 | 0.62 |
| Over 40 | 17.26 ± 0.75 | 0.001 |
Abbreviation: SE, standard error.
5. Discussion
The first way to identify an infertile couple's fertility status and follow an appropriate treatment method is to analyze semen in men. The World Health Organization has also provided the necessary training in this regard (18). The most common parameters to assess male reproductive health are sperm concentration, volume, and motility in semen (19). The present study showed that measuring sperm volume, concentration, and motility provides valuable information for diagnosing male infertility. This study found that all three factors were much lower in infertile men than in fertile men. In this regard, Esteves et al. stated that infertile men could be identified by examining the parameters of semen concentration and motility (20). Berling and Wolner-Hanssen reported that sperm concentration and motility were lower in infertile men than in fertile men (21). Sheikh et al. showed a significant relationship between semen fluid parameters and infertility (22).
The results of the present study were very close to the results of the survey by Najafipour et al. in which semen concentration was 120 × 106/mL, with a volume of 3.2 mL, in fertile individuals and 13 × 106/mL, with a volume of 2.9 mL, in infertile individuals (23). In this study, the concentration was 124 × 106/mL, with a volume of 3.8 mL, in fertile individuals and 20 × 106/mL, with a volume of 2 mL, in infertile individuals. Barekat et al. showed that sperm parameters such as concentration, motility, and normal morphology were lower in men with infertility than in fertile individuals, and the percentage of sperm with abnormal morphology was higher in them than in fertile individuals (24).
In the present study, the percentage of sperm with abnormal morphology was higher in men over 40 than in men under 40. Pino et al. reported that the risk of sperm damage increases with age while semen parameters decline (25). Silea et al. stated sperm volume and motility decreased in infertile men over 40 compared to younger men (26). In the study of Kumar et al., the volume of semen fluid in men over 40 was 2.4 mL (27), and in the study of Omran et al., men over 40 had a volume of 2 mL and a concentration of 19.4 × 106/mL (28).
Babu et al. reported that increasing FSH increases the risk of destruction of seminal vesicles, resulting in decreased sperm count and infertility (29). Khalil Ismael et al. stated that the measurement of FSH and LH is necessary to evaluate male infertility (30). In the present study, FSH and LH hormones were higher in infertile men than in fertile men. In recent decades, in addition to assessing sperm quality through basic testing, molecular and genetic studies have been conducted with the hope that further research will open up new avenues for treating infertility in men.
One of the most common tests is checking for sperm DNA damage (31). Sperms with single-stranded DNA are less fertile than sperms with double-stranded DNA. So, DNA damage is one of the causes of infertility (32). Janati Far et al. showed that essential sperm parameters such as sperm concentration, motility, and morphology were lower in infertile individuals than in fertile individuals, while sperm DNA damage was greater, which could ultimately affect fertility success. The present study confirms the studies of other researchers (33). Busetto et al. reported that sperm DNA damage was greater in older people than in younger men (34). Gunes et al. stated that because male gametes are constantly proliferating and dividing, the risk of mutations in DNA in these cells increases at older ages (35). In the present study, sperm DNA damage was more common in men over 40 than in men under 40. In this study, in infertile individuals, there was a significant negative relationship between sperm motility and DNA damage. Plastira et al. showed that reduced density and DNA damage harmed sperm motility (36).
5.1. Conclusions
The present study showed that sperm parameters such as sperm concentration, motility, and volume are much higher in fertile men than in infertile men, and sperm DNA damage, FSH, and LH hormones were greater in infertile people than in fertile people. There was a significant relationship between age and these parameters so the lowest volume, concentration, and motility and the highest rate of sperm DNA damage were observed in infertile men over 40 years.