1. Background
Dissociative symptoms can be explained as the uncoupling of consciousness (1). This phenomenon is also characterized as an interruption in the integrated functions of perception, consciousness, identity, or memory in the diagnostic and statistical manual of mental disorders fifth edition (DSM5) (2). Dissociative symptoms have been reported to result from issues such as dissociative disorders (3), childhood physical and sexual abuse (4, 5), and substance use (6-9). Unfortunately, there is limited knowledge on the relationship between methamphetamine use and dissociative symptoms, and only a few studies have been conducted on this issue (10, 11). For example, it has been documented that 3,4-methylenedioxymethamphetamine (MDMA) can produce dissociative symptoms resembling dissociative pathology (8).
It is usually presumed that substance use is a major cause of the manifestations of dissociative symptoms, and the users may really look for chemical dissociation to disconnect themselves from reality (7). Researchers have demonstrated that dissociative symptoms can elevate sleep loss or deprivation, stimulating the sleep-dissociation model (12, 13). This model anticipates that substances (e.g., cannabis) elevating sedative sleepiness are more likely to induce dissociative symptoms than stimulant drugs (e.g., MDMA), increasing wakefulness. Furthermore, the hypothesis of chemical dissociation (7) foresees that the dissociative properties of both sedatives and psycho-stimulants are substantial as long as they induce experiences assisting the people to disconnect themselves from reality.
Among substances, methamphetamine as a structural analog of amphetamine and a potent stimulant of the central nervous system is mainly used as a recreational drug and less commonly as a second-line treatment for attention deficit hyperactivity disorder (ADHD) (14). Previous research has revealed a swift increment in the number of methamphetamine users since the late 1980s (15). Due to the mental symptoms associated with methamphetamine and amphetamine intoxication, they have been increasingly used among people with psychological and psychiatric disorders. Nakatani and Hara (16) proposed that the perturbation of consciousness may occasionally happen during the intoxication period with methamphetamine and amphetamine, albeit these symptoms can be neglected easily due to confusing symptomatology (16).
2. Objectives
As mentioned above, research on substance-induced dissociation is an important topic in the fields of psychiatry and psychology among substance users, because the obtained results may shed light on the mechanisms involved in dissociative psychopathology and help to alleviate dissociative symptoms in these people. Thus, for achieving this goal, the present study was done to investigate the prevalence of dissociative experiences and dissociative disorders in methamphetamine users in Shahid Beheshti hospital of Kerman City, Kerman Province, Iran. The reason to conduct our study on hospitalized patients was to reach the patients with more severe disorders such as dissociative disorders, which have not been studied in previous studies.
3. Methods
3.1. Study Design
In this descriptive cross-sectional study, two groups of subjects, including methamphetamine users and well-matched controls, were randomly selected from the individuals referring to the Shahid-Beheshti Hospital in Kerman City using a simple random sampling method from September 2016 to March 2018. A total of 50 methamphetamine users were included in the study, whose diagnosis was validated via the methamphetamine positive-urine test. A total of 51 controls (well-matched with substance users regarding age, gender, and education status) were selected from the patient's relatives who had no physiological disorders. The physiological status of these controls was confirmed by an experienced psychiatrist. Exclusion criteria included having other psychotic disorders, except for methamphetamine-induced psychosis, mental retardation, and cannabis, alcohol, or benzodiazepine use history. Only a previous history of opium use was reported in 42 individuals in the case group and five individuals in the control group, but their urine test was negative at the time of the study. In the following, the objectives of the research were explained to the participants, and written informed consent was obtained from all of them. Finally, the Dissociative Experiences Scale (DES), dissociative disorders interview schedule-DSM-5 (DDIS), and Positive and Negative Syndrome Scale (PANSS) were employed to collect data by a trained psychiatrist.
The DDIS is a highly structured interview, which helps in DSM-5 diagnosis of somatization disorder, borderline personality disorder, and major depressive disorder, as well as all the dissociative disorders. It inquires about positive symptoms of schizophrenia, secondary features of Dissociative Identity Disorder (DID), substance use, other items relevant to dissociative disorders (17) and trances, sleepwalking, possession, childhood abuse, childhood companions, supernatural/extrasensory perception experiences, and participation in cults. This questionnaire contains 132 questions (2).
The DES is a highly reliable and valid test for the screening of dissociative experiences (18). This test contains 28 questions covering three subscales, reflecting the constructs of dissociative symptoms: depersonalization/derealization, amnesia, and absorption. It requires the participants to indicate that to what extent they experience 28 dissociative experiences in their daily life on a 100-mm visual analog scale (anchors: 0 = never; 100 = always).
The PANSS is a 30-item scale, in which each item is rated on a seven-point Likert scale (ranging from normal to extremely abnormal) with sub-scores for seven positive (P), seven negative (N), and 16 global psychopathological symptoms (19).
3.2. Data Analysis
The data obtained from the questionnaires were described by descriptive statistical measures (mean and standard deviation). The chi-square test and t test were applied for comparing the study groups, and also Pearson's correlation coefficient was used for determining the relationship between DES and PANSS scores in methamphetamine users using SPSS version 20 software. A P value of < 0.05 was considered statistically significant.
3.3. Ethical Considerations
For observing the ethical considerations, all the procedures were carried out following the Declaration of Helsinki, and the research was approved by the Ethics Committee of the Kerman University of Medical Sciences (code No. IR. KER.REC.1397.450). Besides, written informed consent was obtained from all the subjects to participate in the research.
4. Results
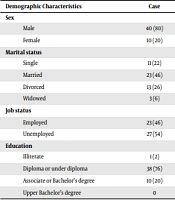
For determining the prevalence of dissociative experiences in methamphetamine users, the two groups, including methamphetamine users and controls, were studied by DES, DDIS, and PANSS. The results obtained from the demographic questionnaire showed that the mean age of the case and control groups was 37.7 ± 8 and 30.4 ± 7.5 years, respectively, and the two groups were similar in terms of sex, education level, history of sexual abuse, physical abuse, psychotherapy, somatic symptom disorder, borderline personality disorder, and history of participation in different cults (Tables 1 and 2). It should be noted that the non-significant difference in sexual abuse between the control and case groups was probably due to the Iranian cultural conditions so that participants somehow avoid answering this question. Although the control group was not required to study the prevalence, it was decided to use the control group, which was matched with the case group in many ways, in order to evaluate the significance of the results as a starting point for the current study.
| Demographic Characteristics | Case | Control | P Value |
|---|---|---|---|
| Sex | 0.762 | ||
| Male | 40 (80) | 42 (82.4) | |
| Female | 10 (20) | 9 (17.6) | |
| Marital status | 0.007 | ||
| Single | 11 (22) | 12 (23.5) | |
| Married | 23 (46) | 36 (70.6) | |
| Divorced | 13 (26) | 3 (5.9) | |
| Widowed | 3 (6) | 0 | |
| Job status | 0.00 | ||
| Employed | 23 (46) | 51 (100) | |
| Unemployed | 27 (54) | 0 | |
| Education | 0.703 | ||
| Illiterate | 1 (2) | 0 | |
| Diploma or under diploma | 38 (76) | 42 (82.4) | |
| Associate or Bachelor’s degree | 10 (20) | 8 (15.7) | |
| Upper Bachelor’s degree | 0 | 1 (2) |
a Values re expressed as No. (%).
| Characteristics | Frequency | P Value | |
|---|---|---|---|
| Case | Control | ||
| Sexual Abuse | 0.06 | ||
| Yes | 10 | 4 | |
| No | 38 | 47 | |
| Physical Abuse | 0.07 | ||
| Yes | 19 | 11 | |
| History of Psychotherapy | 0.09 | ||
| No | 31 | 40 | |
| Yes | 4 | 46 | |
| No | 3 | 48 | |
| Borderline Personality Disorder | 0.17 | ||
| Yes | 11 | 6 | |
| No | 39 | 45 | |
| Cult Participation History | 0.59 | ||
| Yes | 6 | 8 | |
| Somatic symptom Disorder (DSM5) | 0.9 | ||
| No | 12 | 43 | |
| Yes | 31 | 31 | |
| No | 19 | 20 | |
The mean scores of DES in the case and control groups were 15.3 and 14.32, respectively. Among different items of DES, the case group only had higher scores on the depersonalization/derealization item (P < 0.01) (Table 3). The mean scores of PANSS in the case and control groups were 57 and 35, respectively. The mean scores of all PANSS subscales were higher in the case group than in the control group (P < 0.01) (Table 3).
| Characteristics | Case | Control | t-Test | Df | P Value |
|---|---|---|---|---|---|
| DES Subscales | |||||
| Amnesia | 11.93 | 11.39 | 0.188 | 96 | 0.851 |
| Depersonalization/derealization | 11.15 | 4.82 | 2.673 | 96 | 0.009 a |
| Absorption | 21.85 | 21.36 | 0.131 | 96 | 0.493 |
| Total DES | 15.3 | 14.32 | 0.341 | 96 | 0.734 |
| PANSS Subscales | |||||
| Positive symptoms | 13.58 | 7.07 | 6.3 | 99 | 0.00 a |
| Negative symptoms | 11.06 | 7.13 | 4.84 | 99 | 0.00 a |
| Total PANSS | 57 | 35 | 7.64 | 99 | 0.00 a |
| General psychopathology | 26.96 | 17.5 | 7.52 | 99 | 0.00 a |
| Anger Scale | 5.48 | 3.58 | 5.74 | 99 | 0.00 a |
a P < 0.01 is significant.
According to the results obtained from the DDIS, 36% of the methamphetamine users were diagnosed with the dissociative disorder (P < 0.01), 4% with dissociative amnesia (P > 0.05), 2% with a dissociative fugue (P > 0.05), 6% with depersonalization/derealization disorder (P > 0.05), 8% with DID (P < 0.05), and 24% with other specified dissociative disorders (P < 0.01) (Table 4). Thus, dissociative disorder accounted for the highest frequency among methamphetamine users, followed by other specified dissociative disorders and DID. The experiences of possession were present in 17 methamphetamine users and three control group members (P < 0.01).
| DDIS Items | Case Group | Control Group | χ2 Test | df | P Value |
|---|---|---|---|---|---|
| Dissociative amnesia | 2 (4) | 1 (2) | 2.08 | 1 | 0.149 |
| Dissociative fugue | 1 (2) | 0 | 1.03 | 1 | 0.31 |
| Depersonalization/derealization disorder | 3 (6) | 1 (2) | 1.08 | 1 | 0.298 |
| Dissociative identity disorder | 4 (8) | 0 | 4.25 | 1 | 0.0039 b |
| Other specified dissociative disorders | 12 (24) | 0 | 13.89 | 1 | 0.00 b |
| Total dissociative disorders | 18 (36) | 1 (2) | 19.15 | 1 | 0.00 b |
| Possession experience | 17 (34) | 3 (5.8) | 12.57 | 1 | 0.00 b |
a Values re expressed as No. (%).
b P < 0.01 is significant.
The results of correlation analysis revealed a significant positive relationship (r = 0.24) between positive symptoms (based on PANSS) and dissociative experiences (based on DES) (P < 0.05), as described by Spitzer et al. (20) and Ghoreishi and Shajari (21).
5. Discussion
In this study, the mean score of DES in the case group was determined as 15.3, which was lower than those reported in the studies by Somer and Avni (22) and Karadag et al. (23). Among different dissociative experiences, the frequency of the depersonalization/derealization subscale of DES was much higher in the case group that is consistent with the study by van Heugten-van der Kloet et al. (8), who demonstrated that MDMA consumption increased depersonalization/derealization experience. Kianpoor et al. (24) also displayed that this experience was more frequent in opioid users.
According to the results obtained from the DDIS, it was found that methamphetamine can induce dissociative disorders, such as DID and other specified dissociative disorders. According to the DSM5 criteria, other specified dissociative disorders are as follows: (1) atypical presentations not meeting the full diagnostic criteria for DID: this group is similar to the people with DID but with (a) less-than-marked discontinuities of self and agency, and/or (b) alterations in identity or episodes of pathological possession along with reporting no dissociative amnesia; (2) coercive persuasion; (3) acute dissociative reaction to stressful events; and (4) dissociative trance disorder (25). In our research, all of our patients were categorized into the first group. The DID has two subgroups: (1) possession, and (2) non-possession (25); the first subgroup was the leading factor in all of our patients with dissociative disorders. From Jung’s point of view, the induction of possession occurs when archetypal images are not made consciously; if there is already a predisposition to psychosis, it may even happen that the archetypal figures, endowed with a certain autonomy anyway on account of their natural numinosity, will escape from conscious control altogether and become completely independent, thus developing the phenomenon of possession (26).
In more recent studies, it has also been shown that MDMA significantly reduces activation in the medial prefrontal cortex and left insula (27), suggesting a critical role for the insula, particularly the anterior division, in high-level cognitive control and attentional processes. Importantly, the anterior insula can be introduced as an integral hub in mediating dynamic interactions between other large-scale brain networks involved in externally oriented attention and internally oriented or self-related attention (28). Thus, the following question can be raised: (1) do these parts stop acting properly; and (2) does internally oriented attention start and make archetypes appear while using methamphetamine? Therefore, it is suggested that future studies be conducted to answer this question. Due to the lack of sufficient studies about the prevalence of dissociative disorders in methamphetamine users, some of the above were the hypotheses to justify the results of our study.
In addition, in our study, the mean scores of all PANSS subscales were higher in the case group than in the control group, which can reflect a schizophrenic state in methamphetamine users. Results of correlation analysis revealed a significant positive relationship between the PANSS and DES scores, meaning that positive symptoms are related to dissociative experiences, which is consistent with the previous findings discovering the relationship between dissociative experiences and psychosis (21, 29).
In total, our findings confirmed the prevalence of dissociative symptoms in methamphetamine users, as described in other previous studies. For instance, Seedat et al. (30) studied the relationship between substance use and dissociation in 1,007 adults in Memphis, Tennessee, USA. Their results showed that dissociative symptoms were significantly associated with harmful alcohol use. Kianpoor et al. (24) also studied the relationship between substance use and dissociation in 116 prisoners with and without opioid dependence disorder in Iran. Their results proposed a relation between dissociation and addiction.
Finally, it should be mentioned that the low sample size and mere selection of hospitalized patients were the limitations of this study. Besides, the authors had access to individuals with more severe symptoms to be able to assess dissociative disorders in addition to dissociative experiences, but the dose and duration of methamphetamine use were not considered in this study. As the patient could not declare how much methamphetamine was used exactly, performing a prospective cohort study is recommended.
5.1. Conclusion
Our findings indicated that unconscious contents can be brought into conscious awareness by focusing attention through methamphetamine use like active imagination process, meaning that methamphetamine use improves attention and the patients cannot control this process consciously. In this situation, possession or some other dissociative disorders may appear. In other words, it can be concluded that methamphetamine induces the development of dissociative psychosis.